Restor Dent Endod.
2023 Aug;48(3):e24. 10.5395/rde.2023.48.e24.
Does photobiomodulation on the root surface decrease the occurrence of root resorption in reimplanted teeth? A systematic review of animal studies
- Affiliations
-
- 1Department of Conservative Dentistry, School of Dentistry, Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil
- 2Department of Restorative Dentistry, School of Dentistry, University of Passo Fundo, Passo Fundo, RS, Brazil
- KMID: 2548227
- DOI: http://doi.org/10.5395/rde.2023.48.e24
Abstract
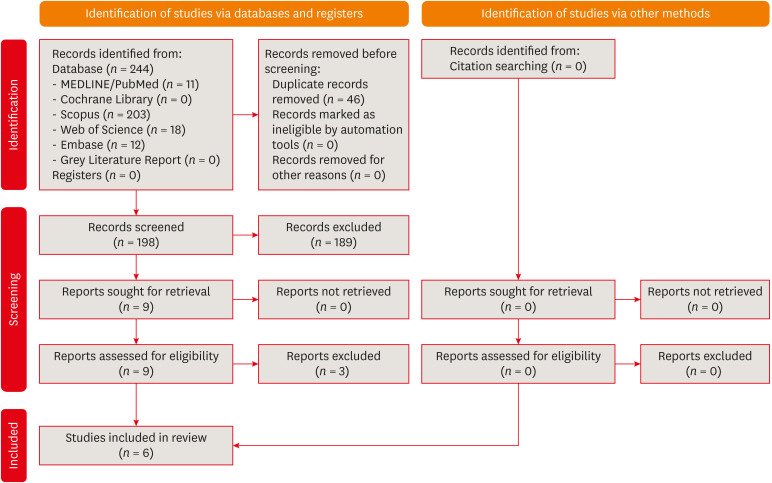
- This review aimed to answer the following question “Does photobiomodulation treatment of the root surface decrease the occurrence of root resorption in reimplanted teeth?” Electronic searches were performed in the MEDLINE/PubMed, Cochrane Library, Scopus, Web of Science, Embase, and Grey Literature Report databases. Risk of bias was evaluated using SYRCLE Risk of Bias tool. The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) tool was used to assess the certainty of evidence. In total, 6 studies were included. Five studies reported a reduced occurrence of root resorption in teeth that received photobiomodulation treatment of the root surface prior to replantation. Only 1 study reported contradictory results. The photobiomodulation parameters varied widely among studies. GRADE assessment showed a low certainty of evidence. It can be inferred that photobiomodulation treatment of the root surface prior to replantation of teeth can reduce the occurrence of root resorption. Nonetheless, further clinical studies are needed. Trial Registration: PROSPERO Identifier: CRD42022349891
Figure
Reference
-
1. Levin L, Day PF, Hicks L, O’Connell A, Fouad AF, Bourguignon C, Abbott PV. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: general introduction. Dent Traumatol. 2020; 36:309–313. PMID: 32472740.
Article2. Petti S, Glendor U, Andersson L. World traumatic dental injury prevalence and incidence, a meta-analysis-one billion living people have had traumatic dental injuries. Dent Traumatol. 2018; 34:71–86. PMID: 29455471.
Article3. Antunes LA, Lemos HM, Milani AJ, Guimarães LS, Küchler EC, Antunes LS. Does traumatic dental injury impact oral health-related to quality of life of children and adolescents? Systematic review and meta-analysis. Int J Dent Hyg. 2020; 18:142–162. PMID: 31828930.
Article4. Corrêa-Faria P, Martins CC, Bönecker M, Paiva SM, Ramos-Jorge ML, Pordeus IA. Clinical factors and socio-demographic characteristics associated with dental trauma in children: a systematic review and meta-analysis. Dent Traumatol. 2016; 32:367–378. PMID: 26990348.
Article5. Magno MB, Nadelman P, Leite KL, Ferreira DM, Pithon MM, Maia LC. Associations and risk factors for dental trauma: a systematic review of systematic reviews. Community Dent Oral Epidemiol. 2020; 48:447–463. PMID: 32893395.
