J Periodontal Implant Sci.
2016 Oct;46(5):329-336. 10.5051/jpis.2016.46.5.329.
Preservation of keratinized mucosa around implants using a prefabricated implant-retained stent: a case-control study
- Affiliations
-
- 1Department of Periodontology, Dankook University College of Dentistry, Cheonan, Korea. perioshin@dankook.ac.kr
- 2Department of Maxilo-Stomatology, Vietnam National University School of Medicine and Pharmacy, Hanoi, Vietnam.
- KMID: 2354931
- DOI: http://doi.org/10.5051/jpis.2016.46.5.329
Abstract
- PURPOSE
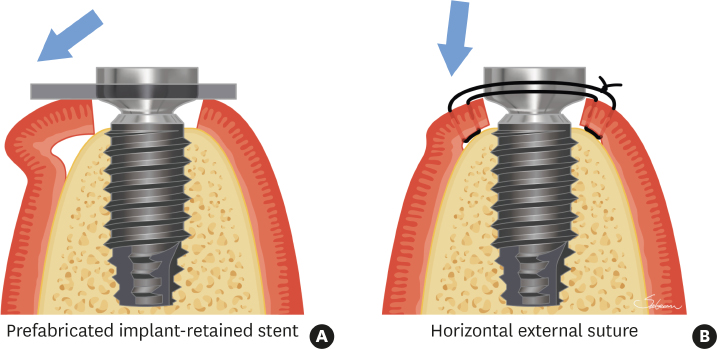
The aim of this study was to clinically assess the impact of a prefabricated implant-retained stent clipped over healing abutments on the preservation of keratinized mucosa around implants after implant surgery, and to compare it with horizontal external mattress sutures.
METHODS
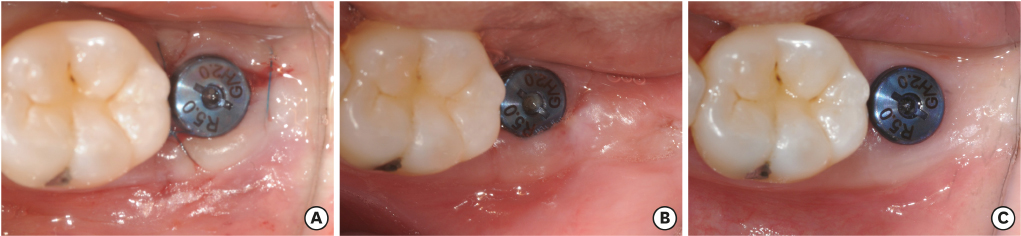
A total of 50 patients were enrolled in this study. In the test group, a prefabricated implant-retained stent was clipped on the healing abutment after implant surgery to replace the keratinized tissue bucco-apically. In the control group, horizontal external mattress sutures were applied instead of using a stent. After the surgical procedure, the width of the buccal keratinized mucosa was measured at the mesial, middle, and distal aspects of the healing abutment. The change in the width of the buccal keratinized mucosa was assessed at 1 and 3 months.
RESULTS
Healing was uneventful in both groups. The difference of width between baseline and 1 month was −0.26±0.85 mm in the test group, without any statistical significance (P=0.137). Meanwhile, the corresponding difference in the control group was −0.74±0.73 mm and it showed statistical significance (P<0.001). The difference of width between baseline and 3 months was −0.57±0.97 mm in the test group and −0.86±0.71 mm in the control group. These reductions were statistically significant (P<0.05); however, there was no difference between the 2 groups.
CONCLUSIONS
Using a prefabricated implant-retained stent was shown to be effective in the preservation of the keratinized mucosa around implants and it was simple and straightforward in comparison to the horizontal external mattress suture technique.
Keyword
MeSH Terms
Figure
Reference
-
1. Wennström JL, Bengazi F, Lekholm U. The influence of the masticatory mucosa on the peri-implant soft tissue condition. Clin Oral Implants Res. 1994; 5:1–8.
Article2. Warrer K, Buser D, Lang NP, Karring T. Plaque-induced peri-implantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implants Res. 1995; 6:131–138.
Article3. Lin GH, Chan HL, Wang HL. The significance of keratinized mucosa on implant health: a systematic review. J Periodontol. 2013; 84:1755–1767.
Article4. Roccuzzo M, Grasso G, Dalmasso P. Keratinized mucosa around implants in partially edentulous posterior mandible: 10-year results of a prospective comparative study. Clin Oral Implants Res. 2016; 27:491–496.
Article5. Fugazzotto PA. Maintenance of soft tissue closure following guided bone regeneration: technical considerations and report of 723 cases. J Periodontol. 1999; 70:1085–1097.
Article6. Trombelli L, Tatakis DN, Scabbia A, Zimmerman GJ. Comparison of mucogingival changes following treatment with coronally positioned flap and guided tissue regeneration procedures. Int J Periodontics Restorative Dent. 1997; 17:448–455.7. Seibert JS. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts. Part I. Technique and wound healing. Compend Contin Educ Dent. 1983; 4:437–453.8. Carnio J, Miller PD Jr. Increasing the amount of attached gingiva using a modified apically repositioned flap. J Periodontol. 1999; 70:1110–1117.
