J Rheum Dis.
2016 Oct;23(5):311-315. 10.4078/jrd.2016.23.5.311.
Tuberculous Osteomyelitis of the First Metatarsophalangeal Joint Misdiagnosed as Gouty Arthritis
- Affiliations
-
- 1Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea. kiwonmoon@kangwon.ac.kr
- 2Department of Pathology, Kangwon National University School of Medicine, Chuncheon, Korea.
- KMID: 2356486
- DOI: http://doi.org/10.4078/jrd.2016.23.5.311
Abstract
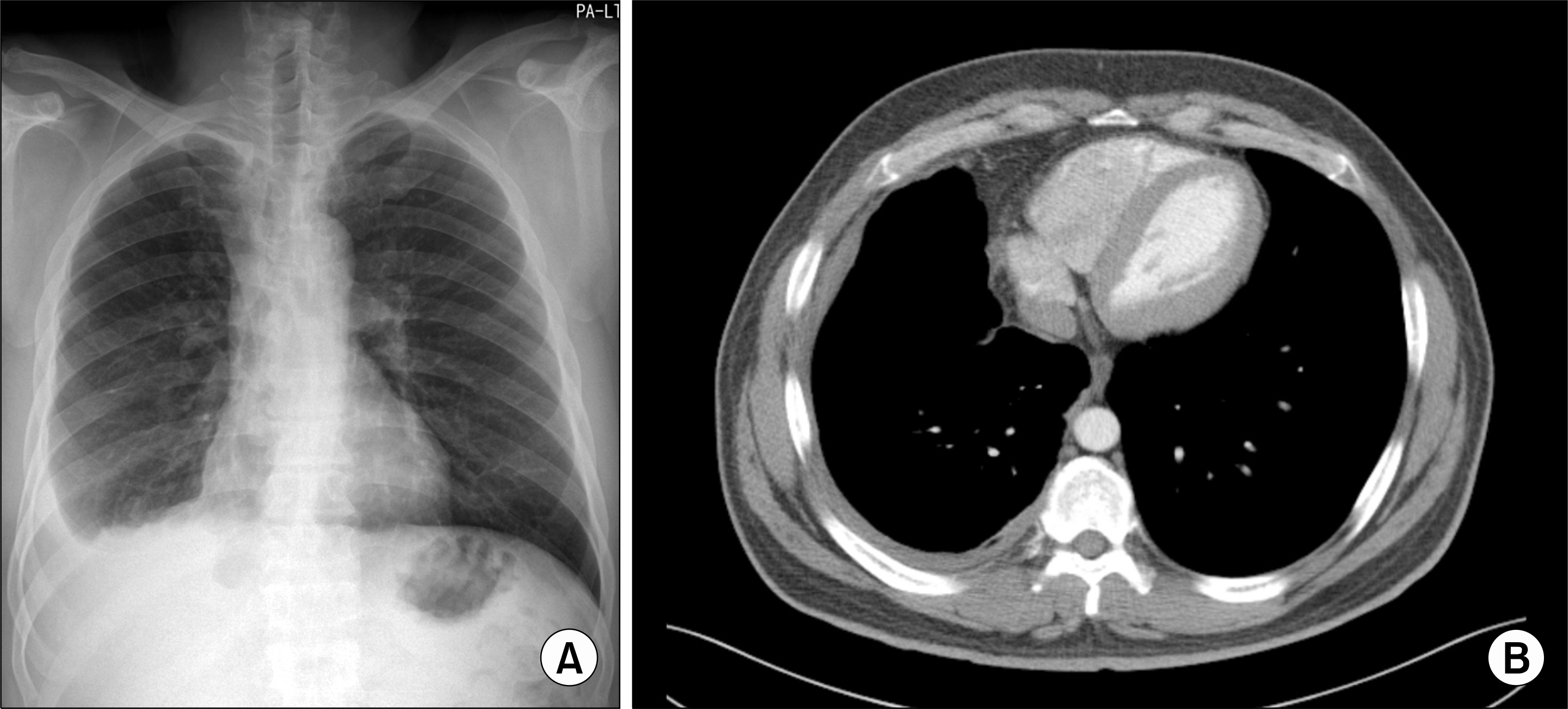
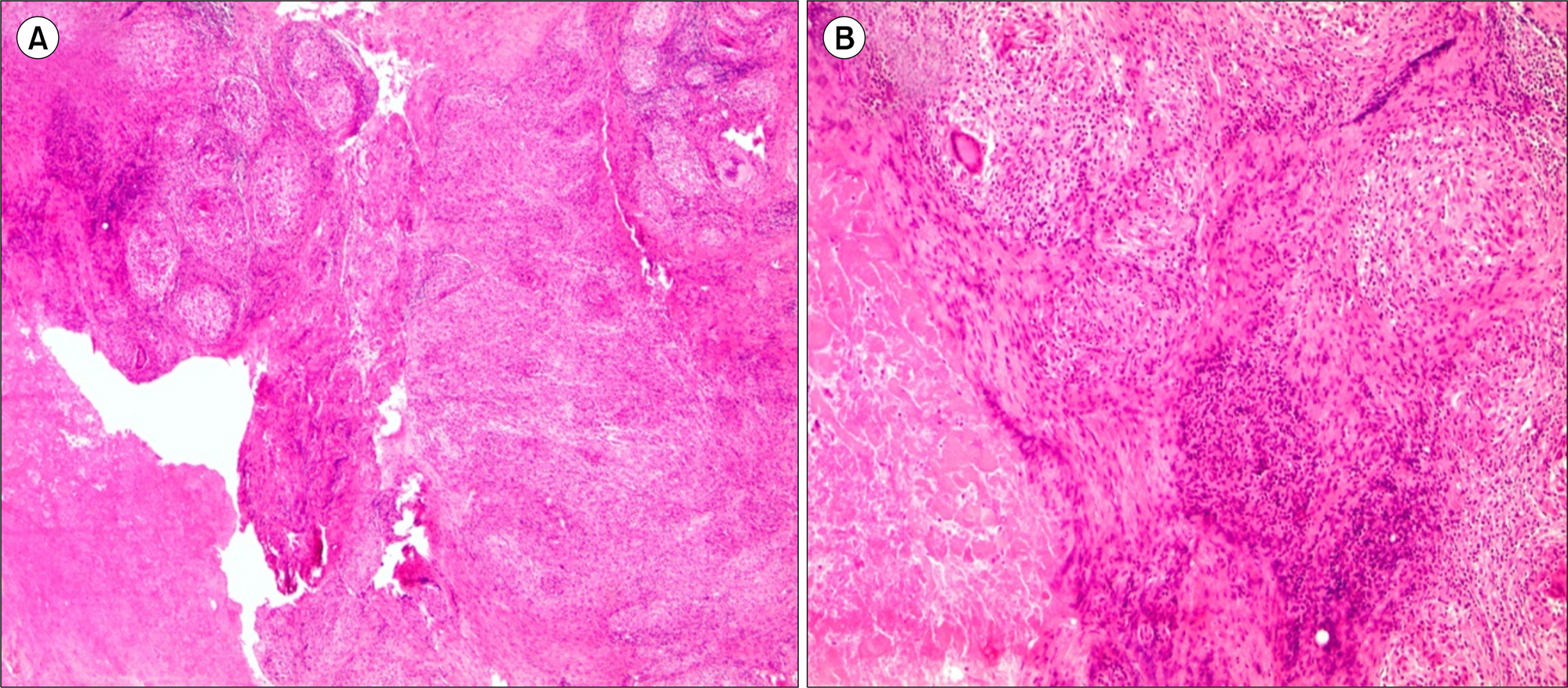
- A-43-year-old man visited our clinic due to pain and swelling of his left first metatarsophalangeal (MTP) joint since 6-months ago. He was diagnosed as gouty arthritis at private clinic and took hypouricemic agent, but he had progressive pain and swelling. There was swelling, erythema and tenderness and ulceration at base of the left first MTP joint. His laboratory results showed elevated C-reactive protein and normal serum uric acid level. The plain radiograph of foot showed bone destruction of left first MTP joint. MRI revealed joint space narrowing, soft tissue swelling and subchondral cyst. He underwent excisional biopsy and histology demonstrated chronic granulomatous inflammation with caseation necrosis. Tissue polymerase chain reaction for mycobacterium tuberculosis was positive. He was diagnosed as tuberculous osteomyelitis. He started on quadruple anti-tuberculous therapy and his symptom was improved. Early diagnosis and anti-tuberculosis therapy could lead to improve outcomes.
