J Korean Ophthalmol Soc.
2015 Mar;56(3):438-442. 10.3341/jkos.2015.56.3.438.
A Case of Alternaria Species Infection after Corneal Tattooing
- Affiliations
-
- 1Department of Ophthalmology, Dankook University Medical College, Cheonan, Korea. perfectcure@hanmail.net
- KMID: 2339052
- DOI: http://doi.org/10.3341/jkos.2015.56.3.438
Abstract
- PURPOSE
To report a case of successful treatment of Alternaria species infection after corneal tattooing using penetrating keratoplasty corneal perforation.
CASE SUMMARY
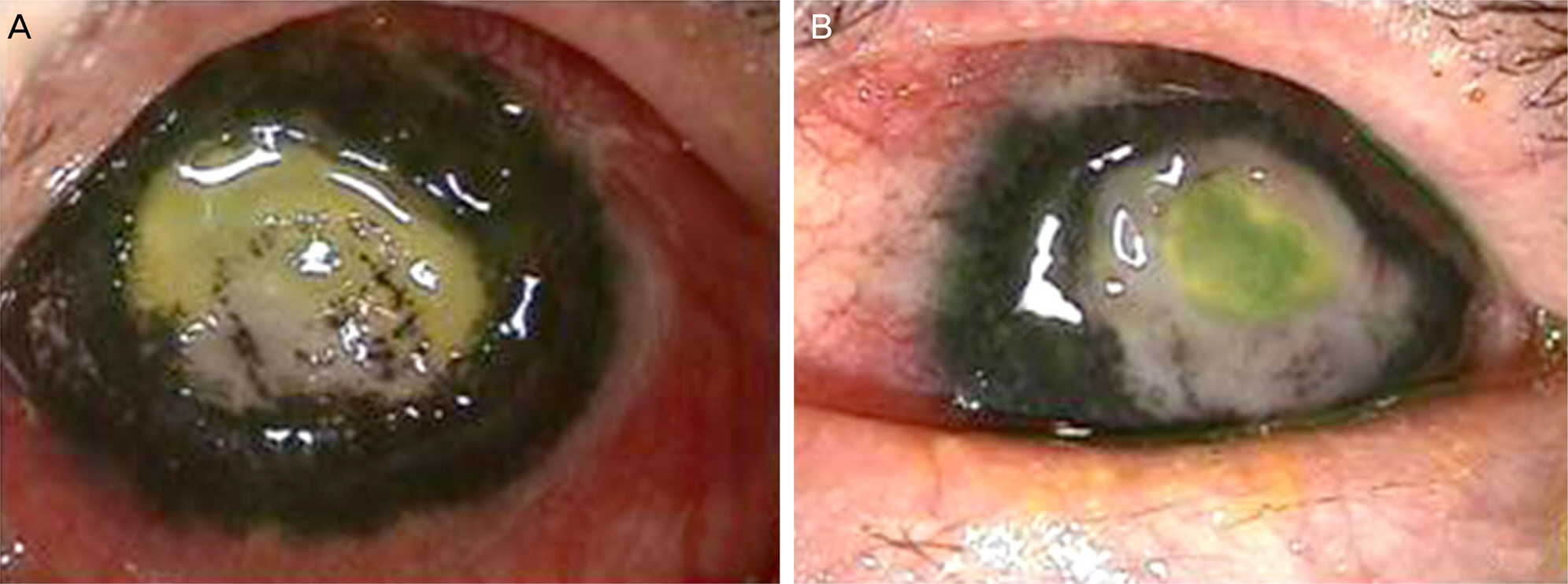
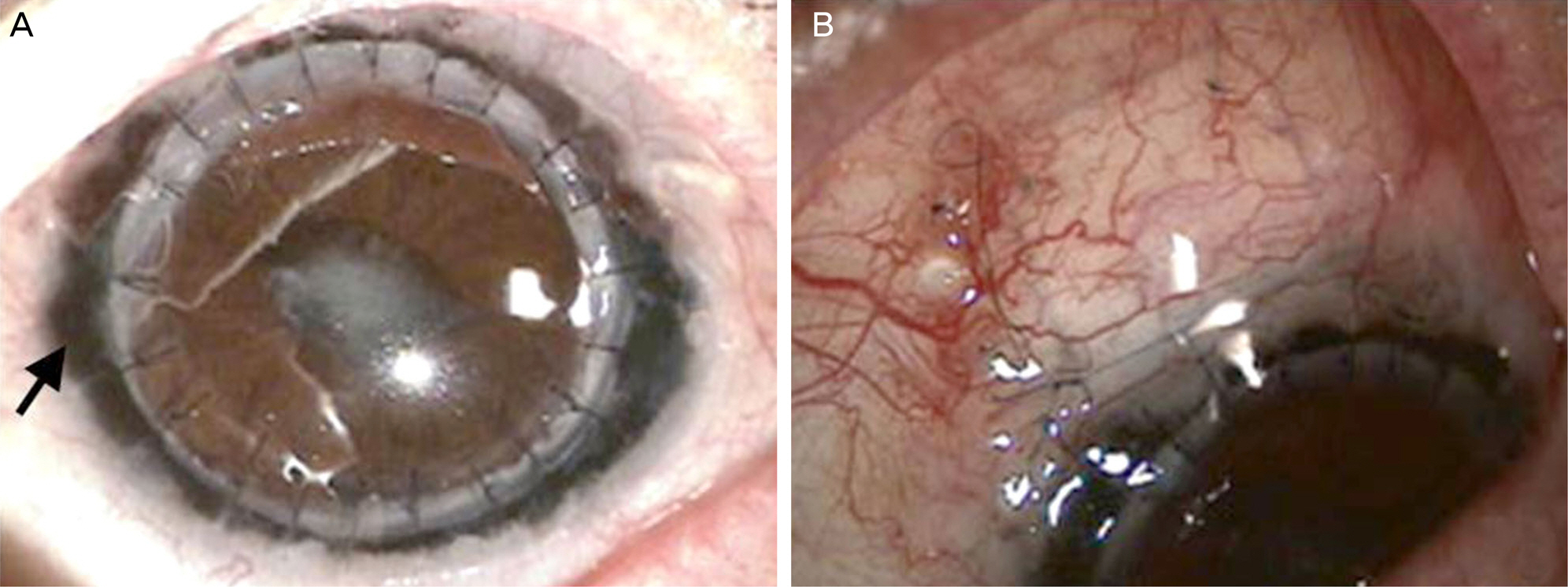
A 65-year-old male underwent corneal tattooing for corneal opacity of the left eye. One month later, epithelial defect and necrosis of the left eye were observed, thus a smear and culture were performed and Alternaria species were cultured. He was treated with 0.3% amphotericin B-fortified eyedrops and Itraconazole oral medication; however, 3 weeks later, corneal perforation of the left eye was observed and penetrating keratoplasty was performed. Postoperatively, due to persistent increased intraocular pressure, trabeculectomy was performed. Two months later, donor cornea was well-grafted and recurrent keratitis was not observed.
CONCLUSIONS
Corneal tattooing can cause damage to the corneal epithelium and anterior stroma and increase the risk of infection when using steroids. In the case of infection, detecting and differentiating the type of microorganisms are more difficult. Therefore, proper care and close monitoring for the signs of infection are important during and after the surgery.
MeSH Terms
Figure
Reference
-
References
1. Kim C, Han YK, Wee WR, et al. Cosmetic repair of corneal opacity by tattooing. J Korean Ophthalmol Soc. 2005; 46:1967–73.2. Mannis MJ, Eghbali K, Schwab IR. Keratopigmentation: a review of corneal tattooing. Cornea. 1999; 18:633–7.3. van der Velden/Samderubun EM, Kok JH. Dermatography as a modern treatment for coloring leucoma corneae. Cornea. 1994; 13:349–53.
Article4. Khan AO, Meyer D. Corneal tattooing for the treatment of debili-tating glare in a child with traumatic iris loss. Am J Ophthalmol. 2005; 139:920–1.
