Allergy Asthma Immunol Res.
2016 Nov;8(6):512-521. 10.4168/aair.2016.8.6.512.
Emergency Department Visits for Asthma Exacerbation due to Weather Conditions and Air Pollution in Chuncheon, Korea: A Case-Crossover Analysis
- Affiliations
-
- 1Department of Allergy and Clinical Immunology, Kangwon National University School of Medicine, Chuncheon, Korea.
- 2Department of Internal Medicine and Environmental Health Center, Kangwon National University Hospital, Chuncheon, Korea. wjkim47@gmail.com
- 3Department of Environmental Science, Kangwon National University, Chuncheon, Korea.
- 4Department of Preventive Medicine, Kangwon National University Hospital, Chuncheon, Korea.
- 5Department of Internal Medicine, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea.
- 6Department of Biostatistics, Graduate School of Public Health, Seoul National University, Seoul, Korea.
- KMID: 2349991
- DOI: http://doi.org/10.4168/aair.2016.8.6.512
Abstract
- PURPOSE
This retrospective study was conducted to estimate the effects of climate factors and air pollution on asthma exacerbations using a case-crossover analysis.
METHODS
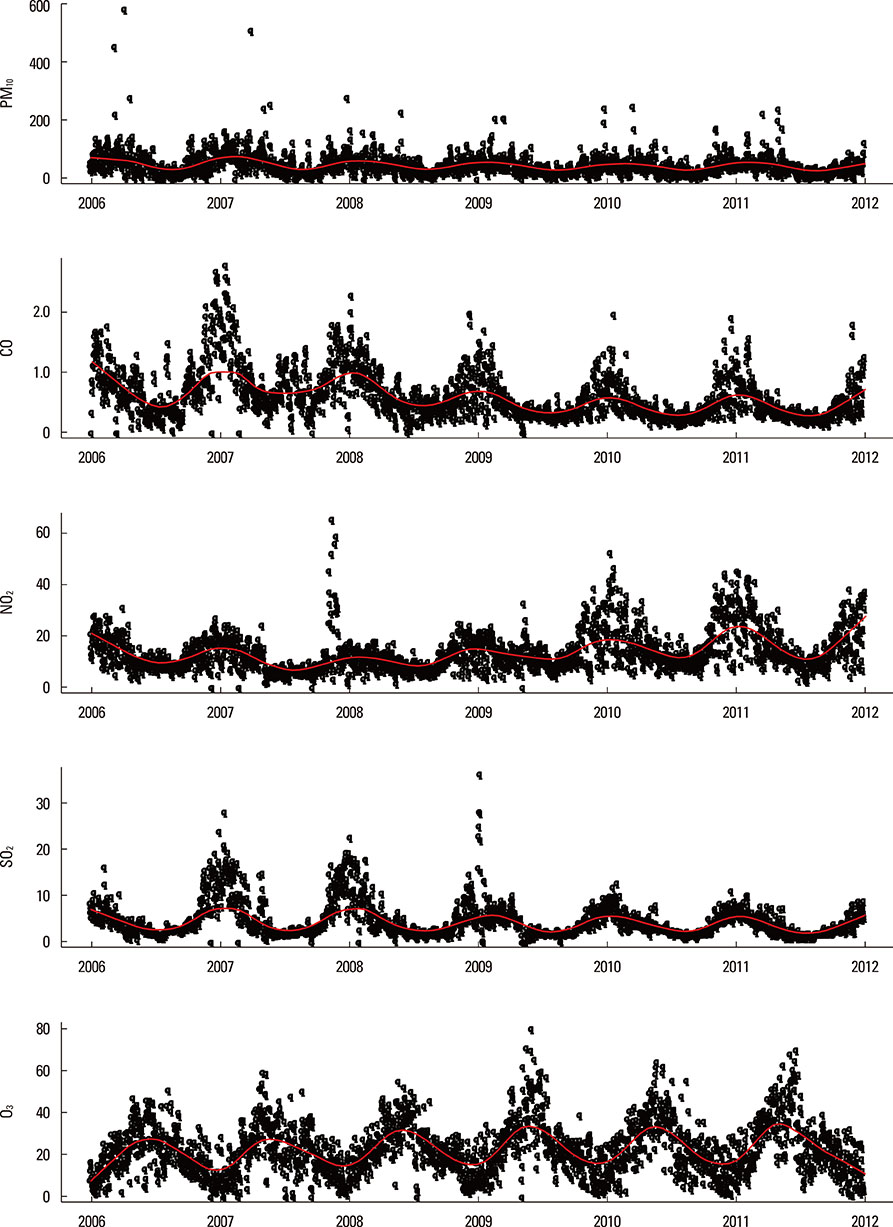
Patients who visited the emergency department (ED) of 2 university hospitals in Chuncheon for asthma exacerbations from January 1, 2006, to December 31, 2011, were enrolled. Daily average data for meteorological factors (temperature, daily temperature range, relative humidity, wind speed, atmospheric pressure, presence of rain, solar irradiation, and presence of fog) and the daily average levels of gaseous air pollutants (SO2, NO2, O3, CO, and PM10) were obtained. A case-crossover analysis was performed using variables about the weather and air pollution at 1-week intervals between cases and controls before and after ED visits.
