Korean J Crit Care Med.
2016 May;31(2):123-128. 10.4266/kjccm.2016.31.2.123.
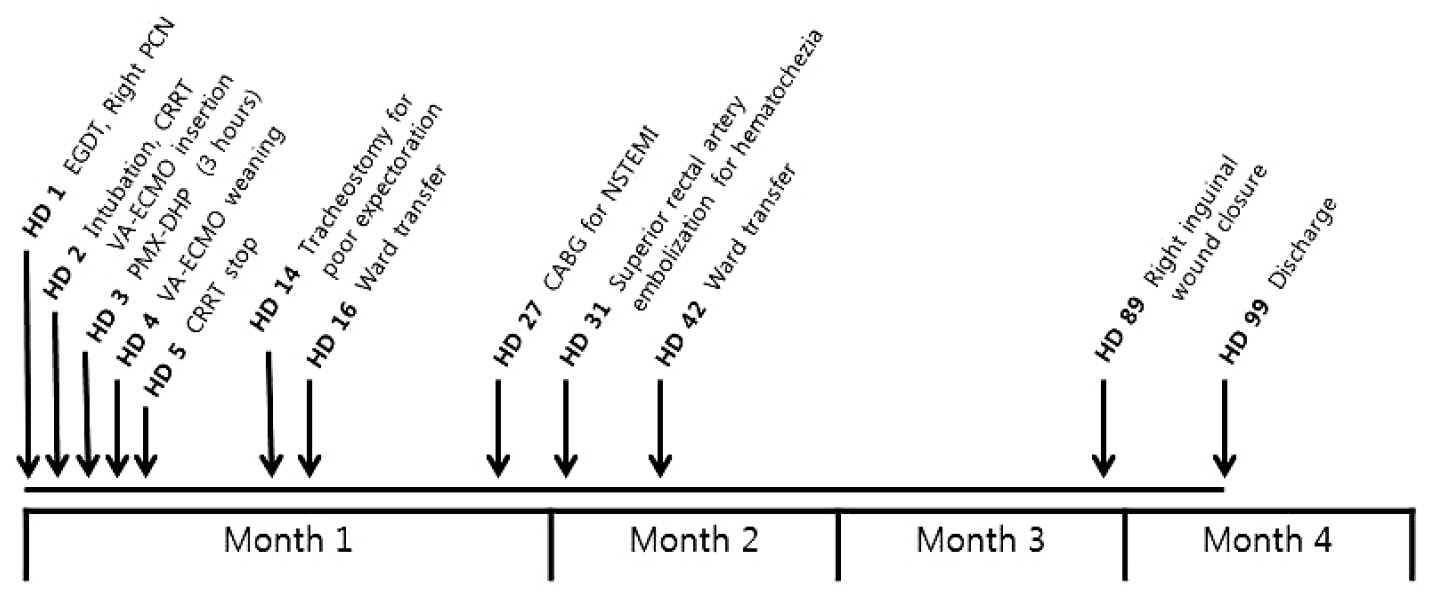
Use of Polymyxin B Hemoperfusion in a Patient with Septic Shock and Septic Cardiomyopathy Who Was Placed on Extracorporeal Membrane Oxygen Support
- Affiliations
-
- 1Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Division of Pulmonary and Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Critical Care Nursing Team, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 5Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ccrzzang@gmail.com
- KMID: 2350919
- DOI: http://doi.org/10.4266/kjccm.2016.31.2.123
Abstract
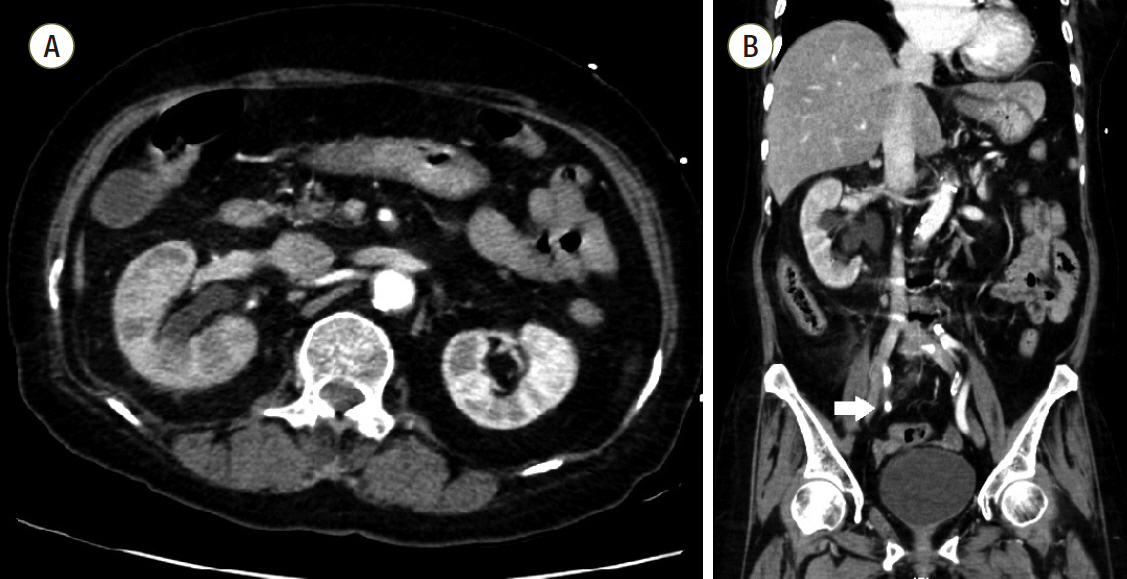
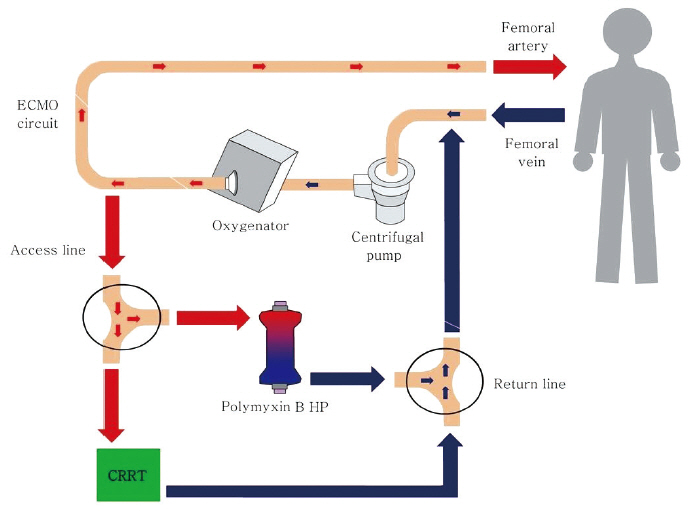
