J Korean Soc Radiol.
2016 Aug;75(2):126-132. 10.3348/jksr.2016.75.2.126.
Characteristic Sonographic and Follow Up Features of Thyroid Nodules According to Childhood Age Groups
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Hospital, Seoul, Korea. ywchang@schmc.ac.kr
- 2Department of Pediatrics, Soonchunhyang University Hospital, Seoul, Korea.
- KMID: 2344802
- DOI: http://doi.org/10.3348/jksr.2016.75.2.126
Abstract
- PURPOSE
We analyzed the spectrum and the significance of pediatric thyroid nodules depicted on sonography and evaluated the follow-up change according to the age group.
MATERIALS AND METHODS
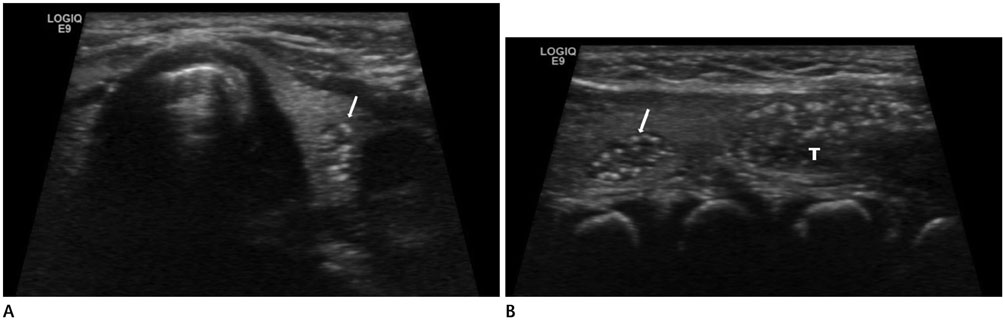
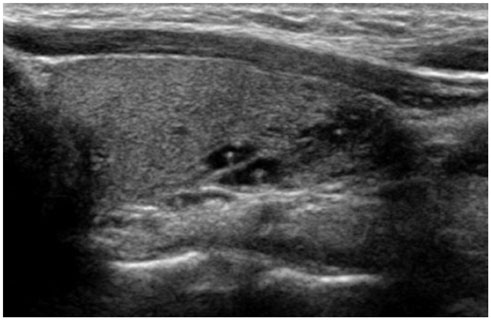
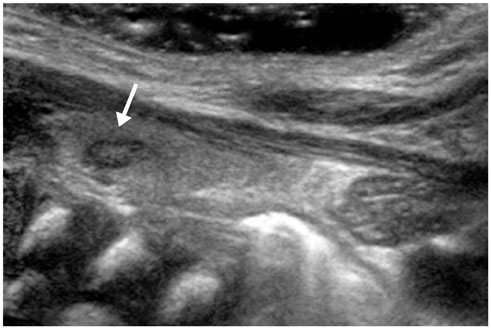
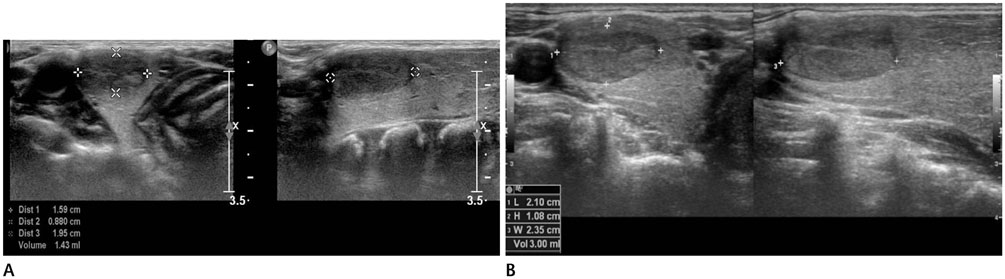
We retrospectively reviewed the sonographic features of 82 nodules in 69 patients (6.6%) among 1282 children less than 13 years of age without a palpable lesion, from January 2006 to January 2013. Patients were divided into three age groups; infants, preschoolers, and schoolers. Thyroid nodules were evaluated according to their sonographic characteristics (simple cyst, colloid cyst, solid mass, or intrathyroid thymus) and the changes detected at follow-up (disappearance, decrease in size, no change or increase in size) were reported.
RESULTS
There was a significant difference in the nodule patterns among the age groups (p < 0.001). The nodules in infants included a simple cyst (n = 12), a solid mass (n = 12), or an intra-thyroid thymus (n = 9). The preschoolers had a simple cyst (n = 11), a colloid cyst (n = 5), a solid mass (n = 3) or an intra-thyroid thymus (n = 5). However, the schoolers had a simple cyst (n = 2), a colloid cyst (n = 18), and a solid mass (n = 5), but there was no case of intra-thyroid thymus. Follow-up of 38 cases revealed significant differences among the age groups (p = 0.018). The nodules in infants showed findings such as disappearance of nodules (n = 9) and no change (n = 10) on follow-up sonography. In preschoolers, the nodules had disappeared (n = 2), decreased in size (n = 1), and showed no change (n = 11). However, the nodules in schoolers were found to be decreased in size (n = 1), show no change (n = 2), and increased in size (n = 2). The proven pathologic finding was benign in four patients.