Article6. Vieira WA, Pecorari VG, Gabriel PH, Vargas-Neto J, Santos EC, Gomes BP, Ferraz CC, Almeida JF, Marciano M, de-Jesus-Soares A. The association of inadequate lip coverage and malocclusion with dental trauma in Brazilian children and adolescents - a systematic review and meta-analysis. Dent Traumatol. 2022; 38:4–19. PMID: 34275184.
Article7. Fouad AF, Abbott PV, Tsilingaridis G, Cohenca N, Lauridsen E, Bourguignon C, O’Connell A, Flores MT, Day PF, Hicks L, Andreasen JO, Cehreli ZC, Harlamb S, Kahler B, Oginni A, Semper M, Levin L. International Association of Dental Traumatology. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent Traumatol. 2020; 36:331–342. PMID: 32460393.
Article8. Souza BD, Dutra KL, Kuntze MM, Bortoluzzi EA, Flores-Mir C, Reyes-Carmona J, Felippe WT, Porporatti AL, De Luca Canto G. Incidence of root resorption after the replantation of avulsed teeth: a meta-analysis. J Endod. 2018; 44:1216–1227. PMID: 29866405.
Article9. Andreasen JO. Relationship between surface and inflammatory resorption and changes in the pulp after replantation of permanent incisors in monkeys. J Endod. 1981; 7:294–301. PMID: 6942086.
Article10. Andreasen JO, Kristerson L. The effect of limited drying or removal of the periodontal ligament. Periodontal healing after replantation of mature permanent incisors in monkeys. Acta Odontol Scand. 1981; 39:1–13. PMID: 6943904.11. Andreasen JO. Periodontal healing after replantation of traumatically avulsed human teeth: assessment by mobility testing and radiography. Acta Odontol Scand. 2009; 33:325–333.
Article12. Fuss Z, Tsesis I, Lin S. Root resorption--diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003; 19:175–182. PMID: 12848710.
Article13. Andreasen JO, Storgaard Jensen S, Sae-Lim V. The role of antibiotics in presenting healing complications after traumatic dental injuries: a literature review. Endod Topics. 2006; 14:80–92.
Article14. Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Robles Aguilar G, Gray A, Han C, Bisignano C, Rao P, Wool E, Johnson SC, Browne AJ, Chipeta MG, Fell F, Hackett S, Haines-Woodhouse G, Kashef Hamadani BH, Kumaran EA, McManigal B, Achalapong S, Agarwal R, Akech S, Albertson S, Amuasi J, Andrews J, Aravkin A, Ashley E, Babin FX, Bailey F, Baker S, Basnyat B, Bekker A, Bender R, Berkley JA, Bethou A, Bielicki J, Boonkasidecha S, Bukosia J, Carvalheiro C, Castañeda-Orjuela C, Chansamouth V, Chaurasia S, Chiurchiù S, Chowdhury F, Clotaire Donatien R, Cook AJ, Cooper B, Cressey TR, Criollo-Mora E, Cunningham M, Darboe S, Day NP, De Luca M, Dokova K, Dramowski A, Dunachie SJ, Duong Bich T, Eckmanns T, Eibach D, Emami A, Feasey N, Fisher-Pearson N, Forrest K, Garcia C, Garrett D, Gastmeier P, Giref AZ, Greer RC, Gupta V, Haller S, Haselbeck A, Hay SI, Holm M, Hopkins S, Hsia Y, Iregbu KC, Jacobs J, Jarovsky D, Javanmardi F, Jenney AW, Khorana M, Khusuwan S, Kissoon N, Kobeissi E, Kostyanev T, Krapp F, Krumkamp R, Kumar A, Kyu HH, Lim C, Lim K, Limmathurotsakul D, Loftus MJ, Lunn M, Ma J, Manoharan A, Marks F, May J, Mayxay M, Mturi N, Munera-Huertas T, Musicha P, Musila LA, Mussi-Pinhata MM, Naidu RN, Nakamura T, Nanavati R, Nangia S, Newton P, Ngoun C, Novotney A, Nwakanma D, Obiero CW, Ochoa TJ, Olivas-Martinez A, Olliaro P, Ooko E, Ortiz-Brizuela E, Ounchanum P, Pak GD, Paredes JL, Peleg AY, Perrone C, Phe T, Phommasone K, Plakkal N, Ponce-de-Leon A, Raad M, Ramdin T, Rattanavong S, Riddell A, Roberts T, Robotham JV, Roca A, Rosenthal VD, Rudd KE, Russell N, Sader HS, Saengchan W, Schnall J, Scott JA, Seekaew S, Sharland M, Shivamallappa M, Sifuentes-Osornio J, Simpson AJ, Steenkeste N, Stewardson AJ, Stoeva T, Tasak N, Thaiprakong A, Thwaites G, Tigoi C, Turner C, Turner P, van Doorn HR, Velaphi S, Vongpradith A, Vongsouvath M, Vu H, Walsh T, Walson JL, Waner S, Wangrangsimakul T, Wannapinij P, Wozniak T, Young Sharma TE, Yu KC, Zheng P, Sartorius B, Lopez AD, Stergachis A, Moore C, Dolecek C, Naghavi M. Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022; 399:629–655. PMID: 35065702.