RESULTS
There were 660 ED visits by 583 patients with asthma exacerbations. Low relative humidity (lag 1 and 2) and high wind speed (lag 1, 2, and 3) were associated with ED visits for asthma. Fog (lag 2) showed protective effects against asthma exacerbations in Chuncheon (risk increase: -29.4% [95% CI=-46.3% to -7.2%], P=0.013). These relationships were stronger in patients ≤19 years old than in those >60 years old. High levels of ambient CO (lag 1, 2, and 3) and NO2 (lag 2 and 3) were associated with decreased ED visits for asthma. However, there were no significant relationships among levels of ambient CO or NO2 and asthma exacerbations after adjusting for wind speed and relative humidity.
CONCLUSIONS
High wind speed and low humidity were associated with an increased risk of asthma ED visits. Fog was associated with a decreased risk of asthma ED visits after controlling for seasonal variations in weather and air pollution.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Air pollution and climate change: Effects on asthmatic patients
Hye-Kyung Park
Allergy Asthma Respir Dis. 2018;6(2):79-84. doi: 10.4168/aard.2018.6.2.79.
Reference
-
1. Lee CC, Sheridan SC, Lin S. Relating weather types to asthma-related hospital admissions in New York State. Ecohealth. 2012; 9:427–439.2. Rundell KW, Sue-Chu M. Air quality and exercise-induced bronchoconstriction in elite athletes. Immunol Allergy Clin North Am. 2013; 33:409–421.3. Rossi OV, Kinnula VL, Tienari J, Huhti E. Association of severe asthma attacks with weather, pollen, and air pollutants. Thorax. 1993; 48:244–248.4. Takizawa H. Impact of air pollution on allergic diseases. Korean J Intern Med. 2011; 26:262–273.5. D'Amato G, Cecchi L. Effects of climate change on environmental factors in respiratory allergic diseases. Clin Exp Allergy. 2008; 38:1264–1274.6. Twaroch TE, Curin M, Valenta R, Swoboda I. Mold allergens in respiratory allergy: from structure to therapy. Allergy Asthma Immunol Res. 2015; 7:205–220.7. Atkinson RW, Strachan DP. Role of outdoor aeroallergens in asthma exacerbations: epidemiological evidence. Thorax. 2004; 59:277–278.8. Carey MJ, Cordon I. Asthma and climatic conditions: experience from Bermuda, an isolated island community. Br Med J (Clin Res Ed). 1986; 293:843–844.9. Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991; 133:144–153.10. Hashimoto M, Fukuda T, Shimizu T, Watanabe S, Watanuki S, Eto Y, et al. Influence of climate factors on emergency visits for childhood asthma attack. Pediatr Int. 2004; 46:48–52.11. Villeneuve PJ, Leech J, Bourque D. Frequency of emergency room visits for childhood asthma in Ottawa, Canada: the role of weather. Int J Biometeorol. 2005; 50:48–56.12. Kim BJ, Lee SY, Kim HB, Lee E, Hong SJ. Environmental changes, microbiota, and allergic diseases. Allergy Asthma Immunol Res. 2014; 6:389–400.13. Dales RE, Cakmak S, Burnett RT, Judek S, Coates F, Brook JR. Influence of ambient fungal spores on emergency visits for asthma to a regional children's hospital. Am J Respir Crit Care Med. 2000; 162:2087–2090.14. Dales RE, Cakmak S, Judek S, Dann T, Coates F, Brook JR, et al. The role of fungal spores in thunderstorm asthma. Chest. 2003; 123:745–750.15. Chavarría JF. Short report: Asthma admissions and weather conditions in Costa Rica. Arch Dis Child. 