Korean Circ J.
2016 Mar;46(2):213-221. 10.4070/kcj.2016.46.2.213.
Predicting Left Ventricular Dysfunction after Surgery in Patients with Chronic Mitral Regurgitation: Assessment of Myocardial Deformation by 2-Dimensional Multilayer Speckle Tracking Echocardiography
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Cardiovascular Imaging Center, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. tyche.park@gmail.com
- 2Department of Thorax Surgery, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Cardiology Clinic, National Cancer Center, Goyang, Korea.
- KMID: 2344473
- DOI: http://doi.org/10.4070/kcj.2016.46.2.213
Abstract
- BACKGROUND AND OBJECTIVES
The development of postoperative left ventricular (LV) dysfunction is a frequent complication in patients with chronic severe mitral valve regurgitation (MR) and portends a poor prognosis. Assessment of myocardial deformation enables myocardial contractility to be accurately estimated. The aim of the present study was to evaluate the predictive value of preoperative regional LV contractile function assessment using two-dimensional multilayer speckle-tracking echocardiography (2D MSTE) analysis in patients with chronic severe MR with preserved LV systolic function.
SUBJECTS AND METHODS
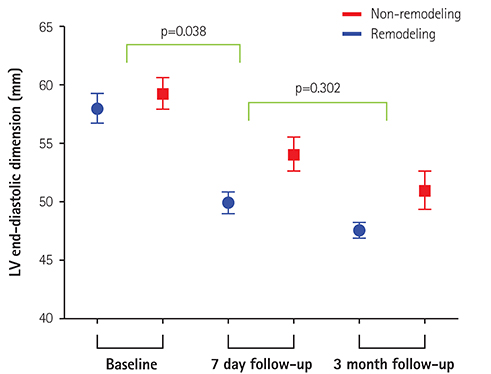
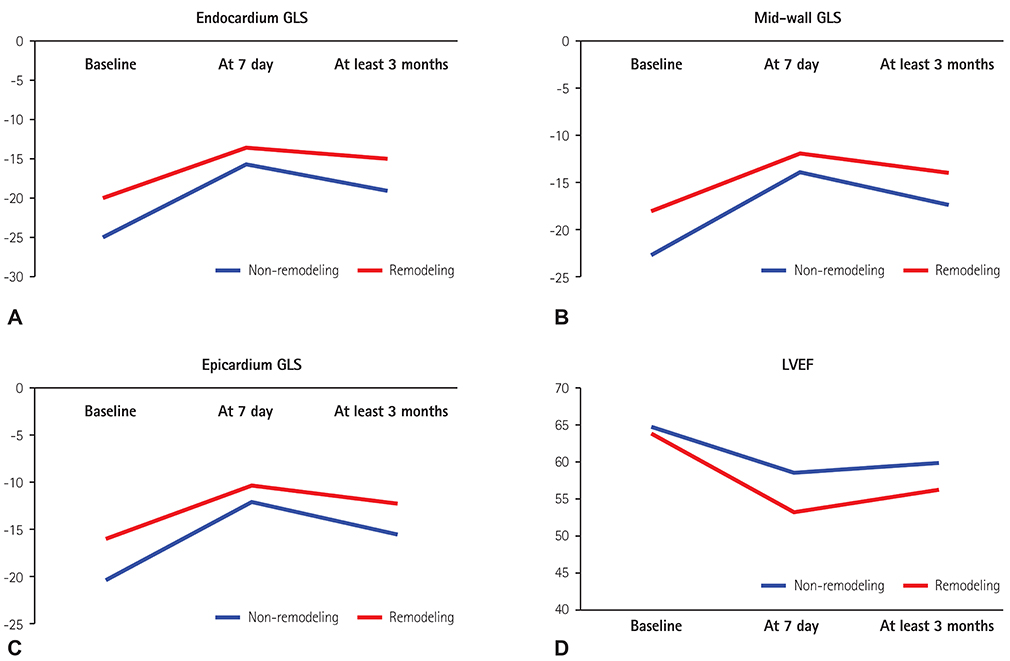
Forty-three consecutive patients with chronic severe MR with preserved LV systolic function scheduled for mitral valve replacement (MVR) or MV repair were prospectively enrolled. Serial echocardiographic studies were performed before surgery, at 7 days follow-up, and at least 3 months follow-up postoperatively. The conventional echocardiographic parameters were analyzed. Global longitudinal strain (GLS) was obtained quantitatively by 2D MSTE.
