J Korean Ophthalmol Soc.
2015 Mar;56(3):452-457. 10.3341/jkos.2015.56.3.452.
A Case of Atypical Acute Retinal Necrosis Observed Using Ultra-Wide-Field Imaging
- Affiliations
-
- 1Department of Ophthalmology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. eyekim@kuh.ac.kr
- KMID: 2339055
- DOI: http://doi.org/10.3341/jkos.2015.56.3.452
Abstract
- PURPOSE
To Report A Case Of Atypical Acute Retinal Necrosis (Arn) Observed Using Ultra-wide-field Imaging.
CASE SUMMARY
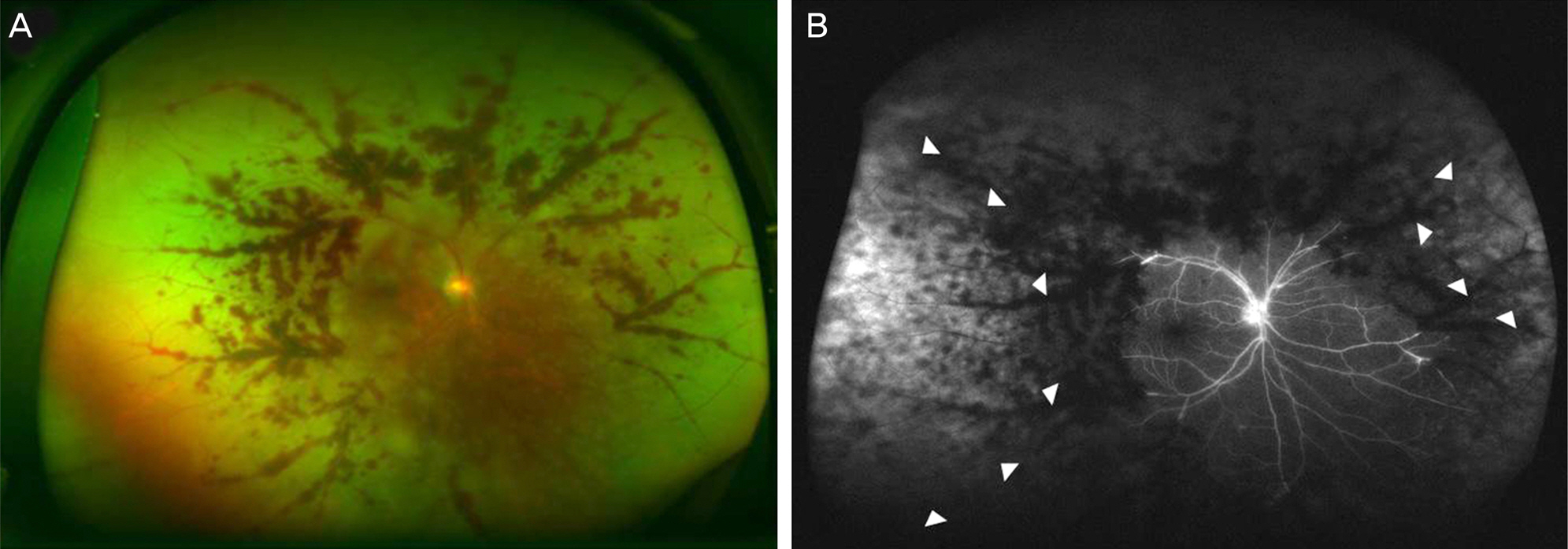
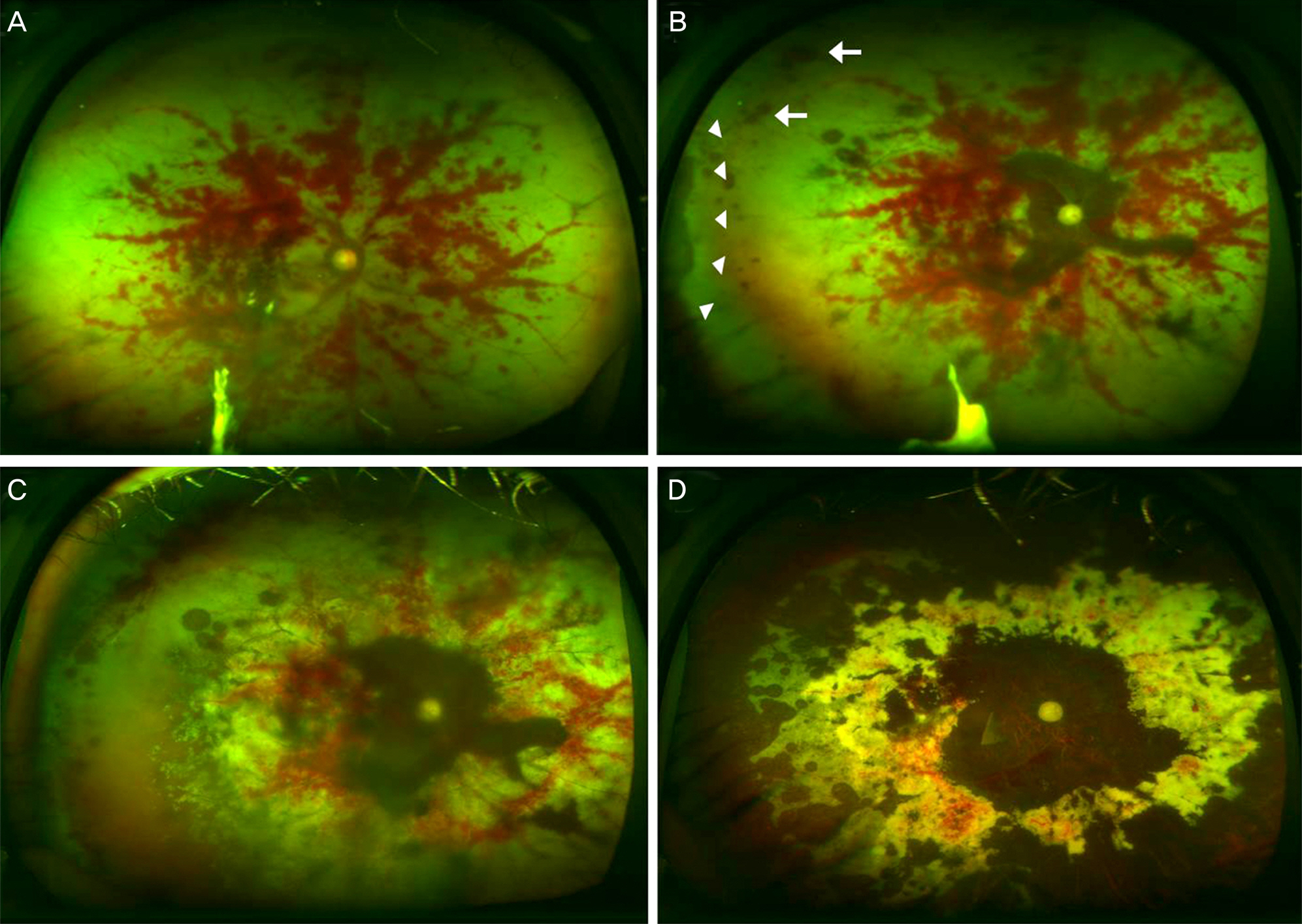
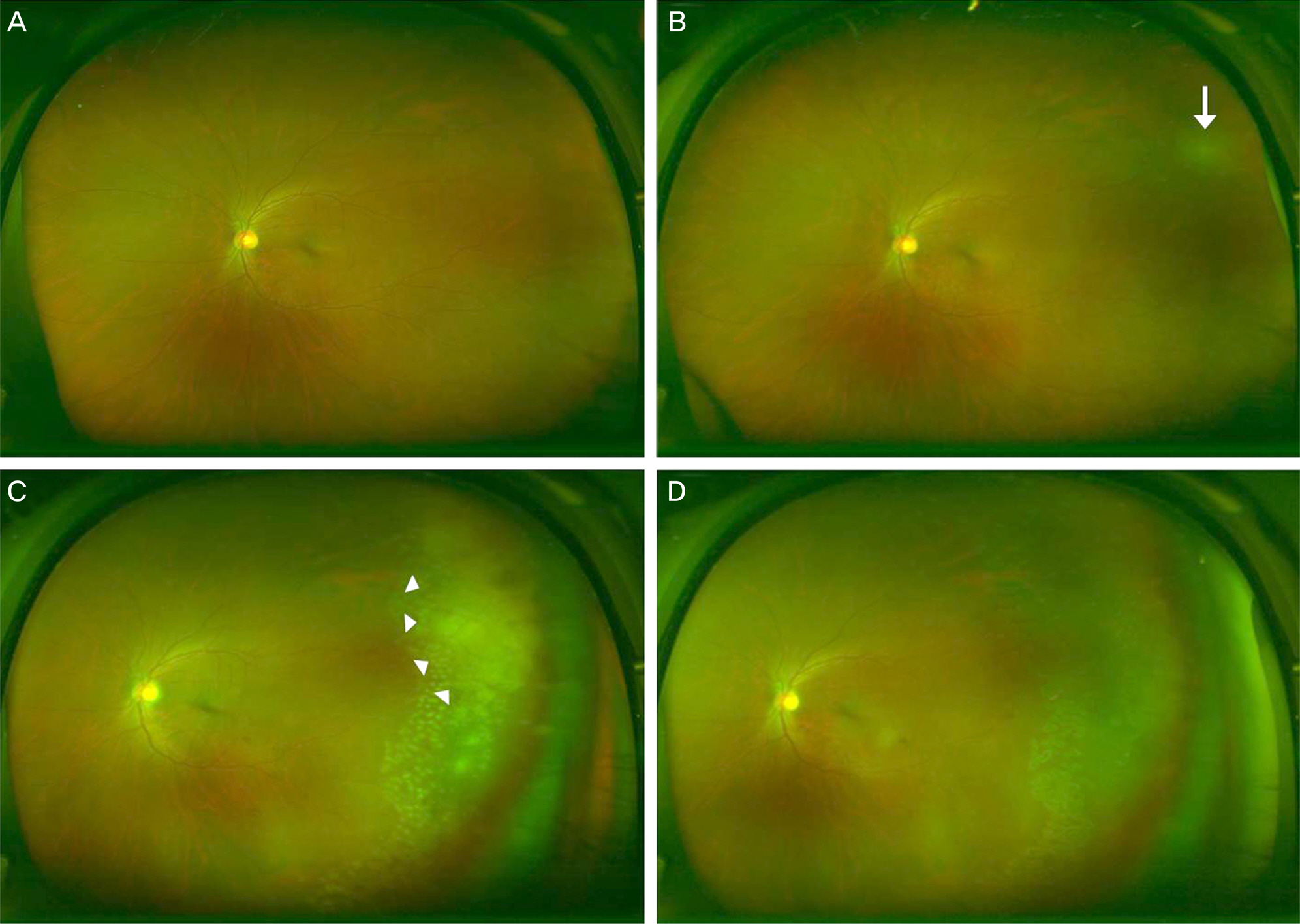