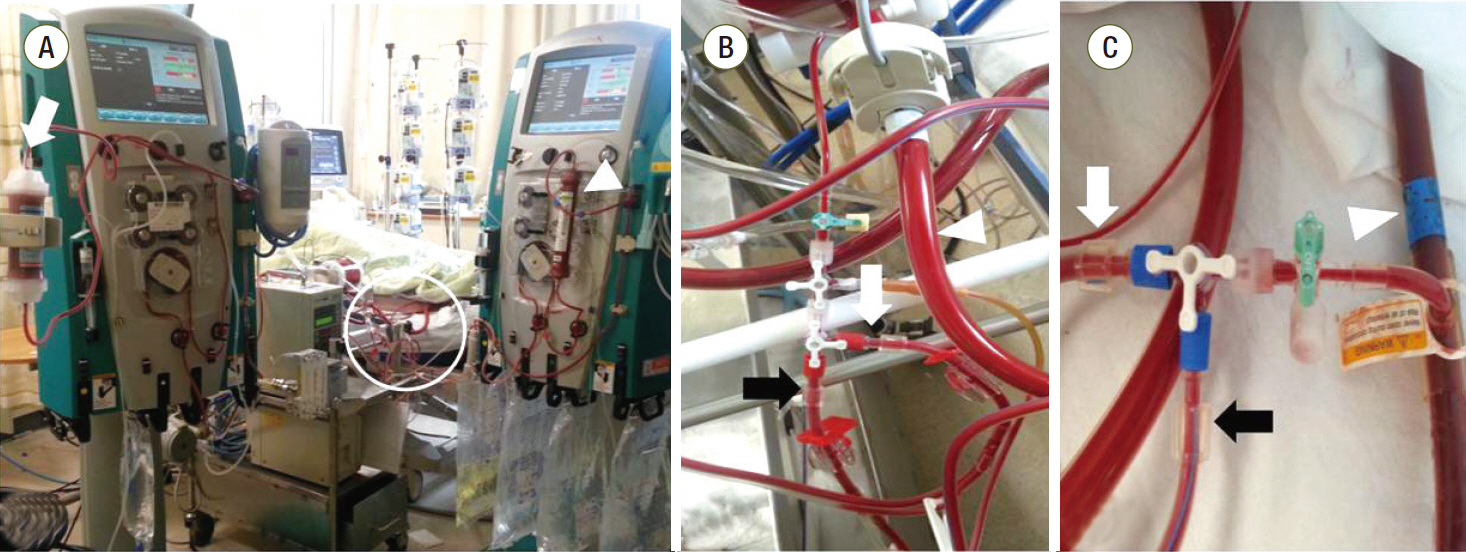
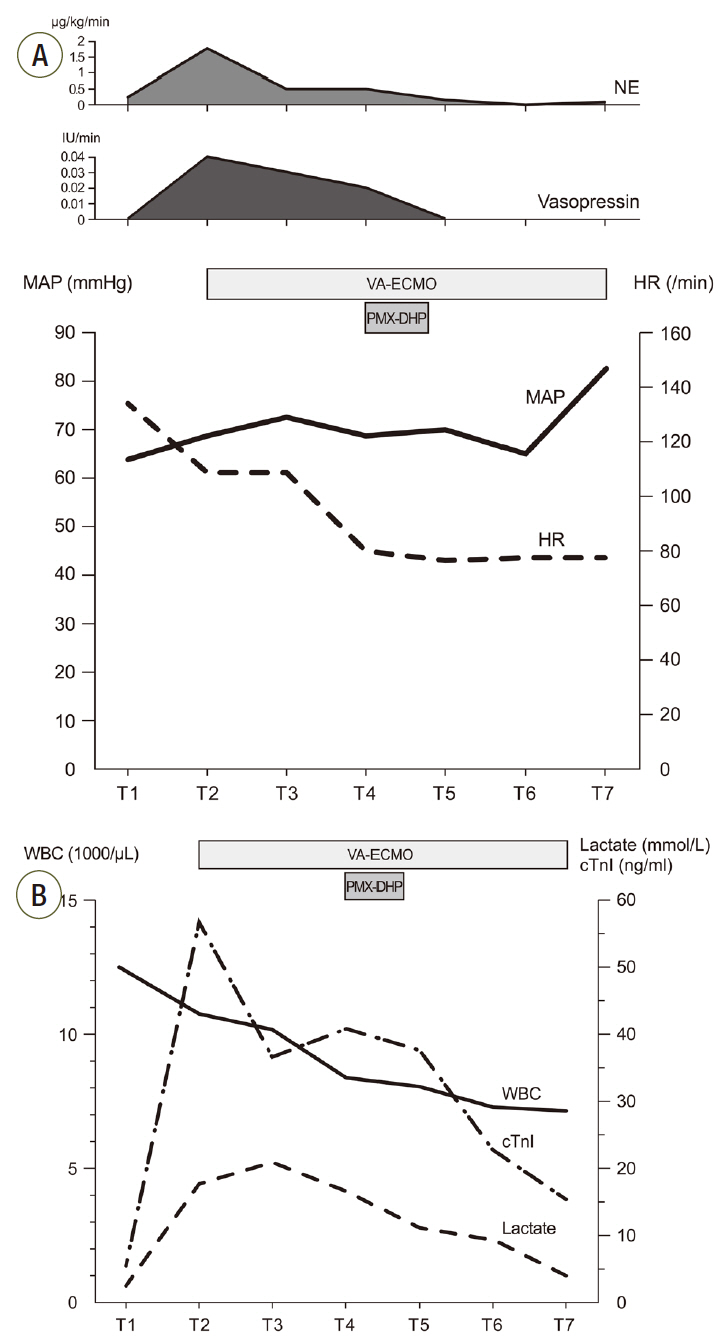
- Although shock in sepsis is usually managed successfully by conventional medical treatment, a subset of cases do not respond and may require salvage therapies such as veno-arterial extracorporeal membrane oxygenation (VA ECMO) support as well as an attempt to remove endotoxins. However, there are limited reports of attempts to remove endotoxins in patients with septic shock on VA ECMO support. We recently experienced a case of septic shock with severe myocardial injury whose hemodynamic improvement was unsatisfactory despite extracorporeal membrane oxygenation (ECMO) support. Since the cause of sepsis was acute pyelonephritis and blood cultures grew gram-negative bacilli, we additionally applied polymyxin B direct hemoperfusion (PMX-DHP) to the ECMO circuit and were able to successfully taper off vasopressors and wean off ECMO support. To the best of our knowledge, this is the first adult case in which PMX-DHP in addition to ECMO support was successfully utilized in a patient with septic shock. This case indicates that additional PMX-DHP therapy may be beneficial and technically feasible in patients with septic shock with severe myocardial injury refractory to ECMO support.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Martin GS. Sepsis, severe sepsis and septic shock: changes in incidence, pathogens and outcomes. Expert Rev Anti Infect Ther. 2012; 10:701–6.
