J Korean Ophthalmol Soc.
2015 Jun;56(6):823-829. 10.3341/jkos.2015.56.6.823.
Results of the Cultured Nasolacrimal Polyurethane Stents (Song's stent(R)) in Nasolacrimal Duct Obstruction Treatment
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University School of Medicine, Busan, Korea. jongsool@pusan.ac.kr
- KMID: 2339145
- DOI: http://doi.org/10.3341/jkos.2015.56.6.823
Abstract
- PURPOSE
In the present study, we cultured specimens and evaluated the types of bacteria existing at the stent and their antibiotic sensitivities from removed nasolacrimal polyurethane stents (Song's stents) due to recurrent inflammation or Song's stent obstruction after placement of Song's stents without fluoroscopic guidance for the treatment of obstructed nasolacrimal ducts.
METHODS
In 11 eyes of 11 patients who received Song's stent intubation to resolve nasolacrimal duct obstruction, the Song's stents were removed due to either recurred symptoms, signs of chronic dacryocystitis, or tube obstruction. Song's stents were cultured to identify bacteria and tested for their antibiotic sensitivity.
RESULTS
The Song's stent removal was from 3 years 7 months to 17 years 1 month after intubation, thus the average duration was 10 years. The species of cultured bacteria were Pseudomonas in 7 eyes, Staphylococcus aureus in 2 eyes, and Stenotrophomonas maltophilia in 2 eyes. In antibiotics sensitivity tests, 5 of 7 eyes with Pseudomonas were resistant to trimethoprime/sulfamethoxazole (Bactrim(R), Roche, Basel, Switzerland) and 2 eyes with Staphylococcus aureus were resistant to penicillin. Ten eyes underwent silicone tube intubation simultaneously during Song's stent removal and 1 eye underwent Song's stent removal only.
CONCLUSIONS
The most common bacteriological etiology of Song's stent obstruction or recurrent inflammation is Pseudomonas species. The use of efficient antibiotics is necessary to avoid antibiotic intolerance and simultaneous silicone tube intubation during Song's stent removal and is essential for the management of epiphora.
MeSH Terms
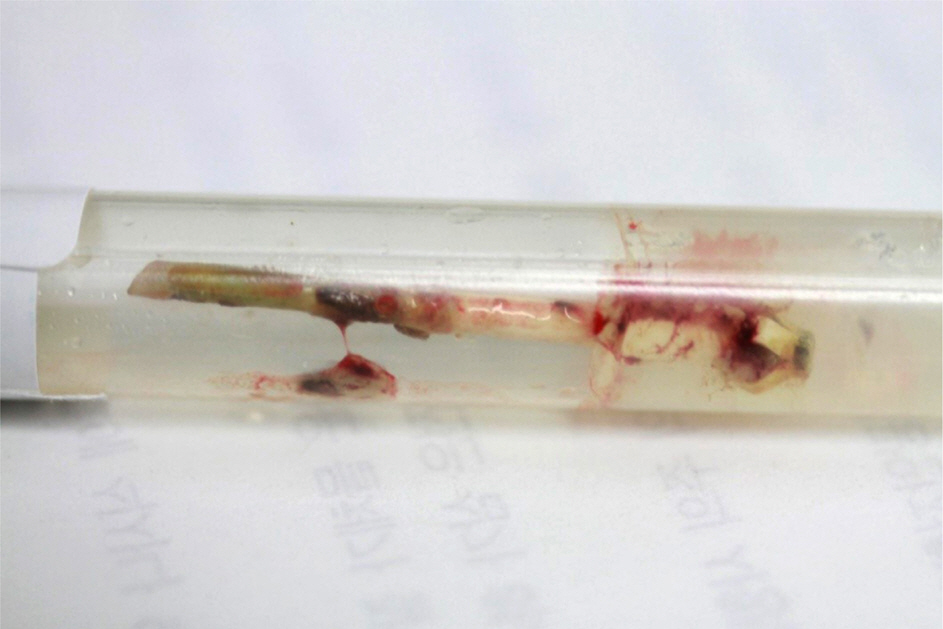
Figure
Reference
-
References
1. Song HY, Jin YH, Kim JH, et al. Nasolacrimal duct obstruction treated nonsurgically with use of plastic stents. Radiology. 1994; 190:535–9.
Article2. Kim BO, Jin KH, Oh JH. Clinical observation on nasolacrimal duct stent intubation in obstruction of nasolacrimal system. J Korean Ophthalmol Soc. 1995; 36:994–9.3. Lee JS, Jeong G, Lee SH, Oum BS. Treatment of obstructed nasolacrimal duct by lacrimal stent without fluoroscopic guidance. J Korean Ophthalmol Soc. 1996; 37:2125–31.4. Suk KW, Kim SS. Long-term outcome of nasolacrimal duct obstruction treated with nasolacrimal polyurethane stents (Song's stent). J Korean Ophthalmol Soc. 2008; 49:1209–14.