A 50-year-old male with recurrent oral ulcer presented with visual loss in his right eye. On the initial visit, slit-lamp examination showed inflammatory cells (3+) in the anterior chamber and vitreous of the right eye. Funduscopic examination and ultra-wide-field fundus images showed severe occlusive vasculitis with perivascular hemorrhage. No necrotic lesion was observed at the peripheral retina in the left eye. Under the impression of Behcet's uveitis, immunosuppressive therapies including oral steroid, intravenous cyclophosphamide, anti-tumor necrosis factor (TNF) alpha agent and intravitreal triamcinolone were administered, but without improvement. Subsequently, a necrotic lesion appeared at the far peripheral retina in the right eye and varicella-zoster virus was identified using the polymerase chain reaction test. After the patient was diagnosed with atypical ARN, intravenous acyclovir was administered, resulting in eventual suppression of the necrotic lesion progression. Due to retinal detachment, pars plana vitrectomy with silicone oil infusion was performed in the right eye. At that time, a whitish lesion at the far peripheral retina in the ultra-wide-field photography of the fellow eye was found and 3 intravitreal ganciclovir injections were administered. Finally, the whitish lesion regressed after 1 month.
CONCLUSIONS
Ultra-wide-field imaging might be useful for diagnosis and follow-up of atypical ARN patients.