Article5. Leigh AG. Tattooing of the cornea. Duke-Elder S, editor. System of Ophthalmology. London: Henry Kimpton;1965. p. 645–8.6. Olander K, Kanai A, Kaufman HE. An analytical electron microscopic study of a corneal tattoo. Ann Ophthalmol. 1983; 15:1046–9.7. Sekundo W, Seifert P, Seitz B, Loeffler KU. Long-term ultra-structural changes in human corneas after tattooing with non-met-allic substances. Br J Ophthalmol. 1999; 83:219–24.8. Lee JE, Lee SU, Kim JH, et al. Corneal tattooing to mask the opacification after amniotic membrane grafting for corneal ulcer. J Korean Ophthalmol Soc. 2006; 47:1491–5.9. Panda A, Mohan M, Chawdhary S. Corneal tattooing--experiences with "lamellar pocket procedure". Indian J Ophthalmol. 1984; 32:408–11.10. Pitz S, Jahn R, Frisch L, et al. Corneal tattooing: an alternative treatment for disfiguring corneal scars. Br J Ophthalmol. 2002; 86:397–9.
Article11. Kim JH, Lee D, Hahn TW, Choi SK. New surgical strategy for corneal tattooing using a femtosecond laser. Cornea. 2009; 28:80–4.
Article12. Hahn YH, Lee DJ, Kim MS, et al. Epidemiology of fungal keratitis in Korea: A multi-center study. J Korean Ophthalmol Soc. 2000; 41:1499–508.13. You IC, Kang IS, Yoon KC. Clinical aspect and prognosis of alternaria keratitis. J Korean Ophthalmol Soc. 2007; 48:478–84.14. Verma K, Vajpayee RB, Titiyal JS, et al. Post-LASIK infectious crystalline keratopathy caused by Alternaria. Cornea. 2005; 24:1018–20.
Article15. Rummelt V, Ruprecht KW, Boltze HJ, Naumann GO. Chronic Alternaria alternata endophthalmitis following intraocular lens implantation. Arch Ophthalmol. 1991; 109:178.
Article16. Sharkey PK, Graybill JR, Rinaldi MG, et al. Itraconazole treatment of phaeohyphomycosis. J Am Acad Dermatol. 1990; 23:577–86.
Article17. Jonas JB, Rank RM, Budde WM. Tectonic sclerokeratoplasty and tectonic penetrating keratoplasty as treatment for perforated or pre-descemetal corneal ulcers. Am J Ophthalmol. 2001; 132:14–8.
Article18. Rodriguez-Ares T, De Rojas Silva V, Ferreiros MP, et al. Acremonium keratitis in a patient with herpetic neurotrophic corneal disease. Acta Ophthalmol Scand. 2000; 78:107–9.
Article19. Boisjoly HM, Pavan-Langston D, Kenyon KR, Baker AS. Superinfections in herpes simplex keratitis. Am J Ophthalmol. 1983; 96:354–61.
Article20. Goldberg DB, Schanzlin DJ, Brown SI. Incidence of increased intraocular pressure after keratoplasty. Am J Ophthalmol. 1981; 92:372–7.
Article21. Jeong IY, You IC, Park YG, Yoon KC. Effect of tectonic penetrating keratoplasty for impending perforation due to infectious corneal ulcer. J Korean Ophthalmol Soc. 2007; 48:883–8.22. Kim M, Oh JY, Kim MK, et al. Clinical manifestation and predis-posing factors of infectious keratitis following penetrating keratoplasty in Korean patients. J Korean Ophthalmol Soc. 2010; 51:504–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Infectious Crystalline Keratopathy Caused by Alternaria
- Taxonomic Studies on Alternaria in Korea (1)
- Two Cases of Glare after Iridotomy for Phakic Intraocular Lens Implantation
- Corneal Tattooing to Mask the Opacification after Amniotic Membrane Grafting for Corneal Ulcer
- Tattooing of the Cornea with Platinum Chloride