Tuberc Respir Dis.
2015 Oct;78(4):450-454. 10.4046/trd.2015.78.4.450.
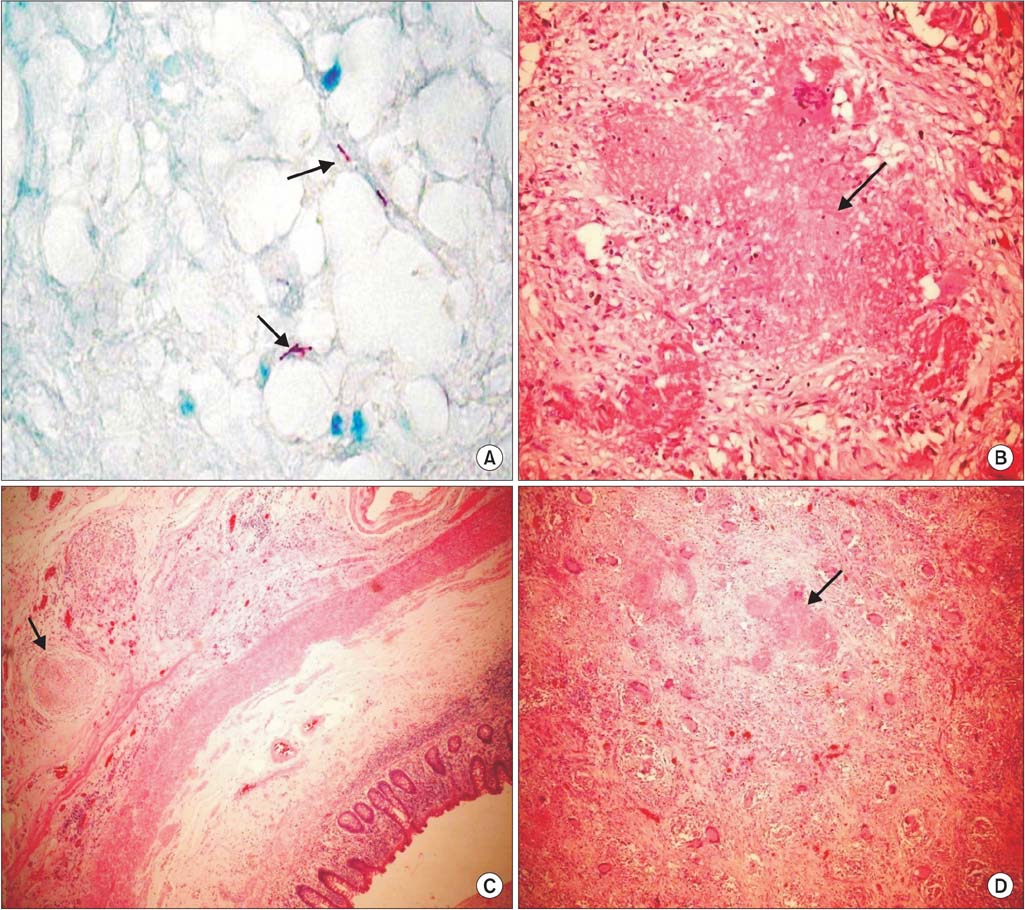
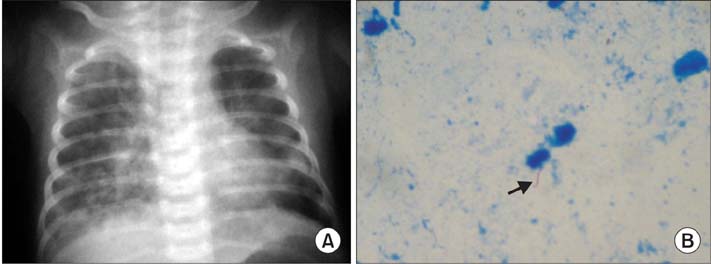
Congenital Tuberculosis as a Result of Disseminated Maternal Disease: Case Report
- Affiliations
-
- 1Clinica Universitaria Bolivariana, Servicio de Pediatria, Universidad Pontificia Bolivariana, Medellin, Colombia. alvaromicro@hotmail.com
- 2Universidad CES, Medellin, Colombia.
