J Korean Foot Ankle Soc.
2016 Sep;20(3):121-125. 10.14193/jkfas.2016.20.3.121.
The Amputation Rate and Associated Risk Factors within 1 Year after the Diagnosis of Diabetic Foot Ulcer
- Affiliations
-
- 1Department of Orthopaedic Surgery, Soonchunhyang University Seoul Hospital, Seoul, Korea. orthowon@gmail.com
- KMID: 2351417
- DOI: http://doi.org/10.14193/jkfas.2016.20.3.121
Abstract
- PURPOSE
This study investigates the amputation rate within 1 year after the diagnosis of diabetic foot ulcer and its associated risk factors.
MATERIALS AND METHODS
This study enrolled 60 patients with diabetic foot ulcer. The mean and standard deviation age was 64.4±12.8 years (range, 32~89 years); the mean and standard deviation prevalence period for diabetes mellitus was 21.0±7.5 years (range, 0.5~36 years). The amputation rate was evaluated by dividing the subjects into two groups"”the major and minor amputation groups"”within 1 year following the initial diagnosis of diabetic foot ulcer. Multivariate Cox proportional hazards regression analysis was used to identify the risk factors for amputation.
RESULTS
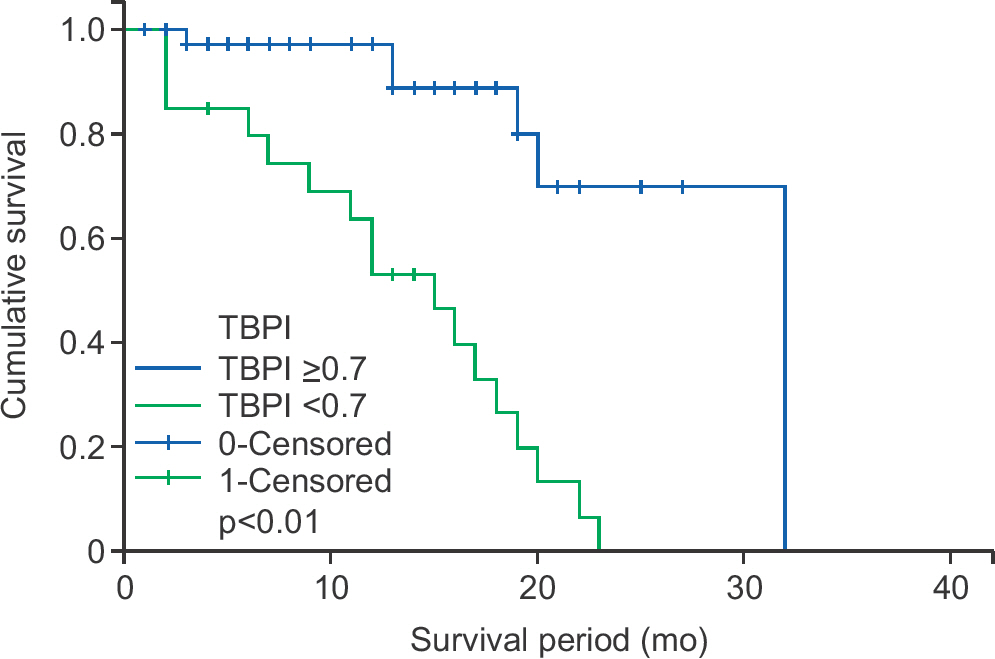
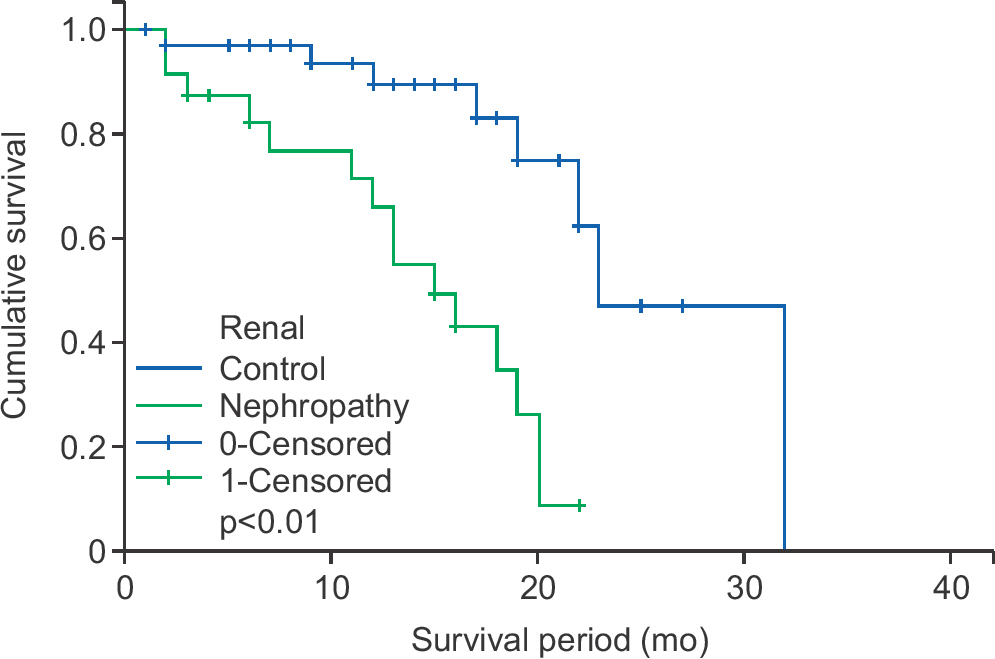
The total amputation rate of 38.3% (n=23) was comprised of the amputation rate for the major amputation group (10.0%) and rate for the minor amputation group (23.8%). There was a high correlation between peripheral artery disease (toe brachial pressure index <0.7) and amputation (hazard ratio [HR] 5.81, confidence interval [CI] 2.09~16.1, p<0.01). Nephropathy was significantly correlated with the amputation rate (HR 3.53, CI 1.29~9.64, p=0.01).
