Ann Surg Treat Res.
2016 Sep;91(3):97-103. 10.4174/astr.2016.91.3.97.
Is focused parathyroidectomy appropriate for patients with primary hyperparathyroidism?
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. Jungjongj@yuhs.ac
- 2Department of Internal Medicine, Endocrine Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2350535
- DOI: http://doi.org/10.4174/astr.2016.91.3.97
Abstract
- PURPOSE
The aim of this study was to determine whether focused or complete parathyroidectomy was more appropriate and to compare follow-up data in primary hyperparathyroidism (PHPT).
METHODS
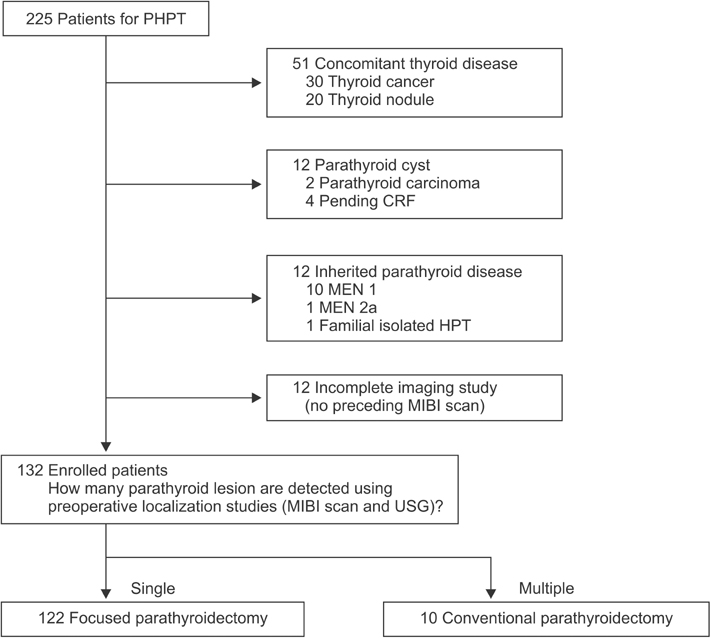
We retrospectively analyzed 225 operations for PHPT at Yonsei University Health System between 2000 and 2012. After excluding 93 patients, the remaining 132 were divided into 2 groups: those who underwent focused parathyroidectomy (FP) and those who underwent conventional parathyroidectomy (CP). We compared clinicopathological features; preoperative calcium, parathyroid hormone (PTH), phosphorus, vitamin D, 24-hour urine calcium, and alkaline phosphatase levels; postoperative calcium and PTH levels; pathologic diagnosis; multiplicity; and results of a localization study between the 2 groups.
RESULTS
There was no significant difference in the rates of development of postoperative persistent hyperparathyroidism (1/122 FP patients and 1/10 CP patients) between the 2 groups due to a technical reason (FP 0.8% vs. CP 10.0%, P = 0.146). Multiglandular disease (MGD) was uncommon in all cases (6 of 132, 4.5%). All MGD cases were diagnosed using a preoperative localization study. Sestamibi scan and ultrasonography sensitivity were 94.2% and 90.2%, respectively.
CONCLUSION
We suggest that FP is appropriate in PHPT, except in cases of MGD if detected before the operation using preoperative imaging. Knowledge of hereditary PHPT and improved preoperative localization studies, such as high-resolution ultrasonography, contributed to the decision to perform FP rather than CP in all cases of unilateral results of the localizing study.
Keyword
MeSH Terms
-
Alkaline Phosphatase
Calcium
Diagnosis
Follow-Up Studies
Humans
Hyperparathyroidism
Hyperparathyroidism, Primary*
Parathyroid Hormone
Parathyroidectomy*
Phosphorus
Retrospective Studies
Technetium Tc 99m Sestamibi
Ultrasonography
Vitamin D
Alkaline Phosphatase
Calcium
Parathyroid Hormone
Phosphorus
Technetium Tc 99m Sestamibi
Vitamin D
Figure
Reference
-
1. Adler JT, Sippel RS, Chen H. New trends in parathyroid surgery. Curr Probl Surg. 2010; 47:958–1017.2. Macfarlane DP, Yu N, Donnan PT, Leese GP. Should 'mild primary hyperparathyroidism' be reclassified as 'insidious': is it time to reconsider? Clin Endocrinol (Oxf). 2011; 75:730–737.3. Chen H, Sokoll LJ, Udelsman R. Outpatient minimally invasive parathyroidectomy: a combination of sestamibi-SPECT localization, cervical block anesthesia, and intraoperative parathyroid hormone assay. Surgery. 1999; 126:1016–1021.4. Flynn MB, Bumpous JM, Schill K, McMasters KM. Minimally invasive radioguided parathyroidectomy. J Am Coll Surg. 2000; 191:24–31.5. Nagar S, Reid D, Czako P, Long G, Shanley C. Outcomes analysis of intraoperative adjuncts during minimally invasive parathyroidectomy for primary hyperparathyroidism. Am J Surg. 2012; 203:177–181.6. Norman J, Politz D. Prospective study in 3,000 consecutive parathyroid operations demonstrates 18 objective factors that influence the decision for unilateral versus bilateral surgical approach. J Am Coll Surg. 2010; 211:244–249.7. Duh QY, Uden P, Clark OH. Unilateral neck exploration for primary hyperparathyroidism: analysis of a controversy using a mathematical model. World J Surg. 1992; 16:654–661.8. Norman J, Lopez J, Politz D. Abandoning unilateral parathyroidectomy: why we reversed our position after 15,000 parathyroid operations. J Am Coll Surg. 2012; 214:260–269.9. Yeh MW, Ituarte PH, Zhou HC, Nishimoto S, Liu IL, Harari A, et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013; 98:1122–1129.10. Lee SH, Hong SJ. Minimally invasive parathyroidectomy without an Intraoperative i-PTH test for patients with primary hyperparathyroidism. J Korean Surg Soc. 2008; 75:9–14.11. Lo CY, Lang BH, Chan WF, Kung AW, Lam KS. A prospective evaluation of preoperative localization by technetium-99m sestamibi scintigraphy and ultrasonography in primary hyperparathyroidism. Am J Surg. 2007; 193:155–159.12. Worsey MJ, Carty SE, Watson CG. Success of unilateral neck exploration for sporadic primary hyperparathyroidism. Surgery. 