J Periodontal Implant Sci.
2011 Apr;41(2):60-66.
Labial and lingual/palatal bone thickness of maxillary and mandibular anteriors in human cadavers in Koreans
- Affiliations
-
- 1Division of Periodontology, Department of Dentistry, Hanyang University College of Medicine, Seoul, Korea. hjyperio@hanyang.ac.kr
Abstract
- PURPOSE
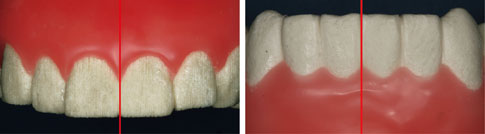
The aim of this study is to evaluate the buccal and lingual bone thickness in the anterior teeth and the relationship between bone thickness and the tissue biotype.
METHODS
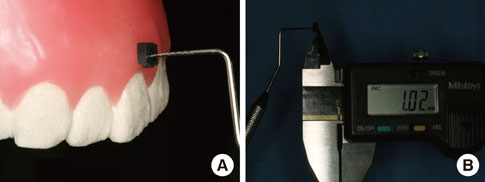
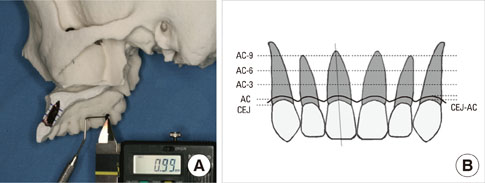
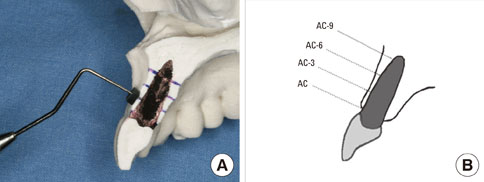
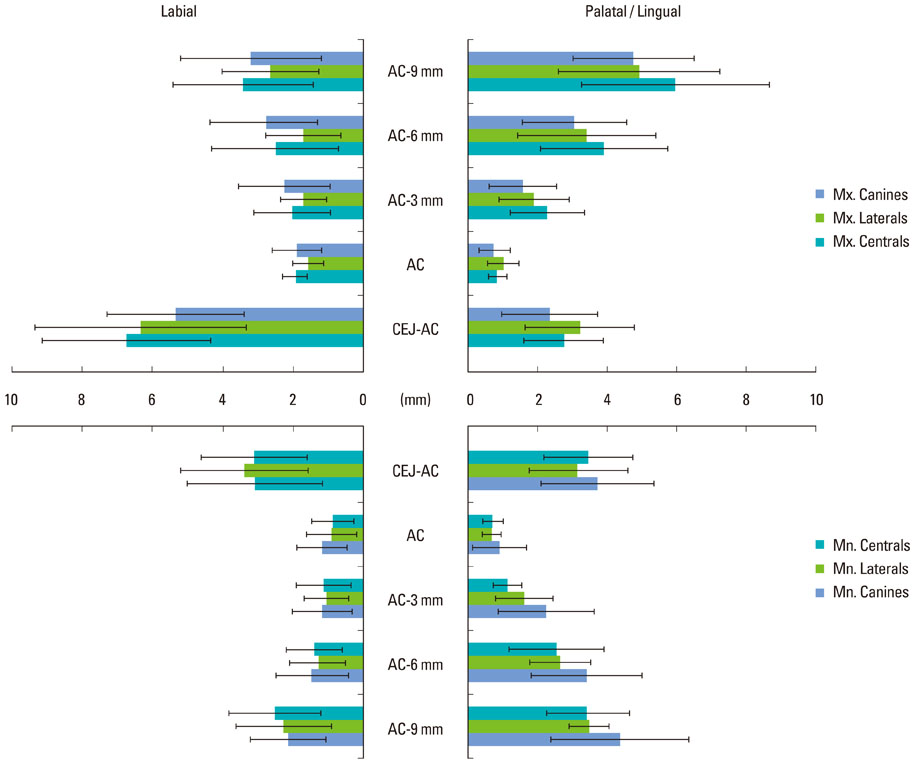
Three male and two female human cadaver heads (mean age, 55.4 years) were used in this study. First, the biotype of periodontium was evaluated and categorized into a thick or a thin group. Next, full thickness reflections of the mandible and the maxilla to expose the underlying bone for accurate measurements in the anterior regions were performed. After the removal of the half of the alveolar bone, the probe with a stopper was used to measure the thickness of bone plate at the alveolar crest (AC), 3 mm apical to the alveolar crest (AC-3), 6 mm apical to the alveolar crest (AC-6), and 9 mm apical to the alveolar crest (AC-9).
RESULTS
Four of them had a thick biotype. There was no penetration or dehiscence. The thickness of the buccal plates at the alveolar crest were 0.97+/-0.18 mm, 0.78+/-0.21 mm, and 0.95+/-0.35 mm in the maxillary central incisors, lateral incisors, and canines, respectively. The thickness of the labial plates at the alveolar crest were 0.86+/-0.59 mm, 0.88+/-0.70 mm, and 1.17+/-0.70 mm in the mandibular central incisors, lateral incisors and canines, respectively.
CONCLUSIONS
The thickness of the labial plate in the maxillary anteriors is very thin that great caution is needed for placing an implant. The present study showed the bone thickness of maxillary and mandibular anteriors at different positions. Therefore, these data can be useful for the understanding of the bone thickness of the anteriors and a successful implant placement.