Article15. Lam K, Sae-Lim V. The effect of Emdogain gel on periodontal healing in replanted monkeys’ teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 97:100–107. PMID: 14716264.
Article16. Lustosa-Pereira A, Garcia RB, de Moraes IG, Bernardineli N, Bramante CM, Bortoluzzi EA. Evaluation of the topical effect of alendronate on the root surface of extracted and replanted teeth. Microscopic analysis on rats’ teeth. Dent Traumatol. 2006; 22:30–35. PMID: 16422756.
Article17. Gulinelli JL, Panzarini SR, Fattah CM, Poi WR, Sonoda CK, Negri MR, Saito CT. Effect of root surface treatment with propolis and fluoride in delayed tooth replantation in rats. Dent Traumatol. 2008; 24:651–657. PMID: 18721196.
Article18. Schwarz F, Pütz N, Georg T, Reich E. Effect of an Er:YAG laser on periodontally involved root surfaces: an in vivo and in vitro SEM comparison. Lasers Surg Med. 2001; 29:328–335. PMID: 11746110.
Article19. Feist IS, De Micheli G, Carneiro SR, Eduardo CP, Miyagi S, Marques MM. Adhesion and growth of cultured human gingival fibroblasts on periodontally involved root surfaces treated by Er:YAG laser. J Periodontol. 2003; 74:1368–1375. PMID: 14584872.
Article20. Hakki SS, Korkusuz P, Berk G, Dundar N, Saglam M, Bozkurt B, Purali N. Comparison of Er,Cr:YSGG laser and hand instrumentation on the attachment of periodontal ligament fibroblasts to periodontally diseased root surfaces: an in vitro study. J Periodontol. 2010; 81:1216–1225. PMID: 20476883.
Article21. Kreisler M, Kohnen W, Beck M, Al Haj H, Christoffers AB, Götz H, Duschner H, Jansen B, D’Hoedt B. Efficacy of NaOCl/H2O2 irrigation and GaAlAs laser in decontamination of root canals in vitro . Lasers Surg Med. 2003; 32:189–196. PMID: 12605425.
Article22. de Souza EB, Cai S, Simionato MR, Lage-Marques JL. High-power diode laser in the disinfection in depth of the root canal dentin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:e68–e72. PMID: 18585615.
Article23. Akiyama F, Aoki A, Miura-Uchiyama M, Sasaki KM, Ichinose S, Umeda M, Ishikawa I, Izumi Y. In vitro studies of the ablation mechanism of periodontopathic bacteria and decontamination effect on periodontally diseased root surfaces by erbium:yttrium-aluminum-garnet laser. Lasers Med Sci. 2011; 26:193–204. PMID: 20309597.
Article24. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71. PMID: 33782057.
Article25. Maia LC, Antonio AG. Systematic reviews in dental research. A guideline. J Clin Pediatr Dent. 2012; 37:117–124. PMID: 23534316.
Article26. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. PRISMA-P Group. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015; 4:1. PMID: 25554246.
Article27. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann T, Mulrow CD, Shamseer L, Moher D. Mapping of reporting guidance for systematic reviews and meta-analyses generated a comprehensive item bank for future reporting guidelines. J Clin Epidemiol. 2020; 118:60–68. PMID: 31740319.
Article28. Hooijmans CR, Rovers MM, de Vries RB, Leenaars M, Ritskes-Hoitinga M, Langendam MW. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014; 14:43. PMID: 24667063.