CONCLUSION
There were significant differences in the prevalence and the interval change of thyroid nodules among infants, preschoolers, and schoolers. A large series of intrathyroid thymus was seen in infants and preschoolers, and masses did not increase in size in these age groups. The frequency of a colloid cyst could be increased in schoolers, and masses were increased in size in this age group, but none of the patients showed a malignant finding on pathology.
MeSH Terms
Figure
Reference
-
1. Babcock DS. Thyroid disease in the pediatric patient: emphasizing imaging with sonography. Pediatr Radiol. 2006; 36:299–308. quiz 372-373.2. Mirshemirani A, Roshanzamir F, Tabari AK, Ghorobi J, Salehpoor S, Gorji FA. Thyroid nodules in childhood: a single institute experience. Iran J Pediatr. 2010; 20:91–96.3. Mazzaferri EL. Management of a solitary thyroid nodule. N Engl J Med. 1993; 328:553–559.4. Niedziela M. Pathogenesis, diagnosis and management of thyroid nodules in children. Endocr Relat Cancer. 2006; 13:427–453.5. Hegedüs L. Clinical practice. The thyroid nodule. N Engl J Med. 2004; 351:1764–1771.6. Francis GL, Waguespack SG, Bauer AJ, Angelos P, Benvenga S, Cerutti JM, et al. Management guidelines for children with thyroid nodules and differentiated thyroid cancer. Thyroi. 2015; 25:716–759.7. Avula S, Daneman A, Navarro OM, Moineddin R, Urbach S, Daneman D. Incidental thyroid abnormalities identified on neck US for non-thyroid disorders. Pediatr Radiol. 2010; 40:1774–1780.8. Kim HG, Kim MJ, Lee MJ. Sonographic appearance of intrathyroid ectopic thymus in children. J Clin Ultrasound. 2012; 40:266–271.9. Segni M, di Nardo R, Pucarelli I, Biffoni M. Ectopic intrathyroidal thymus in children: a long-term follow-up study. Horm Res Paediatr. 2011; 75:258–263.10. Chng CL, Kocjan G, Kurzawinski TR, Beale T. Intrathyroidal ectopic thymic tissue mimicking thyroid cancer in children. Endocr Pract. 2014; 20:e241–e245.11. Durmaz E, Barsal E, Parlak M, Gurer I, Karaguzel G, Akcurin S, et al. Intrathyroidal ectopic thymic tissue may mimic thyroid cancer: a case report. J Pediatr Endocrinol Metab. 2012; 25:997–1000.12. Megremis S, Stiakaki E, Tritou I, Bonapart IE, Tsilimigaki A. Ectopic intrathyroidal thymus misdiagnosed as a thyroid nodule: sonographic appearance. J Clin Ultrasound. 2008; 36:443–447.13. Segni M, Nuti F, di Nardo R. Ectopic intrathyroidal thymus in an 11-year-old boy. Thyroid. 2006; 16:1179–1180.14. Hernandez-Cassis C, Poniecka A, Vogel CK, McKenzie JM. A six-year-old boy with a suspicious thyroid nodule: intrathyroidal thymic tissue. Thyroid. 2008; 18:377–380.15. Lignitz S, Musholt TJ, Kreft A, Engel R, Brzezinska R, Pohlenz J. Intrathyroidal thymic tissue surrounding an intrathyroidal parathyroid gland, the cause of a solitary thyroid nodule in a 6-year-old boy. Thyroid. 2008; 18:1125–1130.16. Gimm O, Krause U, Wessel H, Finke R, Dralle H. Ectopic intrathyroidal thymus diagnosed as a solid thyroid lesion: case report and review of the literature. J Pediatr Surg. 1997; 32:1241–1243.17. Courcoutsakis N, Patronas N, Filie AC, Carney JA, Moraitis A, Stratakis CA. Ectopic thymus presenting as a thyroid nodule in a patient with the Carney complex. Thyroid. 2009; 19:293–296.18. Han BK, Suh YL, Yoon HK. Thymic ultrasound. I. Intrathymic anatomy in infants. Pediatr Radiol. 2001; 31:474–479.19. Park SH, Ryu CW, Kim GY, Shim KS. Intrathyroidal thymic tissue mimicking a malignant thyroid nodule in a 4-year-old child. Ultrasonography. 2014; 33:71–73.20. Patel MN, Komlos M, Racadio JM. Intrathyroidal thymic tissue mimicking a thyroid nodule in a 4-year-old child. J Clin Ultrasound. 2013; 41:319–320.21. Aguayo-Figueroa L, Golightly MG, Hu Y, Cohen HL, Wilson TA. Cytology and flow cytometry to identify ectopic thymic tissue masquerading as a thyroid nodule in two children. Thyroid. 2009; 19:403–406.22. Gupta A, Ly S, Castroneves LA, Frates MC, Benson CB, Feldman HA, et al. A standardized assessment of thyroid nodules in children confirms higher cancer prevalence than in adults. J Clin Endocrinol Metab. 2013; 98:3238–3245.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sonographic Evaluation of Thyroid Nodules
- Pathologic basis of the sonographic differences between thyroid cancer and noninvasive follicular thyroid neoplasm with papillary-like nuclear features
- Ultrasound-Guided Fine-Needle Aspiration Biopsy of Multiple Thyroid Nodules
- Differentiation of Benign and Malignant Thyroid Nodules: Sonographic Analysis and a New Scoring System
- Thyroid Nodules with Macrocalcification: Sonographic Findings Predictive of Malignancy