Keyword
MeSH Terms
Figure
Reference
-
1. Korim M, Patel R, Allen P, Mangwani J. Foot and ankle tuberculosis: case series and literature review. Foot (Edinb). 2014; 24:176–9.
Article2. Samuel S, Boopalan PR, Alexander M, Ismavel R, Varghese VD, Mathai T. Tuberculosis of and around the ankle. J Foot Ankle Surg. 2011; 50:466–72.
Article3. Mittal R, Gupta V, Rastogi S. Tuberculosis of the foot. J Bone Joint Surg Br. 1999; 81:997–1000.
Article4. Gursu S, Yildirim T, Ucpinar H, Sofu H, Camurcu Y, Sahin V, et al. Long-term follow-up results of foot and ankle tuberculosis in Turkey. J Foot Ankle Surg. 2014; 53:557–61.
Article5. Choi JS, Gwak HC, Kim JH, Chung HJ. Tuberculosis in foot and ankle. J Korean Foot Ankle Soc. 2008; 12:203–9.6. Choi JS, Gwak HC, Kim JH, Lee CR. Tuberculous osteomyelitis of the tarsal bone in an infant: case report. J Korean Orthop Assoc. 2009; 44:275–8.7. Nayak B, Dash RR, Mohapatra KC, Panda G. Ankle and foot tuberculosis: a diagnostic dilemma. J Family Med Prim Care. 2014; 3:129–31.
Article8. Chevannes W, Memarzadeh A, Pasapula C. Isolated tuberculous osteomyelitis of the talonavicular joint without pulmonary involvement-a rare case report. Foot (Edinb). 2015; 25:66–8.
Article9. Golden MP, Vikram HR. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005; 72:1761–8.10. Parmar H, Shah J, Patkar D, Singrakhia M, Patankar T, Hutchinson C. Tuberculous arthritis of the appendicular skeleton: MR imaging appearances. Eur J Radiol. 2004; 52:300–9.
Article11. Tsai YJ, Shiau YC. Diagnosis and monitoring treatment response of skeletal tuberculosis of foot by three-phase bone scan: a case report. Ann Nucl Med Sci. 2010; 23:175–80.12. Hong L, Wu JG, Ding JG, Wang XY, Zheng MH, Fu RQ, et al. Multifocal skeletal tuberculosis: experience in diagnosis and treatment. Med Mal Infect. 2010; 40:6–11.
Article13. Hsiao CH, Cheng A, Huang YT, Liao CH, Hsueh PR. Clinical and pathological characteristics of mycobacterial tenosynovitis and arthritis. Infection. 2013; 41:457–64.
Article14. Noussair L, Bert F, Leflon-Guibout V, Gayet N, NicolasChanoine MH. Early diagnosis of extrapulmonary tuberculosis by a new procedure combining broth culture and PCR. J Clin Microbiol. 2009; 47:1452–7.
Article15. Mehta PK, Raj A, Singh N, Khuller GK. Diagnosis of extrapulmonary tuberculosis by PCR. FEMS Immunol Med Microbiol. 2012; 66:20–36.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Gouty Arthritis Involving the Hip Joint Diagnosed Using Ultrasonography
- A Osteochondroma of Calcaneus with Gouty Arthritis of the Subtalar Joint (A Case Report)
- Surgical Treatment of Gouty Tophi in Bilateral Popliteal Cysts
- Acute Gouty Arthritis Presented after Pyrazinamide Treatment in a Patient with Chronic Renal Insufficiency
- Clinical Guidelines for the Antimicrobial Treatment of Bone and Joint Infections in Korea