Intest Res.
2016 Oct;14(4):365-368. 10.5217/ir.2016.14.4.365.
Biologics for the treatment of pyoderma gangrenosum in ulcerative colitis
- Affiliations
-
- 1Department of Gastroenterology, GB Pant Hospital, New Delhi, India. amarender.puri@gmail.com
- KMID: 2354955
- DOI: http://doi.org/10.5217/ir.2016.14.4.365
Abstract
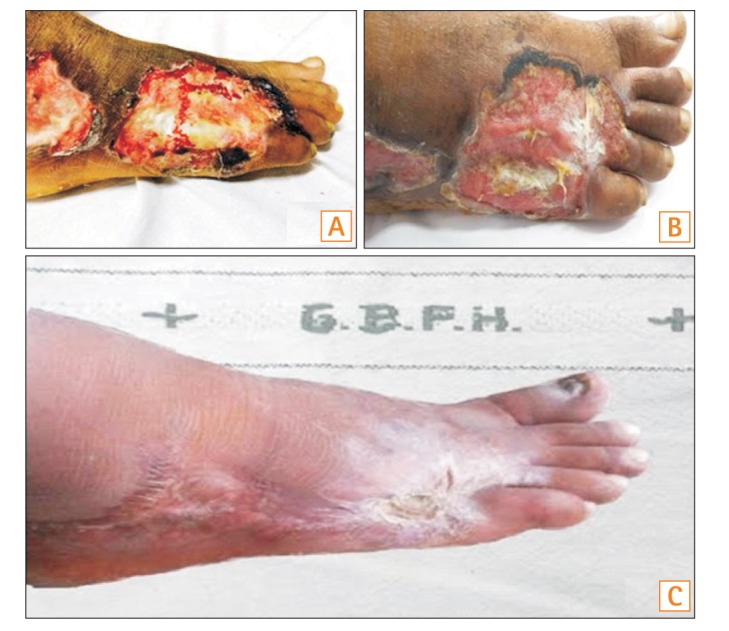
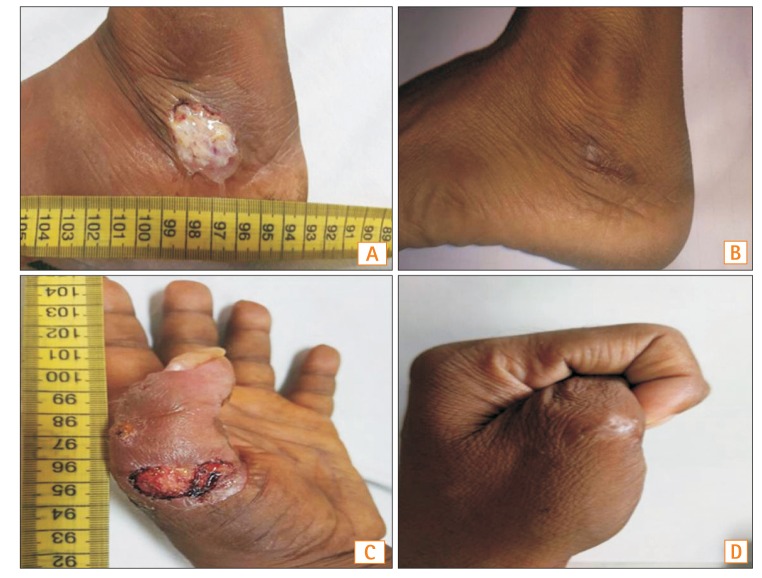
- Pyoderma gangrenosum (PG) is an uncommon extra-intestinal manifestation of inflammatory bowel disease (IBD). Despite limited published literature, biologics have caused a paradigm shift in the management of this difficult-to-treat skin condition. The clinical data and outcomes of three patients with active ulcerative colitis and concurrent PG treated with biologics (infliximab two and adalimumab one) are reviewed in this report. Biologics were added because of the sub-optimal response of the colonic symptoms and skin lesions to parenteral hydrocortisone therapy. All three patients showed a dramatic response to the addition of the biologics. In view of the rapid healing of the skin lesions, superior response rate, and the additional benefit of improvement in the underlying colonic disease following treatment, anti-tumor necrosis factor blockers should be considered as a first line therapy in the management of PG with underlying IBD.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Multiple extraintestinal manifestations in a patient with acute severe ulcerative colitis: a case report
Eun Young Park, Dong Hoon Baek, Seung Min Hong, Geun Am Song
Kosin Med J. 2022;37(4):361-366. doi: 10.7180/kmj.22.027.Hyperbaric oxygen therapy for pyoderma gangrenosum associated with ulcerative colitis
Hyun Il Seo, Hyun-Ju Lee, Koon Hee Han
Intest Res. 2018;16(1):155-157. doi: 10.5217/ir.2018.16.1.155.
Reference
-
1. Menachem Y, Gotsman I. Clinical manifestations of pyoderma gangrenosum associated with inflammatory bowel disease. Isr Med Assoc J. 2004; 6:88–90. PMID: 14986464.2. Rothfuss KS, Stange EF, Herrlinger KR. Extraintestinal manifestations and complications in inflammatory bowel diseases. World J Gastroenterol. 2006; 12:4819–4831. PMID: 16937463.
Article3. Chow RK, Ho VC. Treatment of pyoderma gangrenosum. J Am Acad Dermatol. 1996; 34:1047–1060. PMID: 8647970.
Article4. Brooklyn T, Dunnill G, Probert C. Diagnosis and treatment of pyoderma gangrenosum. BMJ. 2006; 333:181–184. PMID: 16858047.
Article5. Brooklyn TN, Dunnill MG, Shetty A, et al. Infliximab for the treatment of pyoderma gangrenosum: a randomised, double blind, placebo controlled trial. Gut. 2006; 55:505–509. PMID: 16188920.
Article6. Regueiro M, Valentine J, Plevy S, Fleisher MR, Lichtenstein GR. Infliximab for treatment of pyoderma gangrenosum associated with inflammatory bowel disease. Am J Gastroenterol. 2003; 98:1821–1826. PMID: 12907338.
Article7. Agarwal A, Andrews JM. Systematic review: IBD-associated pyoderma gangrenosum in the biologic era, the response to therapy. Aliment Pharmacol Ther. 2013; 38:563–572. PMID: 23914999.
Article8. Hayashi H, Kuwabara C, Tarumi K, Makino E, Fujimoto W. Successful treatment with infliximab for refractory pyoderma gangrenosum associated with inflammatory bowel disease. J Dermatol. 2012; 39:576–578. PMID: 21958000.
Article9. Ueda M, Katoh M, Tanizaki H, Tanioka M, Matsumura Y, Miyachi Y. Refractory pyoderma gangrenosum associated with ulcerative colitis successfully treated with infliximab. Dermatol Online J. 2012; 18:12.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Post-traumatic Pyoderma Gangrenosum Associated with Ulcerative Colitis
- A Case of Pyoderma Gangrenosum Associated with Ulcerative Colitis
- Multiple Pyoderma Gangrenosum in Ulcerative Colitis
- A Case of Simultaneous Presentation of Bullous and Ulcerative Types of Pyoderma Gangrenosum in an Ulcerative Colitis Patient
- Pyoderma Gangrenosum in a Patient with Ulcerative Colitis: A Case Report