RESULTS
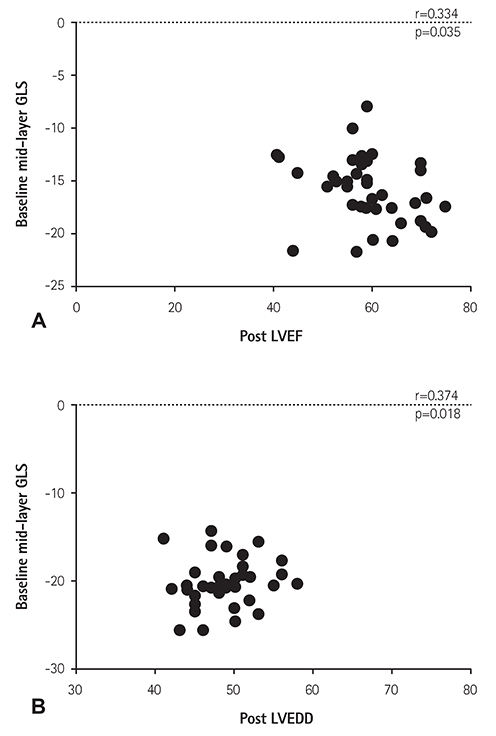
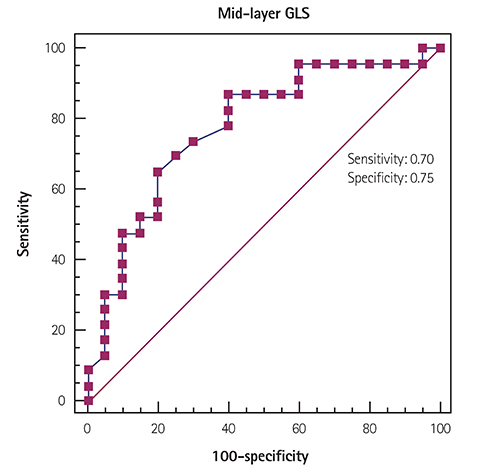
The mean age of patients was 51.7±14.3 years and 25 (58.1%) were male. In receiver-operating characteristic curve analysis, the most useful cutoff value for discriminating postoperative LV remodeling in severe MR with normal LV systolic function was -20.5% of 2D mid-layer GLS. Patients were divided into two groups by the baseline GLS -20.5%. Preoperative GLS values strongly predicted postoperative LV remodeling or LV dysfunction. The postoperative degree of decrease in LV end-diastolic dimension might be an additive predictive factor.
CONCLUSION
STE can be used to predict a decrease in LV function after MVR in patients with chronic severe MR. This promising method could be of use in the clinic when trying to decide upon the optimum time to schedule surgery for such patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC). European Association for Cardio-Thoracic Surgery (EACTS). Vahanian A, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012; 33:2451–2496.2. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2438–2488.3. Witkowski TG, Thomas JD, Debonnaire PJ, et al. Global longitudinal strain predicts left ventricular dysfunction after mitral valve repair. Eur Heart J Cardiovasc Imaging. 2013; 14:69–76.4. Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med. 2005; 352:875–883.5. Rosenhek R, Rader F, Klaar U, et al. Outcome of watchful waiting in asymptomatic severe mitral regurgitation. Circulation. 2006; 113:2238–2244.6. Mascle S, Schnell F, Thebault C, et al. Predictive value of global longitudinal strain in a surgical population of organic mitral regurgitation. J Am Soc Echocardiogr. 2012; 25:766–772.7. Grigioni F, Tribouilloy C, Avierinos JF, et al. Outcomes in mitral regurgitation due to flail leaflets a multicenter European study. JACC Cardiovasc Imaging. 2008; 1:133–141.8. Enriquez-Sarano M, Sundt TM 3rd. Early surgery is recommended for mitral regurgitation. Circulation. 2010; 121:804–811. discussion 8129. Starling MR, Kirsh MM, Montgomery DG, Gross MD. Impaired left ventricular contractile function in patients with long-term mitral regurgitation and normal ejection fraction. J Am Coll Cardiol. 1993; 22:239–250.10. Greenbaum RA, Ho SY, Gibson DG, Becker AE, Anderson RH. Left ventricular fibre architecture in man. Br Heart J. 1981; 45:248–263.11. Mizuguchi Y, Oishi Y, Miyoshi H, Iuchi A, Nagase N, Oki T. The functional role of longitudinal, circumferential, and radial myocardial deformation for regulating the early impairment of left ventricular contraction and relaxation in patients with cardiovascular risk factors: a study with two-dimensional strain imaging. J Am Soc Echocardiogr. 2008; 21:1138–1144.12. Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003; 41:1–12.13. Luchner A, Behrens G, Stritzke J, et al. Long-term pattern of brain natriuretic peptide and N-terminal pro brain natriuretic peptide and its determinants in the general population: contribution of age, gender, and cardiac and extra-cardiac factors. Eur J Heart Fail. 2013; 15:859–867.14. Banovic M, Vujisic-Tesic B, Bojic S, et al. Diagnostic value of NT-proBNP in identifying impaired coronary flow reserve in asymptomatic moderate or severe aortic stenosis. Biomark Med. 2013; 7:221–227.15. