J Periodontal Implant Sci.
2010 Aug;40(4):194-200.
A simple approach to preserve keratinized mucosa around implants using a pre-fabricated implant-retained stent: a report of two cases
- Affiliations
-
- 1Department of Periodontology, Research Institute for Periodontal Regeneration, Yonsei University College of Dentistry, Seoul, Korea. shchoi726@yuhs.ac
- 2Goodmorning Dental Clinic, Seoul, Korea.
Abstract
- PURPOSE
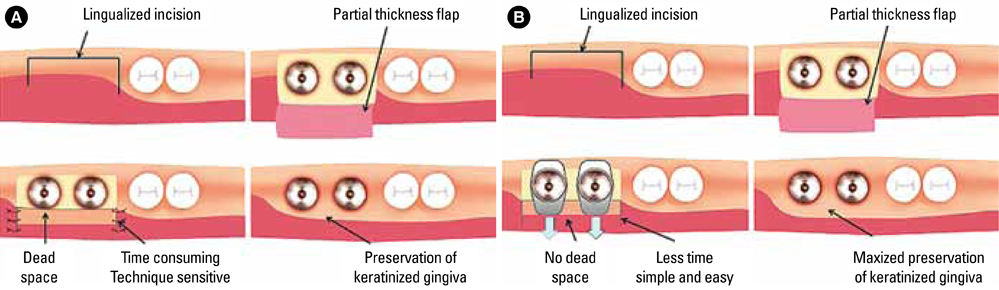
There is no consensus regarding the relationship between the width of keratinized mucosa and the health of peri-implant tissues, but clinicians prefer to provide enough keratinized mucosa around dental implants for long-term implant maintenance. An apically positioned flap during second stage implant surgery is the chosen method of widening the keratinized zone in simple procedures. However, the routine suture techniques used with this method tend to apply tension over the provisional abutments and decrease pre-existing keratinized mucosa. To overcome this shortcoming, a pre-fabricated implant-retained stent was designed to apply vertical pressure on the labial flap and stabilize it in a bucco-apical direction to create a wide keratinized mucous zone.
METHODS
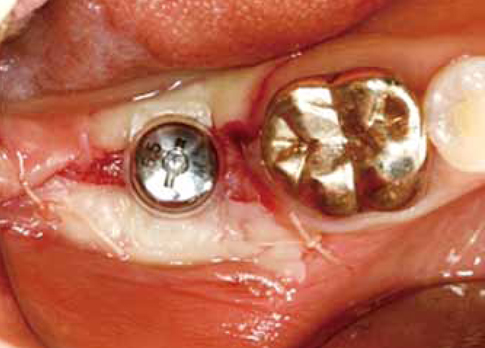
During second stage implant surgery, an apically displaced, partial thickness flap with a lingualized incision was retracted. A pre-fabricated stent was clipped over the abutments after connecting to the provisional abutment. Vertical pressure was applied to displace the labial flap. No suture was required and the stent was removed after 10 days.
RESULTS
A clinically relevant amount of keratinized mucosa was achieved around the dental implants. Buccally displaced keratinized mucosa was firmly attached to the underlying periosteum. A slight shrinkage of the keratinized zone was noted after the healing period in one patient, but no discomfort during oral hygiene was reported. Clinically healthy gingiva with enough keratinized mucosa was achieved in both patients.
CONCLUSIONS
The proposed technique is a simple and time-effective technique for preserving and providing keratinized tissue around dental implants
Keyword
MeSH Terms
Figure
Reference
-
1. Adell R, Lekholm U, Rockler B, Branemark PI, Lindhe J, Eriksson B, et al. Marginal tissue reactions at osseointegrated titanium fixtures (I). A 3-year longitudinal prospective study. Int J Oral Maxillofac Surg. 1986. 15:39–52.2. Lekholm U, Adell R, Lindhe J, Branemark PI, Eriksson B, Rockler B, et al. Marginal tissue reactions at osseointegrated titanium fixtures. (II) A cross-sectional retrospective study. Int J Oral Maxillofac Surg. 1986. 15:53–61.3. Schou S, Holmstrup P, Hjorting-Hansen E, Lang NP. Plaque-induced marginal tissue reactions of osseointegrated oral implants: a review of the literature. Clin Oral Implants Res. 1992. 3:149–161.
