J Periodontal Implant Sci.
2013 Dec;43(6):262-268.
Photobiomodulation and implants: implications for dentistry
- Affiliations
-
- 1Cell Regulation and Control Unit, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD, USA. praveen.arany@nih.gov
Abstract
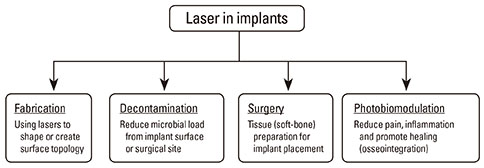
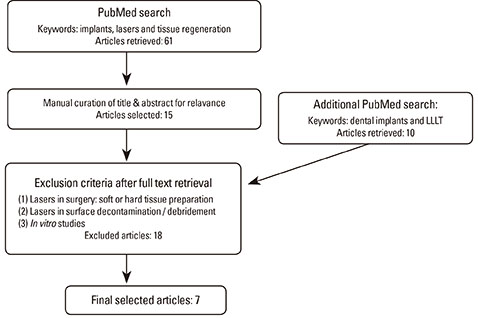
- The use of dental implants has become a mainstay of rehabilitative and restorative dentistry. With an impressive clinical success rate, there remain a few minor clinical issues with the use of implants such as peri-implant mucositis and peri-implantitis. The use of laser technology with implants has a fascinating breadth of applications, beginning from their precision manufacturing to clinical uses for surgical site preparation, reducing pain and inflammation, and promoting osseointegration and tissue regeneration. This latter aspect is the focus of this review, which outlines various studies of implants and laser therapy in animal models. The use of low level light therapy or photobiomodulation has demonstrated its efficacy in these studies. Besides more research studies to understand its molecular mechanisms, significant efforts are needed to standardize the clinical dosing and delivery protocols for laser therapy to ensure the maximal efficacy and safety of this potent clinical tool for photobiomodulation.
MeSH Terms
Figure
Reference
-
1. Peplow PV, Chung TY, Ryan B, Baxter GD. Laser photobiomodulation of gene expression and release of growth factors and cytokines from cells in culture: a review of human and animal studies. Photomed Laser Surg. 2011; 29:285–304.
Article2. Kim YD, Kim SS, Hwang DS, Kim SG, Kwon YH, Shin SH, et al. Effect of low-level laser treatment after installation of dental titanium implant-immunohistochemical study of RANKL, RANK, OPG: an experimental study in rats. Lasers Surg Med. 2007; 39:441–450.
Article3. Mester E, Mester AF, Mester A. The biomedical effects of laser application. Lasers Surg Med. 1985; 5:31–39.
Article4. Hahm E, Kulhari S, Arany PR. Targeting the pain, inflammation and immune (PII) axis: plausible rationale for LLLT. Photonics Lasers Med. 2012; 1:241–254.
Article5. Arany PR, Nayak RS, Hallikerimath S, Limaye AM, Kale AD, Kondaiah P. Activation of latent TGF-beta1 by low-power laser in vitro correlates with increased TGF-beta1 levels in laser-enhanced oral wound healing. Wound Repair Regen. 2007; 15:866–874.
Article6. Thalji G, Cooper LF. Molecular assessment of osseointegration in vivo: a review of the current literature. Int J Oral Maxillofac Implants. 2013; 28:e521–e534.
Article7. Peri-implant mucositis and peri-implantitis: a current understanding of their diagnoses and clinical implications. J Periodontol. 2013; 84:436–443.8. Badran Z, Bories C, Struillou X, Saffarzadeh A, Verner C, Soueidan A. Er: YAG laser in the clinical management of severe peri-implantitis: a case report. J Oral Implantol. 2011; 37(Spec No):212–217.
Article9. Lang NP, Berglundh T. Working Group 4 of Seventh European Workshop on Periodontology. Periimplant diseases: where are we now? Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol. 2011; 38:Suppl 11. 178–181.
Article10. Arnabat-Dominguez J, Bragado-Novel M, Espana-Tost AJ, Berini-Aytes L, Gay-Escoda C. Advantages and esthetic results of erbium, chromium: yttrium-scandium-gallium-garnet laser application in second-stage implant surgery in patients with insufficient gingival attachment: a report of three cases. Lasers Med Sci. 2010; 25:459–464.