Article2. Bréchot N, Luyt CE, Schmidt M, Leprince P, Trouillet JL, Léger P, et al. Venoarterial extracorporeal membrane oxygenation support for refractory cardiovascular dysfunction during severe bacterial septic shock. Crit Care Med. 2013; 41:1616–26.
Article3. Park TK, Yang JH, Jeon K, Choi SH, Choi JH, Gwon HC, et al. Extracorporeal membrane oxygenation for refractory septic shock in adults. Eur J Cardiothorac Surg. 2015; 47:e68–74.
Article4. Huang CT, Tsai YJ, Tsai PR, Ko WJ. Extracorporeal membrane oxygenation resuscitation in adult patients with refractory septic shock. J Thorac Cardiovasc Surg. 2013; 146:1041–6.
Article5. Ronco C, Klein DJ. Polymyxin B hemoperfusion: a mechanistic perspective. Crit Care. 2014; 18:309.
Article6. Cruz DN, Perazella MA, Bellomo R, de Cal M, Polanco N, Corradi V, et al. Effectiveness of polymyxin Bimmobilized fiber column in sepsis: a systematic review. Crit Care. 2007; 11:R47.
Article7. Cruz DN, Antonelli M, Fumagalli R, Foltran F, Brienza N, Donati A, et al. Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA. 2009; 301:2445–52.8. Weerwind PW, van der Veen FH, Gelsomino S, Nagaraj NG, Parise O, Lorusso R, et al. Cytokine removal on extracorporeal life support for treatment of acute endotoxemia: a randomized controlled animal study. Int J Cardiol. 2013; 168:4699–704.
Article9. Bruenger F, Kizner L, Weile J, Morshuis M, Gummert JF. First successful combination of ECMO with cytokine removal therapy in cardiogenic septic shock: a case report. Int J Artif Organs. 2015; 38:113–6.
Article10. Hirakawa E, Ibara S, Tokuhisa T, Hiwatashi S, Hayashida Y, Maede Y, et al. Septic neonate rescued by polymyxin B hemoperfusion. Pediatr Int. 2013; 55:e70–2.
Article11. Court O, Kumar A, Parrillo JE, Kumar A. Clinical review: Myocardial depression in sepsis and septic shock. Crit Care. 2002; 6:500–8.12. Sharma AS, Weerwind PW, Maessen JG. Extracorporeal membrane oxygenation resuscitation in adult patients with refractory septic shock. J Thorac Cardiovasc Surg. 2014; 147:1441–2.
Article13. Akira S. Pathogen recognition by innate immunity and its signaling. Proc Jpn Acad Ser B Phys Biol Sci. 2009; 85:143–56.
Article14. Cohen J. The immunopathogenesis of sepsis. Nature. 2002; 420:885–91.
Article15. Zhou F, Peng Z, Murugan R, Kellum JA. Blood purification and mortality in sepsis: a meta-analysis of randomized trials. Crit Care Med. 2013; 41:2209–20.16. Nakamura T, Ushiyama C, Shoji H, Koide H. Effects of hemoperfusion on serum cardiac troponin T concentrations using polymyxin B-immobilized fibers in septic patients undergoing hemodialysis. ASAIO J. 2002; 48:41–4.
Article17. Nakamura K, Doi K, Inokuchi R, Fukuda T, Hiruma T, Ishii T, et al. Endotoxin adsorption by polymyxin B column or intraaortic balloon pumping use for severe septic cardiomyopathy. Am J Emerg Med. 2013; 31:893.e1–3.
Article18. Sugimoto T, Deji N, Isono M, Kume S, Osawa N, Kanasaki K, et al. A case of acute renal failure complicated with Takotsubo cardiomyopathy. Nihon Toseki Igakkai Zasshi. 2004; 37:2093–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Refractory Septic Shock Treated with Nephrectomy under the Support of Extracorporeal Membrane Oxygenation
- A successful application of adult polymyxin B-immobilized fiber column hemoperfusion to a neonate with septic shock
- Polymyxin B Hemoperfusion in Pneumonic Septic Shock Caused by Gram-Negative Bacteria
- Initial Experience of Using Polymyxin B Hemoperfusion in Abdominal Septic Shock: Things to Consider for Better Outcome
- Polymyxin B Immobilized Fiber Hemoperfusion in Refractory Intra-abdominal Septic Shock