J Korean Surg Soc.
2012 May;82(5):296-301.
Is there a relationship between beginning time and efficiency of octreotide in the treatment of experimental acute pancreatitis?
- Affiliations
-
- 1Department of Surgery, Selcuklu Medical Faculty, Selcuk University, Konya, Turkey. halptekin@hotmail.com
- 2Department of Emergency Medicine, Meram Medical Faculty, Selcuk University, Konya, Turkey.
- 3Department of Pathology, Meram Medical Faculty, Selcuk University, Konya, Turkey.
- 4Department of Biochemistry, Meram Medical Faculty, Selcuk University, Konya, Turkey.
Abstract
- PURPOSE
The efficacy of octreotide in the treatment of acute pancreatitis is controversial. Octreotide treatment for acute pancreatitis often shows poor correlation between results obtained in experimental studies and results of clinical trials. In a clinical setting, there is always a delay between the onset of the disease and initiation of the octreotide treatment. The aim of this study is to investigate the relationship between the beginning of treatment and alteration in effectiveness of octreotide.
METHODS
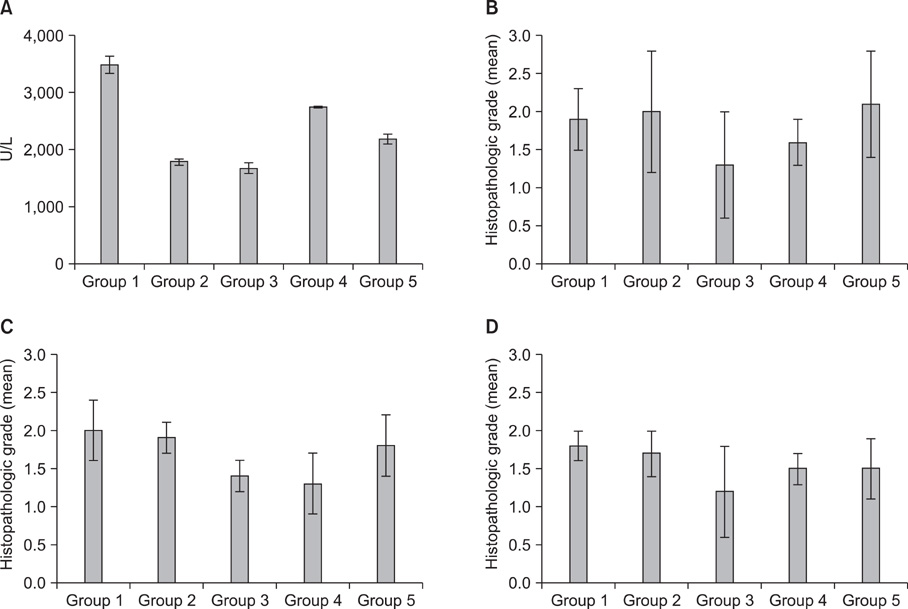
Acute pancreatitis was induced by pancreatic duct ligation in 50 rats. The rats were randomly divided into five groups. Octreotide was not used in group 1 (control group). Only single dose (4 microg/kg) octreotide was administered subcutaneously to rats in group 2, having induced pancreatitis. Octreotide treatment was begun at different times (8th, 24th, 48th hour) in three other groups and continued treatment at a dosage of 4 microg/kg t.i.d. The animals were sacrificed at the end of the 72nd hour and blood and tissue samples were collected.
RESULTS
Leukocyte count and plasma amylase values were less in groups 2 and 3. Hemorrhagic focuses were encountered less at pancreas tissues in group 3. Pancreatic necrosis and alveolar capillary basal membrane damage were lower in groups 3 and 4. No difference was found in fasting blood glucose, calcium and hematocrit.
CONCLUSION
Octreotide had benefical effects in acute pancreatitis when octreotide treatment was begun in the first 24 hours.