Article29. Hooijmans CR, de Vries RBM, Ritskes-Hoitinga M, Rovers MM, Leeflang MM, IntHout J, Wever KE, Hooft L, de Beer H, Kuijpers T, Macleod MR, Sena ES, Ter Riet G, Morgan RL, Thayer KA, Rooney AA, Guyatt GH, Schünemann HJ, Langendam MW. GRADE Working Group. Facilitating healthcare decisions by assessing the certainty in the evidence from preclinical animal studies. PLoS One. 2018; 13:e0187271. PMID: 29324741.
Article30. Friedman S, Komorowski R, Maillet W, Nguyen HQ, Torneck CD. Susceptibility of Nd:YAG laser-irradiated root surfaces in replanted teeth to external inflammatory resorption. Endod Dent Traumatol. 1998; 14:225–231. PMID: 9855802.
Article31. Panzarini SR, Okamoto R, Poi WR, Sonoda CK, Pedrini D, da Silva PE, Saito CT, Marão HF, Sedlacek P. Histological and immunohistochemical analyses of the chronology of healing process after immediate tooth replantation in incisor rat teeth. Dent Traumatol. 2013; 29:15–22. PMID: 22413942.
Article32. Pigatto Mitihiro D, de Paula Ramos S, Corazza Montero J, Alves Campos A, de Oliveira Toginho Filho D, Dezan Garbelini CC. Effects of near-infrared LED therapy on experimental tooth replantation in rats. Dent Traumatol. 2017; 33:32–37. PMID: 27472656.
Article33. Saito CT, Gulinelli JL, Panzarini SR, Garcia VG, Okamoto R, Okamoto T, Sonoda CK, Poi WR. Effect of low-level laser therapy on the healing process after tooth replantation: a histomorphometrical and immunohistochemical analysis. Dent Traumatol. 2011; 27:30–39. PMID: 21244626.
Article34. Carvalho ES, Costa FT, Campos MS, Anbinder AL, Neves AC, Habitante SM, Lage-Marques JL, Raldi DP. Root surface treatment using diode laser in delayed tooth replantation: radiographic and histomorphometric analyses in rats. Dent Traumatol. 2012; 28:429–436. PMID: 22236150.
Article35. Vilela RG, Gjerde K, Frigo L, Leal Junior EC, Lopes-Martins RA, Kleine BM, Prokopowitsch I. Histomorphometric analysis of inflammatory response and necrosis in re-implanted central incisor of rats treated with low-level laser therapy. Lasers Med Sci. 2012; 27:551–557. PMID: 21617972.
Article36. de Carvalho FB, Andrade AS, Barbosa AF, Aguiar MC, Cangussu MC, Pinheiro AL, Ramalho LM. Evaluation of laser phototherapy (λ 780 nm) after dental replantation in rats. Dent Traumatol. 2016; 32:488–494. PMID: 27242245.
Article37. Matos FS, Godolphim FJ, Correia AM, de Albuquerque Júnior RL, Paranhos LR, Rode SM, Ribeiro MA. Effect of laser photobiomodulation on the periodontal repair process of replanted teeth. Dent Traumatol. 2016; 32:402–408. PMID: 27126801.
Article38. Carvalho ED, Rosa RH, Pereira FM, Anbinder AL, Mello I, Habitante SM, Raldi DP. Effects of diode laser irradiation and fibroblast growth factor on periodontal healing of replanted teeth after extended extra-oral dry time. Dent Traumatol. 2017; 33:91–99. PMID: 27748036.
Article39. McGuinness LA, Higgins JP. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021; 12:55–61. PMID: 32336025.
Article40. Hecova H, Tzigkounakis V, Merglova V, Netolicky J. A retrospective study of 889 injured permanent teeth. Dent Traumatol. 2010; 26:466–475. PMID: 20946344.
Article41. Soares AJ, Gomes BP, Zaia AA, Ferraz CC, de Souza-Filho FJ. Relationship between clinical-radiographic evaluation and outcome of teeth replantation. Dent Traumatol. 2008; 24:183–188. PMID: 18352921.