- 3Hospital Pablo Tobon Uribe, Medellin, Colombia.
- 4Facultad de Medicina, Universidad Pontificia Bolivariana, Medellin, Colombia.
- KMID: 2320726
- DOI: http://doi.org/10.4046/trd.2015.78.4.450
Abstract
- Although tuberculosis is highly prevalent worldwide, congenital tuberculosis is one of the least common manifestations of the disease. The diagnosis is usually difficult because of the non-specific clinical presentation and the lack of awareness of maternal disease prior to pregnancy and delivery. We present the case of a preterm neonate with congenital tuberculosis, born to a previously healthy mother who had developed severe disseminated tuberculosis during her pregnancy. Once the diagnosis was confirmed in the mother, the congenital infection was confirmed by isolation of Mycobacterium tuberculosis in gastric aspirates, and positive polymerase chain reaction in a cerebrospinal fluid examination. Treatment for tuberculosis with a four-drug regimen resulted in an adequate clinical response in both the mother and infant.
Keyword
MeSH Terms
Figure
Reference
-
1. Perez-Velez CM, Marais BJ. Tuberculosis in children. N Engl J Med. 2012; 367:348–361.2. Cortes Buelvas A, Osorio MA, Bolivar G, Lopez P, Palomino MF. Tuberculosis congénita. Informe de un caso con autopsia. Colomb Med. 2000; 31:185–188.3. Ormerod P. Tuberculosis in pregnancy and the puerperium. Thorax. 2001; 56:494–499.4. Dalamon RS, Cantelli SN, Jaroslavsky D, Bruno M, Debuh MA, Falk DJ. Tuberculosis congenita. Presentacion infrecuente de una enfermedad habitual. Arch Argent Pediatr. 2008; 106:147–150.5. Nakbanpot S, Rattanawong P. Congenital tuberculosis because of misdiagnosed maternal pulmonary tuberculosis during pregnancy. Jpn J Infect Dis. 2013; 66:327–330.6. Coulter JB. Perinatal tuberculosis. Ann Trop Paediatr. 2011; 31:11–13.7. Sosa LM, Cala LL, Mantilla JC. Congenital tuberculosis associated with maternal disseminated miliary tuberculosis. Biomedica. 2007; 27:475–482.8. Mantilla Hernandez JC, Cardenas NC. Tuberculosis congenita: reporte del primer caso en el nororiente colombiano. Medicas UIS. 2007; 20:137–142.9. David M, Ojeda P. Tuberculosis congenita. Presentacion de caso clínico. Rev Colomb Neumol. 2004; 16:189–192.10. Ray M, Dixit A, Vaipei K, Singhi PD. Congenital tuberculosis. Indian Pediatr. 2002; 39:1167–1168.11. Satti KF, Ali SA, Weitkamp JH. Congenital infections. Part 2: Parvovirus, Listeria, tuberculosis, syphilis, and varicella. Neoreviews. 2010; 11:e681–e695.12. Hageman J, Shulman S, Schreiber M, Luck S, Yogev R. Congenital tuberculosis: critical reappraisal of clinical findings and diagnostic procedures. Pediatrics. 1980; 66:980–984.13. Abughali N, van Der Kuyp F, Annable W, Kumar ML. Congenital tuberculosis. Pediatr Infect Dis J. 1994; 13:738–741.14. Cantwell MF, Shehab ZM, Costello AM, Sands L, Green WF, Ewing EP Jr, et al. Brief report: congenital tuberculosis. N Engl J Med. 1994; 330:1051–1054.15. Skevaki CL, Kafetzis DA. Tuberculosis in neonates and infants: epidemiology, pathogenesis, clinical manifestations, diagnosis, and management issues. Paediatr Drugs. 2005; 7:219–234.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Disseminated Bone Tuberculosis
- A Case of Disseminated Bone Tuberculosis with Diagnosed by Bone Marrow Aspirated Filter Biopsy
- Disseminated Tuberculosis in a Patient with Chronic Renal Failure
- A Case of Congenital Tuberculosis woth Massive Ascites and Pleural Effusion
- A Case of Disseminated Cutaneous Cryptococcosis Accompanied by Pulmonary Tuberculosis