Article11. Botos S, Yousef H, Zweig B, Flinton R, Weiner S. The effects of laser microtexturing of the dental implant collar on crestal bone levels and peri-implant health. Int J Oral Maxillofac Implants. 2011; 26:492–498.12. Guzzardella GA, Torricelli P, Nicoli Aldini N, Giardino R. Laser technology in orthopedics: preliminary study on low power laser therapy to improve the bone-biomaterial interface. Int J Artif Organs. 2001; 24:898–902.
Article13. Lopes CB, Pinheiro AL, Sathaiah S, Da Silva NS, Salgado MA. Infrared laser photobiomodulation (lambda 830 nm) on bone tissue around dental implants: a Raman spectroscopy and scanning electronic microscopy study in rabbits. Photomed Laser Surg. 2007; 25:96–101.
Article14. Campanha BP, Gallina C, Geremia T, Loro RC, Valiati R, Hubler R, et al. Low-level laser therapy for implants without initial stability. Photomed Laser Surg. 2010; 28:365–369.
Article15. Bengtson AL, Bengtson NG, Bengtson CR, Mendes FM, Pinheiro SR. Histological and radiographic evaluation of the muscle tissue of rats after implantation of bone morphogenic protein (rhBMP-2) in a scaffold of inorganic bone and after stimulation with low-power laser light. Indian J Dent Res. 2010; 21:420–424.
Article16. Pinto MR, dos Santos RL, Pithon MM, Araujo MT, Braga JP, Nojima LI. Influence of low-intensity laser therapy on the stability of orthodontic mini-implants: a study in rabbits. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 115:e26–e30.17. Favero LG, Pisoni A, Paganelli C. Removal torque of osseointegrated mini-implants: an in vivo evaluation. Eur J Orthod. 2007; 29:443–448.
Article18. Dortbudak O, Haas R, Mailath-Pokorny G. Effect of low-power laser irradiation on bony implant sites. Clin Oral Implants Res. 2002; 13:288–292.
Article19. Maluf AP, Maluf RP, Brito Cda R, Franca FM, de Brito RB Jr. Mechanical evaluation of the influence of low-level laser therapy in secondary stability of implants in mice shinbones. Lasers Med Sci. 2010; 25:693–698.
Article20. Simmons D. The use of animal models in studying genetic disease: transgenesis and induced mutation. Nature Educ. 2008; 1:70.21. Mapara M, Thomas BS, Bhat KM. Rabbit as an animal model for experimental research. Dent Res J (Isfahan). 2012; 9:111–118.
Article22. Wang X, Mabrey JD, Agrawal CM. An interspecies comparison of bone fracture properties. Biomed Mater Eng. 1998; 8:1–9.23. VandeBerg JL, Williams-Blangero S. Advantages and limitations of nonhuman primates as animal models in genetic research on complex diseases. J Med Primatol. 1997; 26:113–119.
Article24. Nguyen D, Xu T. The expanding role of mouse genetics for understanding human biology and disease. Dis Model Mech. 2008; 1:56–66.
Article25. Fell HB. Tissue culture and its contribution to biology and medicine. J Exp Biol. 1972; 57:1–13.
Article26. Khadra M, Kasem N, Lyngstadaas SP, Haanaes HR, Mustafa K. Laser therapy accelerates initial attachment and subsequent behaviour of human oral fibroblasts cultured on titanium implant material: a scanning electron microscope and histomorphometric analysis. Clin Oral Implants Res. 2005; 16:168–175.
Article27. Dortbudak O, Haas R, Mallath-Pokorny G. Biostimulation of bone marrow cells with a diode soft laser. Clin Oral Implants Res. 2000; 11:540–545.
Article28. Schenk RK, Buser D. Osseointegration: a reality. Periodontol 2000. 1998; 17:22–35.
Article29. Gilbert GH, Williams OD, Rindal DB, Pihlstrom DJ, Benjamin PL, Wallace MC, et al. The creation and development of the dental practice-based research network. J Am Dent Assoc. 2008; 139:74–81.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Does photobiomodulation on the root surface decrease the occurrence of root resorption in reimplanted teeth? A systematic review of animal studies
- Lightening up Light Therapy: Activation of Retrograde Signaling Pathway by Photobiomodulation
- Photobiomodulation Therapy in the Treatment of Salivary Dysfunction
- Appraisal of Recent Developments in Combined Photodynamic Treatment (PDT)/Photobiomodulation (PBM) for Dermal Wound Healing
- A review on photobiomodulation therapy for olfactory dysfunction caused by COVID-19