Article5. Oztürk S, Konuk O, Ilgit ET, et al. Outcome of patients with nasolacrimal polyurethane stent implantation: do they keep tearing? Ophthal Plast Reconstr Surg. 2004; 20:130–5.6. Lee JH, Kang MS, Yang JW. Clinicopathologic findings after nasolacrimal polyurethane stent implantations. Korean J Ophthalmol. 2005; 19:252–7.
Article7. Shin HM, Lew H, Lee JM. Cytologic study of removed silicone tube in nasolacrimal duct obstruction patients with the liquid-based thin layer preparation technique. J Korean Ophthalmol Soc. 2004; 45:707–13.8. Park SW, Park JM, Lee JE, Lee JS. Results of the cultured Jones tubes used in lacrimal bypass surgery. J Korean Ophthalmol Soc. 2006; 47:696–702.9. Lee JS, Jung G, Oum BS, et al. Clinical efficacy of the polyurethane stent without fluoroscopic guidance in the treatment of nasolacrimal duct obstruction. Ophthalmology. 2000; 107:1666–70.
Article10. Toti A. New conservative approach of radical cure of chronic sup-puration of the lacrimal sac (dacryocystorhinostomy). Clin Mod Firenze. 1904; 10:385–7.11. Häusler R, Caversaccio M. Microsurgical endonasal dacryocystorhinostomy with long-term insertion of bicanalicular silicone tubes. Arch Otolaryngol Head Neck Surg. 1998; 124:188–91.
Article12. Neuhaus RW. Orbital complications secondary to endoscopic sinus surgery. Ophthalmology. 1990; 97:1512–8.
Article13. Cunningham MJ, Woog JJ. Endonasal endoscopic dacryocystorhinostomy in children. Arch Otolaryngol Head Neck Surg. 1998; 124:328–33.
Article14. Woog JJ, Metson R, Puliafito CA. Holmium:YAG endonasal laser dacryocystorhinostomy. Am J Ophthalmol. 1993; 116:1–10.15. Boush GA, Lemke BN, Dortzbach RK. Results of endonasal laser-assisted dacryocystorhinostomy. Ophthalmology. 1994; 101:955–9.
Article16. Kong YT, Kim TI, Kong BW. A report of 131 cases of endoscopic laser lacrimal surgery. Ophthalmology. 1994; 101:1793–1800.
Article17. Lee SH, Chung WS. Long term surgical efficacy of endonasal da-cryo cys torhinostomy. J Korean Ophthalmol Soc. 2000; 41:307–13.18. Rice DH. Endoscopic intranasal dacryocystorhinostomy results in four patients. Arch Otolaryngol Head Neck Surg. 1990; 116:1061.
Article19. Schaudig U, Maas R. The polyurethane nasolacrimal duct stent for lower tear duct obstruction: long-term success rate and complications. Graefes Arch Clin Exp Ophthalmol. 2000; 238:733–7.
Article20. Chaudhry IA, Shamsi FA, Al-Rashed W. Bacteriology of chronic dacryocystitis in a tertiary eye care center. Ophthal Plast Reconstr Surg. 2005; 21:207–10.
Article21. Lee JS, Oum BS, Lee JE, et al. Treatment of obstructed lacrimal ap-paratus by Bowman's Probe Guided Lacrimal Bypass Surgery. J Korean Ophthalmol Soc. 1999; 40:1746–54.22. Yazici B, Yazici Z, Parlak M. Treatment of nasolacrimal duct obstruction in adults with polyurethane stent. Am J Ophthalmol. 2001; 131:37–43.
Article23. Rhim WI, Kim HS, Lew H, Yun YS. Morphological study of removed silicone tube from nasolacrimal duct obstruction patients. J Korean Ophthalmol Soc. 2002; 43:2106–11.24. Ma YR, Jong SK. The study of chronic dacryocystitis: identification of pathogenic organism and histopathological findings. J Korean Ophthalmol Soc. 1999; 40:652–6.25. Hartikainen J, Lehtonen OP, Saari KM. Bacteriology of lacrimal duct obstruction in adults. Br J Ophthalmol. 1997; 81:37–40.
Article26. Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 3. Ophthal Plast Reconstr Surg. 1993; 9:11–26.27. Purgason PA, Hornblass A, Loeffler M. Atypical presentation of fungal dacryocystitis. A report of two cases. Ophthalmology. 1992; 99:1430–2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Observation on Nasolacrimal Duct Stent Intubation in Obstruction of Nasolacrimal System
- Long-term Outcome of Nasolacrimal Duct Obstruction Treated with Nasolacrimal Polyurethane Stents (Song's Stent)
- Clinicopathologic Findings after Nasolacrimal Polyurethane Stent Implantations
- Results with Silicone Stent in Lacrimal Drainage System
- Nasolacrimal Duct Stent Insertion: Causes of Insertion Failure and Reobstruction