Article9. Carnio J, Camargo PM. The modified apically repositioned flap to increase the dimensions of attached gingiva: the single incision technique for multiple adjacent teeth. Int J Periodontics Restorative Dent. 2006; 26:265–269.10. Karring T, Ostergaard E, Löe H. Conservation of tissue specificity after heterotopic transplantation of gingiva and alveolar mucosa. J Periodontal Res. 1971; 6:282–293.
Article11. Karring T, Lang NP, Löe H. The role of gingival connective tissue in determining epithelial differentiation. J Periodontal Res. 1975; 10:1–11.
Article12. Del Pizzo M, Modica F, Bethaz N, Priotto P, Romagnoli R. The connective tissue graft: a comparative clinical evaluation of wound healing at the palatal donor site. A preliminary study. J Clin Periodontol. 2002; 29:848–854.
Article13. Soileau KM, Brannon RB. A histologic evaluation of various stages of palatal healing following subepithelial connective tissue grafting procedures: a comparison of eight cases. J Periodontol. 2006; 77:1267–1273.
Article14. Park JC, Yang KB, Choi Y, Kim YT, Jung UW, Kim CS, et al. A simple approach to preserve keratinized mucosa around implants using a pre-fabricated implant-retained stent: a report of two cases. J Periodontal Implant Sci. 2010; 40:194–200.
Article15. Moore JR. A modification of stent design for preprosthetic surgery. J Oral Surg. 1970; 28:263–266.16. Sanders B, Starshak TJ. Modified technique for palatal mucosal grafts in mandibular labial vestibuloplasty. J Oral Surg. 1975; 33:950–952.17. Firtell DN, Oatis GW, Curtis TA, Sugg WE Jr. A stent for a split-thickness skin graft vestibuloplasty. J Prosthet Dent. 1976; 36:204–210.
Article18. Hughes WG, Howard CW 3rd. Simultaneous split-thickness skin grafting and placement of endosteal implants in the edentulous mandible: a preliminary report. J Oral Maxillofac Surg. 1992; 50:448–451.
Article19. Kahnberg KE, Nystrom E, Bartholdsson L. Combined use of bone grafts and Brånemark fixtures in the treatment of severely resorbed maxillae. Int J Oral Maxillofac Implants. 1989; 4:297–304.20. Nyström E, Kahnberg KE, Albrektsson T. Treatment of the severely resorbed maxillae with bone graft and titanium implants: histologic review of autopsy specimens. Int J Oral Maxillofac Implants. 1993; 8:167–172.21. Small SA. Surgical stents and major oral maxillofacial surgery. Dent Clin North Am. 1989; 33:497–509.22. ten Bruggenkate CM, Krekeler G, van der Kwast WA, Oosterbeek HS. Palatal mucosa grafts for oral implant devices. Oral Surg Oral Med Oral Pathol. 1991; 72:154–158.
Article23. Grgurević J, Knezević G, Kobler P, Krmpotić I. An alternative method of fixation of alveolar ridge mucosa during the vestibuloplasty procedure. Br J Oral Maxillofac Surg. 1988; 26:370–374.
Article24. Hall HD. Vestibuloplasty, mucosal grafts (palatal and buccal). J Oral Surg. 1971; 29:786–791.25. Brygider RM, Bain CA. Custom stent fabrication for free gingival grafts around osseointegrated abutment fixtures. J Prosthet Dent. 1989; 62:320–322.
Article26. Ziccardi VB, Misch C, Patterson GT, Nawrocki JS. Use of endosseous implants to fixate a surgical stent in conjunction with mandibular vestibuloplasty. Compendium. 1993; 14:774.27. Proussaefs P, Lozada J, Kleinman A. The “Loma Linda stent”: a screw-retained resin stent. J Oral Implantol. 2003; 29:19–23.28. Langer B, Langer L. Overlapped flap: a surgical modification for implant fixture installation. Int J Periodontics Restorative Dent. 1990; 10:208–215.29. Landi L, Sabatucci D. Plastic surgery at the time of membrane removal around mandibular endosseous implants: a modified technique for implant uncovering. Int J Periodontics Restorative Dent. 2001; 21:280–287.30. Lee KH, Kim BO, Jang HS. Clinical evaluation of a collagen matrix to enhance the width of keratinized gingiva around dental implants. J Periodontal Implant Sci. 2010; 40:96–101.
Article31. Valderhaug J, Birkeland JM. Periodontal conditions in patients 5 years following insertion of fixed prostheses. Pocket depth and loss of attachment. J Oral Rehabil. 1976; 3:237–243.
Article32. Stetler KJ, Bissada NF. Significance of the width of keratinized gingiva on the periodontal status of teeth with submarginal restorations. J Periodontol. 1987; 58:696–700.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A simple approach to preserve keratinized mucosa around implants using a pre-fabricated implant-retained stent: a report of two cases
- Free Gingival Graft to Gain Peri-implant Keratinized Mucosa
- Free gingival graft for the increase of peri-implant attached keratinized mucosa decreased after guided bone regeneration
- Retrospective analysis of keratinized tissue augmentation using a xenogeneic collagen matrix for resolving peri-implant mucositis and peri-implantitis
- The study of the peri-inplant soft tissue around osseointegrated implants in partial edentulous patients