Keyword
MeSH Terms
-
Acyclovir
Anterior Chamber
Cyclophosphamide
Diagnosis
Ganciclovir
Hemorrhage
Herpesvirus 3, Human
Humans
Male
Middle Aged
Necrosis
Oral Ulcer
Photography
Polymerase Chain Reaction
Retina
Retinal Detachment
Retinal Necrosis Syndrome, Acute*
Silicone Oils
Triamcinolone
Uveitis
Vasculitis
Vitrectomy
Acyclovir
Cyclophosphamide
Ganciclovir
Silicone Oils
Triamcinolone
Figure
Reference
-
References
1. Urayama A, Yamada N, Sasaki T, et al. Unilateral acute uveitis with retinal periarteritis and detachment. Jpn J Clin Ophthalmol. 1971; 25:607–19.2. Usui Y, Goto H. Overview and diagnosis of acute retinal necrosis syndrome. Semin Ophthalmol. 2008; 23:275–83.
Article3. Walters G, James TE. Viral causes of the acute retinal necrosis syndrome. Curr Opin Ophthalmol. 2001; 12:191–5.
Article4. Tugal-Tutkun I, Gupta V, Cunningham ET. Differential diagnosis of behçet uveitis. Ocul Immunol Inflamm. 2013; 21:337–50.
Article5. Wessel MM, Aaker GD, Parlitsis G, et al. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2012; 32:785–91.
Article6. Prasad PS, Oliver SC, Coffee RE, et al. Ultra wide-field angio-graphic characteristics of branch retinal and hemicentral retinal vein occlusion. Ophthalmology. 2010; 117:780–4.
Article7. Tsui I, Kaines A, Havunjian MA, et al. Ischemic index and neovascularization in central retinal vein occlusion. Retina. 2011; 31:105–10.
Article8. Kaines A, Tsui I, Sarraf D, Schwartz S. The use of ultra wide field fluorescein angiography in evaluation and management of uveitis. Semin Ophthalmol. 2009; 24:19–24.
Article9. Anderson L, Friberg TR, Singh J. Ultrawide-angle retinal imaging and retinal detachment. Semin Ophthalmol. 2007; 22:43–7.
Article10. Clarkson JG, Blumenkranz MS, Culbertson WW, et al. Retinal detachment following the acute retinal necrosis syndrome. Ophthalmology. 1984; 91:1665–8.
Article11. Holland GN. Standard diagnostic criteria for the acute retinal necrosis syndrome. Executive Committee of the American Uveitis Society. Am J Ophthalmol. 1994; 117:663–7.12. Neubauer AS, Yu A, Haritoglou C, Ulbig MW. Peripheral retinal changes in acute retinal necrosis imaged by ultra widefield scanning laser ophthalmoscopy. Acta Ophthalmol Scand. 2005; 83:758–60.
Article13. Wensing B, de Groot-Mijnes JD, Rothova A. Necrotizing and nonnecrotizing variants of herpetic uveitis with posterior segment involvement. Arch Ophthalmol. 2011; 129:403–8.
Article14. Khairallah M, Accorinti M, Muccioli C, et al. Epidemiology of Behçet disease. Ocul Immunol Inflamm. 2012; 20:324–35.
Article15. Park JW, Koh HJ, Kim HB. Behcet's Disease in Korean. J Korean Ophthalmol Soc. 2002; 43:67–74.16. Bodaghi B, Rozenberg F, Cassoux N, et al. Nonnecrotizing herpetic retinopathies masquerading as severe posterior uveitis. Ophthalmology. 2003; 110:1737–43.
Article17. Tran TH, Rozenberg F, Cassoux N, et al. Polymerase chain reaction analysis of aqueous humour samples in necrotising retinitis. Br J Ophthalmol. 2003; 87:79–83.
Article18. Palay DA, Sternberg P Jr, Davis J, et al. Decrease in the risk of bilateral acute retinal necrosis by acyclovir therapy. Am J Ophthalmol. 1991; 112:250–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Availability of Ultra-Wide-field Fundus Imaging in Korean Patient with Retinal Break
- Ultra-wide Field Fundus Photography Using Eye Steering Technique in Patients with Symptomatic Posterior Vitreous Detachment
- The Extent of Silicone Oil Emulsification Revealed by Ultra-wide-field Fundus Photography and Optical Coherence Tomography
- The Characteristics of Non-Retinal Lesions in the Ultra-Wide Field Scanning Laser Ophthalmoscope Image
- Primary Choroidal Inflammation and Early Retinal Detachment in Acute Retinal Necrosis: Case Report