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.16. Sohn DW, Chai IH, Lee DJ, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol. 1997; 30:474–480.17. Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003; 16:777–802.18. Chen CG, Thomas JD, Anconina J, et al. Impact of impinging wall jet on color Doppler quantification of mitral regurgitation. Circulation. 1991; 84:712–720.19. Adamu U, Schmitz F, Becker M, Kelm M, Hoffmann R. Advanced speckle tracking echocardiography allowing a three-myocardial layer-specific analysis of deformation parameters. Eur J Echocardiogr. 2009; 10:303–308.20. Suri RM, Schaff HV, Dearani JA, et al. Recovery of left ventricular function after surgical correction of mitral regurgitation caused by leaflet prolapse. J Thorac Cardiovasc Surg. 2009; 137:1071–1076.21. Matsumura T, Ohtaki E, Tanaka K, et al. Echocardiographic prediction of left ventricular dysfunction after mitral valve repair for mitral regurgitation as an indicator to decide the optimal timing of repair. J Am Coll Cardiol. 2003; 42:458–463.22. Ahmed MI, Gladden JD, Litovsky SH, et al. Increased oxidative stress and cardiomyocyte myofibrillar degeneration in patients with chronic isolated mitral regurgitation and ejection fraction >60%. J Am Coll Cardiol. 2010; 55:671–679.23. de Isla LP, de Agustin A, Rodrigo JL, et al. Chronic mitral regurgitation: a pilot study to assess preoperative left ventricular contractile function using speckle-tracking echocardiography. J Am Soc Echocardiogr. 2009; 22:831–838.24. Kim MS, Kim YJ, Kim HK, et al. Evaluation of left ventricular short- and long-axis function in severe mitral regurgitation using 2-dimensional strain echocardiography. Am Heart J. 2009; 157:345–351.25. Witkowski TG, Thomas JD, Delgado V, et al. Changes in left ventricular function after mitral valve repair for severe organic mitral regurgitation. Ann Thorac Surg. 2012; 93:754–760.26. Sengupta PP, Krishnamoorthy VK, Korinek J, et al. Left ventricular form and function revisited: applied translational science to cardiovascular ultrasound imaging. J Am Soc Echocardiogr. 2007; 20:539–551.27. Vendelin M, Bovendeerd PH, Engelbrecht J, Arts T. Optimizing ventricular fibers: uniform strain or stress, but not ATP consumption, leads to high efficiency. Am J Physiol Heart Circ Physiol. 2002; 283:H1072–H1081.28. Leitman M, Lysiansky M, Lysyansky P, et al. Circumferential and longitudinal strain in 3 myocardial layers in normal subjects and in patients with regional left ventricular dysfunction. J Am Soc Echocardiogr. 2010; 23:64–70.29. Manaka M, Tanaka N, Takei Y, Kurohane S, Takazawa K, Yamashina A. Assessment of regional myocardial systolic function in hypertensive left ventricular hypertrophy using harmonic myocardial strain imaging. J Cardiol. 2005; 45:53–60.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of 3-Dimensional Speckle Tracking Echocardiography: A Review from Our Experiences
- Functional Assessment for Congenital Heart Disease
- Characteristics of Myocardial Deformation and Rotation in Subjects With Diastolic Dysfunction Without Diastolic Heart Failure
- Echocardiographic Assessment of Mitral Valve Regurgitation
- Assessment of Mitral Valve Complex by Three-Dimensional Echocardiography: Therapeutic Strategy for Functional Mitral Regurgitation