Tuberc Respir Dis.
2015 Oct;78(4):326-335. 10.4046/trd.2015.78.4.326.
The Influence of Asian Dust, Haze, Mist, and Fog on Hospital Visits for Airway Diseases
- Affiliations
-
- 1Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Internal Medicine and Environmental Health Center, Kangwon National University Hospital, Kangwon National University School of Medicine, Chuncheon, Korea. pulmo2@kangwon.ac.kr
- KMID: 2320701
- DOI: http://doi.org/10.4046/trd.2015.78.4.326
Abstract
- BACKGROUND
Asian dust is known to have harmful effects on the respiratory system. Respiratory conditions are also influenced by environmental conditions regardless of the presence of pollutants. The same pollutant can have different effects on the airway when the air is dry compared with when it is humid. We investigated hospital visits for chronic obstructive pulmonary disease (COPD) and asthma in relation to the environmental conditions.
METHODS
We conducted a retrospective study using the Korean National Health Insurance Service claims database of patients who visited hospitals in Chuncheon between January 2006 and April 2012. Asian dust, haze, mist, and fog days were determined using reports from the Korea Meteorological Administration. Hospital visits for asthma or COPD on the index days were compared with the comparison days. We used two-way case-crossover techniques with one to two matching.
RESULTS
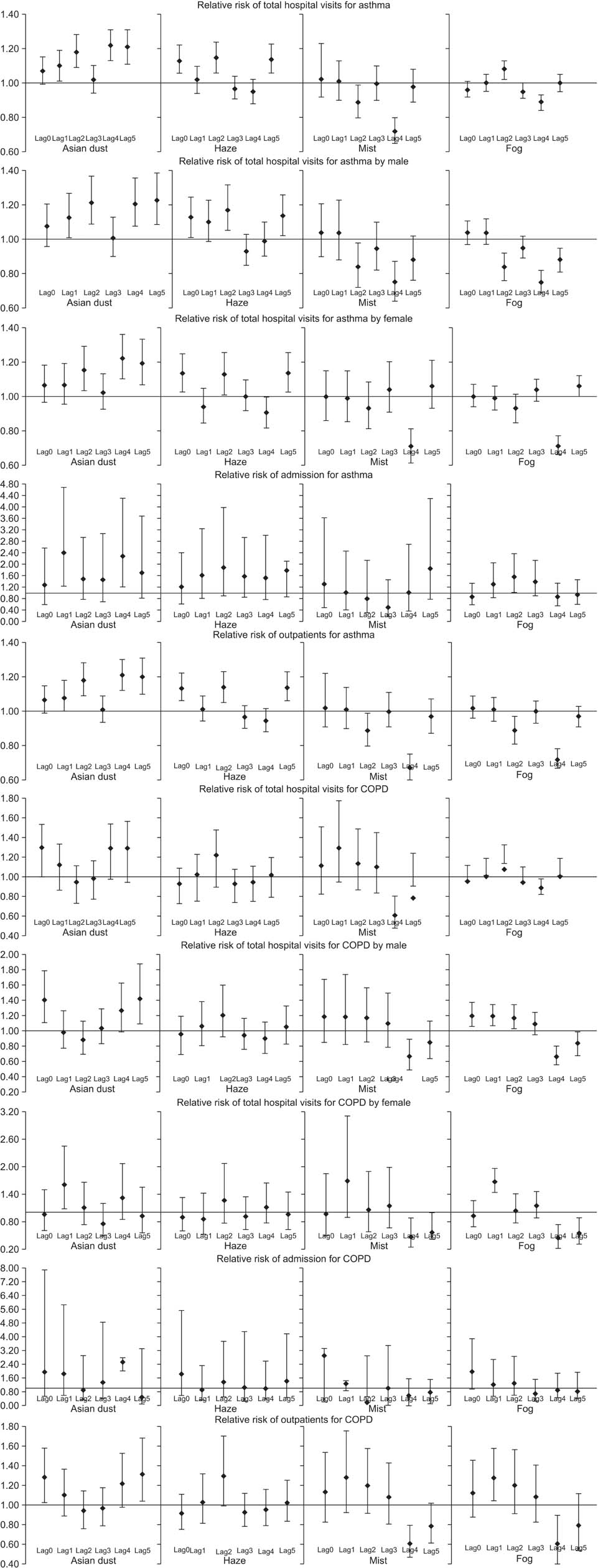
The mean hospital visits for asthma and COPD were 59.37 +/- 34.01 and 10.04 +/- 6.18 per day, respectively. Hospital visits for asthma significantly increased at lag0 and lag1 for Asian dust (relative risk [RR], 1.10; 95% confidence interval [CI], 1.01-1.19; p<0.05) and haze (RR, 1.13; 95% CI, 1.06-1.22; p<0.05), but were significantly lower on misty (RR, 0.89; 95% CI, 0.80-0.99; p<0.05) and foggy (RR, 0.89; 95% CI, 0.84-0.93; p<0.05) days than on control days. The hospital visits for COPD also significantly increased on days with Asian dust (RR, 1.29; 95% CI, 1.05-1.59; p<0.05), and were significantly lower at lag4 for foggy days, compared with days without fog (RR, 0.85; 95% CI, 0.75-0.97; p<0.05).
CONCLUSION
Asian dust showed an association with airway diseases and had effects for several days after the exposure. In contrast to Asian dust, mist and fog, which occur in humid air conditions, showed the opposite effects on airway diseases, after adjusting to the pollutants. It would require more research to investigate the effects of various air conditions on airway diseases.