Keyword
MeSH Terms
Figure
Reference
-
1. Blanes RJ, Bernard JP, Blanes ZM, Belser UC. A 10-year prospective study of ITI dental implants placed in the posterior region. II: influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clin Oral Implants Res. 2007. 18:707–714.
Article2. Tolstunov L. Implant zones of the jaws: implant location and related success rate. J Oral Implantol. 2007. 33:211–220.
Article3. Evans CD, Chen ST. Esthetic outcomes of immediate implant placements. Clin Oral Implants Res. 2008. 19:73–80.
Article4. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989. 9:332–343.5. Kan JY, Rungcharassaeng K, Umezu K, Kois JC. Dimensions of peri-implant mucosa: an evaluation of maxillary anterior single implants in humans. J Periodontol. 2003. 74:557–562.
Article6. Chen ST, Darby IB, Reynolds EC. A prospective clinical study of non-submerged immediate implants: clinical outcomes and esthetic results. Clin Oral Implants Res. 2007. 18:552–562.
Article7. Wheeler SL, Vogel RE, Casellini R. Tissue preservation and maintenance of optimum esthetics: a clinical report. Int J Oral Maxillofac Implants. 2000. 15:265–271.8. Becker BE, Becker W, Ricci A, Geurs N. A prospective clinical trial of endosseous screw-shaped implants placed at the time of tooth extraction without augmentation. J Periodontol. 1998. 69:920–926.
Article9. Paolantonio M, Dolci M, Scarano A, d'Archivio D, di Placido G, Tumini V, et al. Immediate implantation in fresh extraction sockets. A controlled clinical and histological study in man. J Periodontol. 2001. 72:1560–1571.
Article10. Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005. 32:212–218.
Article11. Araújo MG, Sukekava F, Wennström JL, Lindhe J. Ridge alterations following implant placement in fresh extraction sockets: an experimental study in the dog. J Clin Periodontol. 2005. 32:645–652.
Article12. Araújo MG, Wennström JL, Lindhe J. Modeling of the buccal and lingual bone walls of fresh extraction sites following implant installation. Clin Oral Implants Res. 2006. 17:606–614.
Article13. Botticelli D, Berglundh T, Lindhe J. The influence of a biomaterial on the closure of a marginal hard tissue defect adjacent to implants. An experimental study in the dog. Clin Oral Implants Res. 2004. 15:285–292.
Article14. Botticelli D, Persson LG, Lindhe J, Berglundh T. Bone tissue formation adjacent to implants placed in fresh extraction sockets: an experimental study in dogs. Clin Oral Implants Res. 2006. 17:351–358.
Article15. Becker W, Goldstein M, Becker BE, Sennerby L. Minimally invasive flapless implant surgery: a prospective multicenter study. Clin Implant Dent Relat Res. 2005. 7:Suppl 1. S21–S27.
Article16. Schwartz-Arad D, Chaushu G. Immediate implant placement: a procedure without incisions. J Periodontol. 1998. 69:743–750.
Article17. Chen ST, Darby IB, Reynolds EC, Clement JG. Immediate implant placement postextraction without flap elevation. J Periodontol. 2009. 80:163–172.
Article18. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004. 19:Suppl. 43–61.19. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005. 25:113–119.20. Ferrus J, Cecchinato D, Pjetursson EB, Lang NP, Sanz M, Lindhe J. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implants Res. 2010. 21:22–29.
Article21. Katranji A, Misch K, Wang HL. Cortical bone thickness in dentate and edentulous human cadavers. J Periodontol. 2007. 78:874–878.
Article22. Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith DH. Gingival biotype assessment in the esthetic zone: visual versus direct measurement. Int J Periodontics Restorative Dent. 2010. 30:237–243.23. Araújo MG, Sukekava F, Wennström JL, Lindhe J. Tissue modeling following implant placement in fresh extraction sockets. Clin Oral Implants Res. 2006. 17:615–624.
Article24. Pennel BM, King KO, Wilderman MN, Barron JM. Repair of the alveolar process following osseous surgery. J Periodontol. 1967. 38:426–431.
Article25. Wilderman MN, Pennel BM, King K, Barron JM. Histogenesis of repair following osseous surgery. J Periodontol. 1970. 41:551–565.
Article26. Kan JY, Rungcharassaeng K, Lozada JL. Bilaminar subepithelial connective tissue grafts for immediate implant placement and provisionalization in the esthetic zone. J Calif Dent Assoc. 2005. 33:865–871.27. Fickl S, Zuhr O, Wachtel H, Bolz W, Huerzeler M. Tissue alterations after tooth extraction with and without surgical trauma: a volumetric study in the beagle dog. J Clin Periodontol. 2008. 35:356–363.
Article28. Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res. 2009. 20:545–549.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Alveolar bone thickness around maxillary central incisors of different inclination assessed with cone-beam computed tomography
- Angulation between Long Axis of Anterior Teeth and Alveolar Process, and Thickness of Alveolar Bone
- Alveolar bone thickness and fenestration of incisors in untreated Korean patients with skeletal class III malocclusion: A retrospective 3-dimensional cone-beam computed tomography study
- Quality and Morphology on cortico-cancellous bone in Korean mandibular symphysis area
- Evaluation of mandibular cortical bone thickness for placement of temporary anchorage devices (TADs)