Article42. Ash C, Dubec M, Donne K, Bashford T. Effect of wavelength and beam width on penetration in light-tissue interaction using computational methods. Lasers Med Sci. 2017; 32:1909–1918. PMID: 28900751.
Article43. Cios A, Cieplak M, Szymański Ł, Lewicka A, Cierniak S, Stankiewicz W, Mendrycka M, Lewicki S. Effect of different wavelengths of laser irradiation on the skin cells. Int J Mol Sci. 2021; 22:2437. PMID: 33670977.
Article44. Basso FG, Pansani TN, Cardoso LM, Citta M, Soares DG, Scheffel DS, Hebling J, de Souza Costa CA. Epithelial cell-enhanced metabolism by low-level laser therapy and epidermal growth factor. Lasers Med Sci. 2018; 33:445–449. PMID: 28285410.
Article45. Lopes-Martins RAB, Penna SC, Joensen J, Iversen VV, Bjordal JM. Low-level laser therapy [LLLT] in inflammatory and rheumatic diseases: a review of therapeutic mechanisms. Curr Rheumatol Rev. 2007; 3:147–154.
Article46. Lee JH, Chiang MH, Chen PH, Ho ML, Lee HE, Wang YH. Anti-inflammatory effects of low-level laser therapy on human periodontal ligament cells: in vitro study. Lasers Med Sci. 2018; 33:469–477. PMID: 29116611.
Article47. Fujimura T, Mitani A, Fukuda M, Mogi M, Osawa K, Takahashi S, Aino M, Iwamura Y, Miyajima S, Yamamoto H, Noguchi T. Irradiation with a low-level diode laser induces the developmental endothelial locus-1 gene and reduces proinflammatory cytokines in epithelial cells. Lasers Med Sci. 2014; 29:987–994. PMID: 24197516.
Article48. Kreisler M, Christoffers AB, Willershausen B, d’Hoedt B. Effect of low-level GaAlAs laser irradiation on the proliferation rate of human periodontal ligament fibroblasts: an in vitro study. J Clin Periodontol. 2003; 30:353–358. PMID: 12694435.
Article49. Kreisler M, Christoffers AB, Al-Haj H, Willershausen B, d’Hoedt B. Low level 809-nm diode laser-induced in vitro stimulation of the proliferation of human gingival fibroblasts. Lasers Surg Med. 2002; 30:365–369. PMID: 12116329.
Article50. Marinho RR, Matos RM, Santos JS, Ribeiro MA, Smaniotto S, Barreto EO, Ribeiro RA, Lima RC Jr, Albuquerque RL Jr, Thomazzi SM. Potentiated anti-inflammatory effect of combined 780 nm and 660 nm low level laser therapy on the experimental laryngitis. J Photochem Photobiol B. 2013; 121:86–93. PMID: 23524249.
Article51. Santos NR, de M Sobrinho JB, Almeida PF, Ribeiro AA, Cangussú MC, dos Santos JN, Pinheiro AL. Influence of the combination of infrared and red laser light on the healing of cutaneous wounds infected by Staphylococcus aureus. Photomed Laser Surg. 2011; 29:177–182. PMID: 21214389.
Article52. Raldi DP, Mello I, Neves AC, Habitante SM, Miyagi SS, Lage-Marques JL. Attachment of cultured fibroblasts and ultrastructural analysis of simulated cervical resorptions treated with high-power lasers and MTA. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e154–e161. PMID: 19969481.
Article53. Haypek P, Zezell DM, Bachmann L, Marques MM. Interaction between high-power diode laser and dental root surface. Thermal, morphological and biocompatibility analysis. J Oral Laser Applic. 2006; 6:101–109.54. Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999; 49:1–17. PMID: 10365442.
Article55. Aihara N, Yamaguchi M, Kasai K. Low-energy irradiation stimulates formation of osteoclast-like cells via RANK expression in vitro . Lasers Med Sci. 2006; 21:24–33. PMID: 16568210.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A roentgenographic study on apical root resorption of human permanent teeth
- Enamel matrix derivative for replanted teeth in animal models: a systematic review and meta-analysis
- A radiographic study on root resorption in the malocclusion patients before orthodontic treatment
- Root surface changes during the initial leveling and alignment phase in orthodontics: a scanning electron microscopic study
- A study on the pattern of the root resorption following maxillary incisor retraction