Keyword
MeSH Terms
Figure
Reference
-
1. Csavina J, Field J, Taylor MP, Gao S, Landazuri A, Betterton EA, et al. A review on the importance of metals and metalloids in atmospheric dust and aerosol from mining operations. Sci Total Environ. 2012; 433:58–73.2. Ewing SA, Christensen JN, Brown ST, Vancuren RA, Cliff SS, Depaolo DJ. Pb isotopes as an indicator of the Asian contribution to particulate air pollution in urban California. Environ Sci Technol. 2010; 44:8911–8916.3. Park JW, Lim YH, Kyung SY, An CH, Lee SP, Jeong SH, et al. Effects of ambient particulate matter on peak expiratory flow rates and respiratory symptoms of asthmatics during Asian dust periods in Korea. Respirology. 2005; 10:470–476.4. Watanabe M, Yamasaki A, Burioka N, Kurai J, Yoneda K, Yoshida A, et al. Correlation between Asian dust storms and worsening asthma in Western Japan. Allergol Int. 2011; 60:267–275.5. Chiu HF, Tiao MM, Ho SC, Kuo HW, Wu TN, Yang CY. Effects of Asian dust storm events on hospital admissions for chronic obstructive pulmonary disease in Taipei, Taiwan. Inhal Toxicol. 2008; 20:777–781.6. Tam WW, Wong TW, Wong AH, Hui DS. Effect of dust storm events on daily emergency admissions for respiratory diseases. Respirology. 2012; 17:143–148.7. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001; 163:1256–1276.8. Handzel ZT. Effects of environmental pollutants on airways, allergic inflammation, and the immune response. Rev Environ Health. 2000; 15:325–336.9. Muhlfeld C, Rothen-Rutishauser B, Blank F, Vanhecke D, Ochs M, Gehr P. Interactions of nanoparticles with pulmonary structures and cellular responses. Am J Physiol Lung Cell Mol Physiol. 2008; 294:L817–L829.10. Sapey E, Stockley RA. COPD exacerbations. 2: aetiology. Thorax. 2006; 61:250–258.11. Chauhan AJ, Johnston SL. Air pollution and infection in respiratory illness. Br Med Bull. 2003; 68:95–112.12. Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007; 370:786–796.13. Chung YS, Kim HS, Yoon MB. Observations of visibility and chemical compositions related to fog, mist and haze in South Korea. Water Air Soil Pollut. 1999; 111:139–157.14. Lumb AB. Nunn's applied respiratory physiology. 7th ed. London: Elsevier Health Sciences;2012.15. Gyan K, Henry W, Lacaille S, Laloo A, Lamsee-Ebanks C, McKay S, et al. African dust clouds are associated with increased paediatric asthma accident and emergency admissions on the Caribbean island of Trinidad. Int J Biometeorol. 2005; 49:371–376.16. Hackney JD, Linn WS, Avol EL. Potential risks to human respiratory health from "acid fog": evidence from experimental studies of volunteers. Environ Health Perspect. 1985; 63:57–61.17. Kanatani KT, Ito I, Al-Delaimy WK, Adachi Y, Mathews WC, Ramsdell JW, et al. Desert dust exposure is associated with increased risk of asthma hospitalization in children. Am J Respir Crit Care Med. 2010; 182:1475–1481.18. Lee JT, Son JY, Cho YS. A comparison of mortality related to urban air particles between periods with Asian dust days and without Asian dust days in Seoul, Korea, 2000-2004. Environ Res. 2007; 105:409–413.19. Garcia-Aymerich J, Tobias A, Anto JM, Sunyer J. Air pollution and mortality in a cohort of patients with chronic obstructive pulmonary disease: a time series analysis. J Epidemiol Community Health. 2000; 54:73–74.20. Higgins BG, Francis HC, Yates CJ, Warburton CJ, Fletcher AM, Reid JA, et al. Effects of air pollution on symptoms and peak expiratory flow measurements in subjects with obstructive airways disease. Thorax. 1995; 50:149–155.21. Kan H, Chen B. A case-crossover analysis of air pollution and daily mortality in Shanghai. J Occup Health. 2003; 45:119–124.22. Schwartz J, Dockery DW. Increased mortality in Philadelphia associated with daily air pollution concentrations. Am Rev Respir Dis. 1992; 145:600–604.23. Tellez-Rojo MM, Romieu I, Ruiz-Velasco S, Lezana MA, Hernandez-Avila MM. Daily respiratory mortality and PM10 pollution in Mexico City: importance of considering place of death. Eur Respir J. 2000; 16:391–396.24. Arbex MA, de Souza Conceicao GM, Cendon SP, Arbex FF, Lopes AC, Moyses EP, et al. Urban air pollution and chronic obstructive pulmonary disease-related emergency department visits. J Epidemiol Community Health. 2009; 63:777–783.25. Ko FW, Hui DS. Air pollution and chronic obstructive pulmonary disease. Respirology. 2012; 17:395–401.26. Anto JM, Vermeire P, Vestbo J, Sunyer J. Epidemiology of chronic obstructive pulmonary disease. Eur Respir J. 2001; 17:982–994.27. Holguin F. T raffic related exposures and lung function in adults. Thorax. 2007; 62:837–838.28. Long W, Tate RB, Neuman M, Manfreda J, Becker AB, Anthonisen NR. Respiratory symptoms in a susceptible population due to burning of agricultural residue. Chest. 1998; 113:351–357.29. Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000; 117:5 Suppl 2. 398S–401S.30. Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008; 359:2355–2365.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Toxicity and health effects of Asian dust: a literature review
- Effect of the Asian Dust Events on Respiratory Disease During the Spring
- Perceptions of the Asian Dust: Analysis of the Newspaper Articles about the Asian Dust
- Acute Effects of Asian Dust Events on Respiratory Symptoms and Peak Expiratory Flow in Children with Mild Asthma
- The Health Effects of Asian Dust Event