Keyword
MeSH Terms
Figure
Reference
-
1. Yeo CI, Cameron JL. Sabiston DC, Lyerly HK, editors. The pancreas. Textbook of surgery: the biological basis of modern surgical practice. 1997. 15th ed. Philadelphia: WB Saunders;1152–1186.2. Steer ML. Yamada T, Alpers DH, editors. Acute pancreatitis. Textbook of gastroenterology. 1991. Philadelphia: Lippincott;1859–1873.3. Calleja GA, Barkin JS. Acute pancreatitis. Med Clin North Am. 1993. 77:1037–1056.4. Doherty MG, Way LW. Way LW, Doherty MG, editors. Pancreas. Current surgical diagnosis and treatment. 2003. New York: McGraw-Hill;625–651.5. Choi JY, Kim KH. Effects of small molecular antioxidants on cerulein-induced acute pancreatitis in rat. Korean J Physiol Pharmacol. 1998. 2:629–635.6. Becker V. Pathological anatomy and pathogenesis of acute pancreatitis. World J Surg. 1981. 5:303–313.7. Choi TK, Mok F, Zhan WH, Fan ST, Lai EC, Wong J. Somatostatin in the treatment of acute pancreatitis: a prospective randomised controlled trial. Gut. 1989. 30:223–227.8. Guler O, Akturan S, Kisli E, Dolapçi I, Caydere M, Akova A. Acute pancreatitis, bacterial translocation, and different octreotide regimens: an experimental study. Surg Today. 2009. 39:876–883.9. Korun N, Yilmazlar T, Kaya E, Kutlay B. The effect of octreotide (SMS 201-995) on experimentally induced pancreatitis with 50% ethyl alcohol in rats. Int Surg. 1994. 79:148–151.10. Buchler MW, Binder M, Friess H. Role of somatostatin and its analogues in the treatment of acute and chronic pancreatitis. Gut. 1994. 35:3 Suppl. S15–S19.11. Jenkins SA, Berein A. Review article: the relative effectiveness of somatostatin and octreotide therapy in pancreatic disease. Aliment Pharmacol Ther. 1995. 9:349–361.12. Greenberg R, Haddad R, Kashtan H, Brazowski E, Graff E, Skornick Y, et al. Continuous intravenous octreotide treatment for acute experimental pancreatitis. Digestion. 1999. 60:125–131.13. Uhl W, Buchler MW, Malfertheiner P, Beger HG, Adler G, Gaus W. A randomised, double blind, multicentre trial of octreotide in moderate to severe acute pancreatitis. Gut. 1999. 45:97–104.14. Uhl W, Anghelacopoulos SE, Friess H, Buchler MW. The role of octreotide and somatostatin in acute and chronic pancreatitis. Digestion. 1999. 60:Suppl 2. 23–31.15. Kitagawa M, Naruse S, Ishiguro H, Hayakawa T. Pharmaceutical development for treating pancreatic diseases. Pancreas. 1998. 16:427–431.16. Buter A, Imrie CW, Carter CR, Evans S, McKay CJ. Dynamic nature of early organ dysfunction determines outcome in acute pancreatitis. Br J Surg. 2002. 89:298–302.17. Isenmann R, Rau B, Beger HG. Early severe acute pancreatitis: characteristics of a new subgroup. Pancreas. 2001. 22:274–278.18. Paran H, Klausner J, Siegal A, Graff E, Freund U, Kaplan O. Effect of the somatostatin analogue octreotide on experimental pancreatitis in rats. J Surg Res. 1996. 62:201–206.19. Kaplan O, Kaplan D, Casif E, Siegal A, Paran H, Graf E, et al. Effects of delayed administration of octreotide in acute experimental pancreatitis. J Surg Res. 1996. 62:109–117.20. Chen CC, Wang SS, Tsay SH, Lee FY, Wu SL, Lu RH, et al. Effects of high dose octreotide on retrograde bile salt-induced pancreatitis in rats. Peptides. 1998. 19:543–547.21. Murayama KM, Drew JB, Joehl RJ. Does somatostatin analogue prevent experimental acute pancreatitis? Arch Surg. 1990. 125:1570–1572.22. Baxter JN, Jenkins SA, Day DW, Roberts NB, Cowell DC, Mackie CR, et al. Effects of somatostatin and a long-acting somatostatin analogue on the prevention and treatment of experimentally induced acute pancreatitis in the rat. Br J Surg. 1985. 72:382–385.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Trial of Ocrteotide in the Theatment of Severe Acute Pancreatitis
- Acute Necrotizing Pancreatitis during L-asparaginase Treatment in a Patient with Acute Lymphoblastic Leukemia
- Evalutation of Corticosteroid and Octreotide in the Prevention of Post-ERCP Pancreatitis
- Experimental Animal Models of Pancreatic Diseases
- A Case of Mediastinal Pacreatic Pseudocyst Treated with Octreotide