Tuberc Respir Dis.
2015 Oct;78(4):396-400. 10.4046/trd.2015.78.4.396.
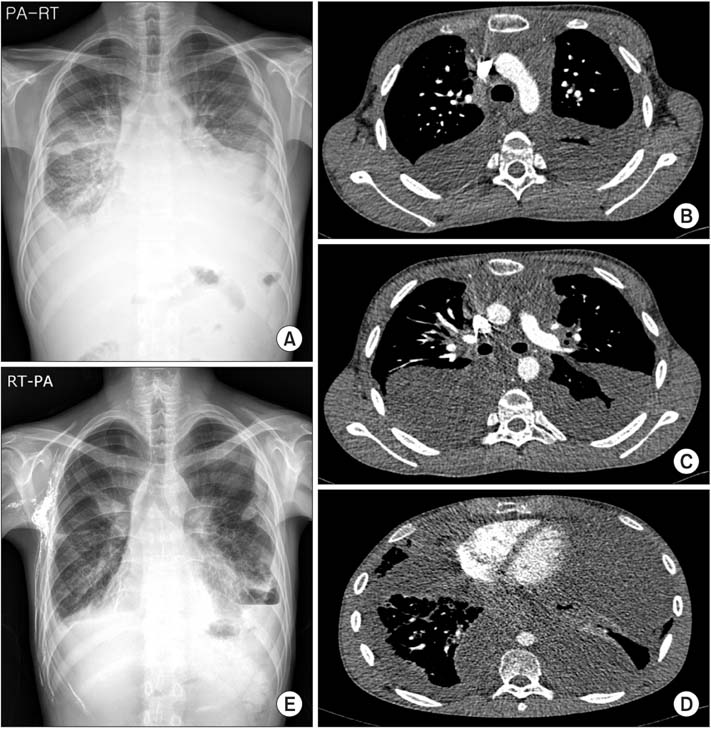
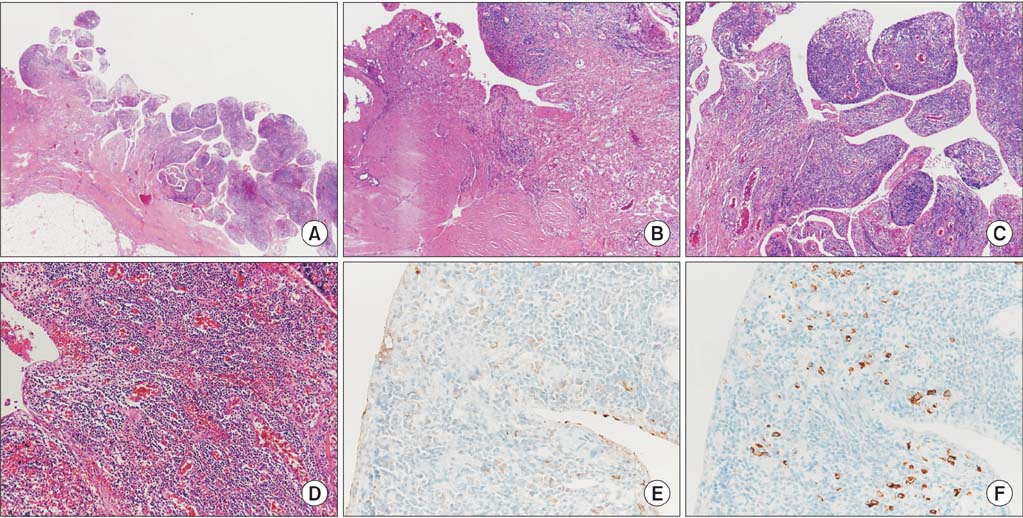
A Case of Extensive IgG4-Related Disease Presenting as Massive Pleural Effusion, Mediastinal Mass, and Mesenteric Lymphadenopathy in a 16-Year-Old Male
- Affiliations
-
- 1Division of Pulmonology, Yonsei University College of Medicine, Seoul, Korea. chungks@yuhs.ac
- 2Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2320714
- DOI: http://doi.org/10.4046/trd.2015.78.4.396
Abstract
- IgG4-related disease is an immune-mediated fibro-inflammatory disease, characterized by lymphoplasmacytic infiltration composed of IgG4-positive plasma cells of various organs with elevated circulating levels of IgG4. This disease is now reported with increasing frequency and usually affects middle-aged men. Massive pleural effusion in children is an uncommon feature in IgG4-related disease. Here, we report a case of a 16-year-old male patient with extensive IgG4-related disease presenting with massive pleural effusion, mediastinal mass, and mesenteric lymphadenopathy.
Keyword
MeSH Terms
Figure
Reference
-
1. Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012; 25:1181–1192.2. Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, et al. A novel clinical entity, IgG4-related disease (Ig-G4RD): general concept and details. Mod Rheumatol. 2012; 22:1–14.3. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012; 366:539–551.4. Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001; 344:732–738.5. Kamisawa T, Okamoto A. IgG4-related sclerosing disease. World J Gastroenterol. 2008; 14:3948–3955.6. Cheuk W, Chan JK. IgG4-related sclerosing disease: a critical appraisal of an evolving clinicopathologic entity. Adv Anat Pathol. 2010; 17:303–332.7. Carruthers MN, Khosroshahi A, Augustin T, Deshpande V, Stone JH. The diagnostic utility of serum IgG4 concentrations in IgG4-related disease. Ann Rheum Dis. 2015; 74:14–18.8. Khosroshahi A, Carruthers MN, Deshpande V, Unizony S, Bloch DB, Stone JH. Rituximab for the treatment of IgG4-related disease: lessons from 10 consecutive patients. Medicine (Baltimore). 2012; 91:57–66.9. Frulloni L, Lunardi C, Simone R, Dolcino M, Scattolini C, Falconi M, et al. Identification of a novel antibody associated with autoimmune pancreatitis. N Engl J Med. 2009; 361:2135–2142.10. Raina A, Yadav D, Krasinskas AM, McGrath KM, Khalid A, Sanders M, et al. Evaluation and management of autoimmune pancreatitis: experience at a large US center. Am J Gastroenterol. 2009; 104:2295–2306.11. Choi JH, Sim JK, Oh JY, Lee EJ, Hur GY, Lee SH, et al. A case of IgG4-related disease presenting as massive pleural effusion and thrombophlebitis. Tuberc Respir Dis. 2014; 76:179–183.12. Mahajan VS, Mattoo H, Deshpande V, Pillai SS, Stone JH. IgG4-related disease. Annu Rev Pathol. 2014; 9:315–347.13. Kato E, Takayanagi N, Ishiguro T, Kagiyama N, Shimizu Y, Sugita Y. IgG4-related pleuritis with chylothorax. Intern Med. 2014; 53:1545–1548.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of IgG4-Related Disease Presenting as Massive Pleural Effusion and Thrombophlebitis
- Medistinal Teratoma with Pleural and Pericardial Effusion Teratoma with Pleural and Pericardial Effusion
- Immunoglobulin G4-Related Disease in the Thorax: Imaging Findings and Differential Diagnosis
- Rupture of Mediastinal Mature Teratoma into the Pleural Cavity: A Case Report
- A Case of Chronic Pancreatitis with Massive Pleural Effusion