2001; 84:514–515.16. Ehara A, Takasaki H, Takeda Y, Kida T, Mizukami S, Hagisawa M, et al. Are high barometric pressure, low humidity and diurnal change of temperature related to the onset of asthmatic symptoms? Pediatr Int. 2000; 42:272–274.17. Arnedo-Pena A, García-Marcos L, Bercedo-Sanz A, Aguinaga-Ontoso I, González-Díaz C, García-Merino A, et al. Prevalence of asthma symptoms in schoolchildren, and climate in west European countries: an ecologic study. Int J Biometeorol. 2013; 57:775–784.18. Khot A, Burn R, Evans N, Lenney W, Storr J. Biometeorological triggers in childhood asthma. Clin Allergy. 1988; 18:351–358.19. Vanos JK. Children's health and vulnerability in outdoor microclimates: A comprehensive review. Environ Int. 2015; 76:1–15.20. Simoni M, Baldacci S, Maio S, Cerrai S, Sarno G, Viegi G. Adverse effects of outdoor pollution in the elderly. J Thorac Dis. 2015; 7:34–45.21. Tanaka H, Honma S, Nishi M, Igarashi T, Nishio F, Abe S. Two-year follow-up study of the effect of acid fog on adult asthma patients. Intern Med. 1996; 35:100–104.22. Kashiwabara K, Kohrogi H, Ota K, Moroi T. High frequency of emergency room visits of asthmatic children on misty or foggy nights. J Asthma. 2002; 39:711–717.23. Tanaka H, Honma S, Nishi M, Igarashi T, Teramoto S, Nishio F, et al. Acid fog and hospital visits for asthma: an epidemiological study. Eur Respir J. 1998; 11:1301–1306.24. Klemm O, Schemenauer RS, Lummerich A, Cereceda P, Marzol V, Corell D, et al. Fog as a fresh-water resource: overview and perspectives. Ambio. 2012; 41:221–234.25. McCreanor J, Cullinan P, Nieuwenhuijsen MJ, Stewart-Evans J, Malliarou E, Jarup L, et al. Respiratory effects of exposure to diesel traffic in persons with asthma. N Engl J Med. 2007; 357:2348–2358.26. Cadelis G, Tourres R, Molinie J, Petit RH. Exacerbations of asthma in Guadeloupe (French West Indies) and volcanic eruption in Montserrat (70 km from Guadeloupe). Rev Mal Respir. 2013; 30:203–214.27. Lai LW. Effect of photochemical smog associated with synoptic weather patterns on cardiovascular and respiratory hospital admissions in metropolitan Taipei. Int J Environ Health Res. 2012; 22:287–304.28. Kim S, Kim Y, Lee MR, Kim J, Jung A, Park JS, et al. Winter season temperature drops and sulfur dioxide levels affect on exacerbation of refractory asthma in South Korea: a time-trend controlled case-crossover study using soonchunhyang asthma cohort data. J Asthma. 2012; 49:679–687.29. Sun HL, Chou MC, Lue KH. The relationship of air pollution to ED visits for asthma differ between children and adults. Am J Emerg Med. 2006; 24:709–713.30. Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, Todd K, et al. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005; 16:164–174.31. Kashiwabara K, Itonaga K, Moroi T. Airborne water droplets in mist or fog may affect nocturnal attacks in asthmatic children. J Asthma. 2003; 40:405–411.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea
- Short-term Effect of Air Pollution on Respiratory Disease in Seoul : A Case-Crossover Study
- Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea: A case-crossover study
- Effects of Air Pollution on Asthma in Seoul: Comparisons across Subject Characteristic
- Effect of Air Pollution on Emergency Room Visits for Asthma: a Time Series Analysis