1993; 114:1024–1029.13. Mihai R, Simon D, Hellman P. Imaging for primary hyperparathyroidism--an evidence-based analysis. Langenbecks Arch Surg. 2009; 394:765–784.14. Agcaoglu O, Aliyev S, Heiden K, Neumann D, Milas M, Mitchell J, et al. A new classification of positive sestamibi and ultrasound scans in parathyroid localization. World J Surg. 2012; 36:2516–2521.15. Akram K, Parker JA, Donohoe K, Kolodny G. Role of single photon emission computed tomography/computed tomography in localization of ectopic parathyroid adenoma: a pictorial case series and review of the current literature. Clin Nucl Med. 2009; 34:500–502.16. Rodgers SE, Hunter GJ, Hamberg LM, Schellingerhout D, Doherty DB, Ayers GD, et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006; 140:932–940.17. Alexandrides TK, Kouloubi K, Vagenakis AG, Yarmenitis S, Spyridonidis T, Vassilakos P, et al. The value of scintigraphy and ultrasonography in the preoperative localization of parathyroid glands in patients with primary hyperparathyroidism and concomitant thyroid disease. Hormones (Athens). 2006; 5:42–51.18. Gill MT, Dean M, Karr J, Aultman DF, Nathan CO. Intraoperative parathyroid hormone assay: a necessary tool for multi-glandular disease. Otolaryngol Head Neck Surg. 2011; 144:691–697.19. Yip L, Pryma DA, Yim JH, Virji MA, Carty SE, Ogilvie JB. Can a lightbulb sestamibi SPECT accurately predict single-gland disease in sporadic primary hyperparathyroidism? World J Surg. 2008; 32:784–792.20. Wirowski D, Goretzki PE, Schwarz K, Lammers BJ, Dotzenrath C, Roher HD. Failed surgery in primary hyperparathyroidism: what has changed with time. Exp Clin Endocrinol Diabetes. 2013; 121:323–328.21. Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg. 2002; 235:665–670.22. Yoon JH, Chang HS, Park CS. Surgical strategy in the management of primary hyperparathyroidism. J Korean Surg Soc. 2004; 66:372–378.23. Harrison TS, Duarte B, Reitz RE, Princenthal R, Seaton JF, Badder EM, et al. Primary hyperparathyroidism: four-to eight-year postoperative follow-up demonstrating persistent functional insignificance of microscopic parathyroid hyperplasia and decreased autonomy of parathyroid hormone release. Ann Surg. 1981; 194:429–437.24. Mazeh H, Chen H, Leverson G, Sippel RS. Creation of a "Wisconsin index" nomogram to predict the likelihood of additional hyperfunctioning parathyroid glands during parathyroidectomy. Ann Surg. 2013; 257:138–141.25. Elaraj DM, Sippel RS, Lindsay S, Sansano I, Duh QY, Clark OH, et al. Are additional localization studies and referral indicated for patients with primary hyperparathyroidism who have negative sestamibi scan results? Arch Surg. 2010; 145:578–581.26. Ning L, Sippel R, Schaefer S, Chen H. What is the clinical significance of an elevated parathyroid hormone level after curative surgery for primary hyperparathyroidism? Ann Surg. 2009; 249:469–472.27. Carneiro DM, Solorzano CC, Nader MC, Ramirez M, Irvin GL 3rd. Comparison of intraoperative iPTH assay (QPTH) criteria in guiding parathyroidectomy: which criterion is the most accurate? Surgery. 2003; 134:973–979.28. Day KM, Elsayed M, Monchik JM. No need to abandon focused unilateral exploration for primary hyperparathyroidism with intraoperative monitoring of intact parathyroid hormone. J Am Coll Surg. 2015; 221:518–523.29. Kim HG, Kim WY, Woo SU, Lee JB, Lee YM. Minimally invasive parathyroidectomy with or without intraoperative parathyroid hormone for primary hyperparathyroidism. Ann Surg Treat Res. 2015; 89:111–116.30. Miura D, Wada N, Arici C, Morita E, Duh QY, Clark OH. Does intraoperative quick parathyroid hormone assay improve the results of parathyroidectomy? World J Surg. 2002; 26:926–930.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Disease of Parathyroid and Surgical Strategy
- A Case of Primary Hyperparathyroidism Associated with Hypercalcemic Crisis and Systemic Calcinosis
- Primary Hyperparathyroidism Assosiated with Pathologic Fracture: A Case Report
- Subtotal Parathyroidectomy for Tertiary Hyperparathyroidism: a Case Report and Literature Review
- Surgical Experience of Primary Hyperparathyroidism: Analysis of Postoperative Outcomes