Article4. Warrer K, Buser D, Lang NP, Karring T. Plaque-induced peri-implantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implants Res. 1995. 6:131–138.
Article5. Zarb GA, Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part III: Problems and complications encountered. J Prosthet Dent. 1990. 64:185–194.
Article6. Adell R, Lekholm U, Rockler B, Branemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981. 10:387–416.
Article7. Block MS, Kent JN. Factors associated with soft- and hard-tissue compromise of endosseous implants. J Oral Maxillofac Surg. 1990. 48:1153–1160.
Article8. Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants. 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990. 1:33–40.
Article9. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986. 1:11–25.10. Langer B, Sullivan DY. Osseointegration: its impact on the interrelationship of periodontics and restorative dentistry: Part I. Int J Periodontics Restorative Dent. 1989. 9:84–105.11. Langer B, Langer L. Overlapped flap: a surgical modification for implant fixture installation. Int J Periodontics Restorative Dent. 1990. 10:208–215.12. Landi L, Sabatucci D. Plastic surgery at the time of membrane removal around mandibular endosseous implants: a modified technique for implant uncovering. Int J Periodontics Restorative Dent. 2001. 21:280–287.13. Reiser G, Brun J, Mahan P, Larkin L. The subepithelial connective tissue graft palatal donor site:Anatomic considerations for surgeons. Int J Periodontics Restorative Dent. 1996. 16:130–137.14. Lang NP, Loe H. The relationship between the width of keratinized gingiva and gingival health. J Periodontol. 1972. 43:623–627.
Article15. de Trey E, Bernimoulin JP. Influence of free gingival grafts on the health of the marginal gingiva. J Clin Periodontol. 1980. 7:381–393.
Article16. Hall WB. Present status of soft tissue grafting. J Periodontol. 1977. 48:587–597.
Article17. Wennstrom JL, Bengazi F, Lekholm U. The influence of the masticatory mucosa on the peri-implant soft tissue condition. Clin Oral Implants Res. 1994. 5:1–8.
Article18. Bengazi F, Wennstrom JL, Lekholm U. Recession of the soft tissue margin at oral implants. A 2-year longitudinal prospective study. Clin Oral Implants Res. 1996. 7:303–310.
Article19. Sclar AG. Soft tissue and esthetic considerations in implant dentistry. 2003. Chicago: Quintessence Publishing Co..20. Moore JR. A modification of stent design for preprosthetic surgery. J Oral Surg. 1970. 28:263–266.21. Sanders B, Starshak TJ. Modified technique for palatal mucosal grafts in mandibular labial vestibuloplasty. J Oral Surg. 1975. 33:950–952.22. Firtell DN, Oatis GW, Curtis TA, Sugg WE Jr. A stent for a split-thickness skin graft vestibuloplasty. J Prosthet Dent. 1976. 36:204–210.
Article23. Hughes WG, Howard CW 3rd. Simultaneous split-thickness skin grafting and placement of endosteal implants in the edentulous mandible: a preliminary report. J Oral Maxillofac Surg. 1992. 50:448–451.
Article24. Nystrom E, Kahnberg KE, Albrektsson T. Treatment of the severely resorbed maxillae with bone graft and titanium implants: histologic review of autopsy specimens. Int J Oral Maxillofac Implants. 1993. 8:167–172.25. Brygider RM, Bain CA. Custom stent fabrication for free gingival grafts around osseointegrated abutment fixtures. J Prosthet Dent. 1989. 62:320–322.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preservation of keratinized mucosa around implants using a prefabricated implant-retained stent: a case-control study
- Free Gingival Graft to Gain Peri-implant Keratinized Mucosa
- Free gingival graft for the increase of peri-implant attached keratinized mucosa decreased after guided bone regeneration
- Retrospective analysis of keratinized tissue augmentation using a xenogeneic collagen matrix for resolving peri-implant mucositis and peri-implantitis
- The study of the peri-inplant soft tissue around osseointegrated implants in partial edentulous patients