CONCLUSION
Clinicians who treat patients with diabetic foot complications must understand the fact that the amputation rate within 1 year is significant, and that the amputation rate of patients with peripheral artery disease or nephropathy is especially high.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Risk Factors for the Treatment Failure of Antibiotic-Loaded Cement Spacer Insertion in Diabetic Foot Infection
Se-Jin Park, Seungcheol Song
J Korean Foot Ankle Soc. 2019;23(2):58-66. doi: 10.14193/jkfas.2019.23.2.58.
Reference
-
1.Boulton AJ. The pathway to foot ulceration in diabetes. Med Clin North Am. 2013. 97:775–90.
Article2.Singh N., Armstrong DG., Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005. 293:217–28.
Article3.Stiegler H. Das diabetische Fußsyndrom [Diabetic foot syndrome]. Herz. 2004. 29:104–15. German.4.Gregg EW., Sorlie P., Paulose-Ram R., Gu Q., Eberhardt MS., Wolz M, et al. Prevalence of lower-extremity disease in the US adult population >=42 years of age with and without diabetes: 1999-2000 national health and nutrition examination survey. Diabetes Care. 2004. 27:1591–7.5.Winkley K., Stahl D., Chalder T., Edmonds ME., Ismail K. Risk factors associated with adverse outcomes in a population-based prospective cohort study of people with their first diabetic foot ulcer. J Diabetes Complications. 2007. 21:341–9.
Article6.Morbach S., Furchert H., Gröblinghoff U., Hoffmeier H., Kersten K., Klauke GT, et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a de-cade. Diabetes Care. 2012. 35:2021–7.
Article7.Won SH., Chung CY., Park MS., Lee T., Sung KH., Lee SY, et al. Risk factors associated with amputation-free survival in patient with diabetic foot ulcers. Yonsei Med J. 2014. 55:1373–8.
Article8.Faglia E., Clerici G., Caminiti M., Curci V., Somalvico F. Prognostic difference between soft tissue abscess and osteomyelitis of the foot in patients with diabetes: data from a consecutive series of 452 hospitalized patients. J Foot Ankle Surg. 2012. 51:34–8.
Article9.Beks PJ., Mackaay AJ., de Neeling JN., de Vries H., Bouter LM., Heine RJ. Peripheral arterial disease in relation to glycaemic level in an elderly Caucasian population: the Hoorn study. Diabetologia. 1995. 38:86–96.
Article10.Høyer C., Sandermann J., Petersen LJ. The toe-brachial index in the diagnosis of peripheral arterial disease. J Vasc Surg. 2013. 58:231–8.
Article11.Sharp CS., Bessman AN., Wagner FW Jr., Garland D. Microbiology of deep tissue in diabetic gangrene. Diabetes Care. 1978. 1:289–92.
Article12.Pscherer S., Dippel FW., Lauterbach S., Kostev K. Amputation rate and risk factors in type 2 patients with diabetic foot syndrome under real-life conditions in Germany. Prim Care Diabetes. 2012. 6:241–6.
Article13.Miyajima S., Shirai A., Yamamoto S., Okada N., Matsushita T. Risk factors for major limb amputations in diabetic foot gangrene patients. Diabetes Res Clin Pract. 2006. 71:272–9.
Article14.Kaminski M., Frescos N., Tucker S. Prevalence of risk factors for foot ulceration in patients with end-stage renal disease on hae-modialysis. Intern Med J1. 2012. 42:e120–8.
Article