Tuberc Respir Dis.
2014 Aug;77(2):85-89. 10.4046/trd.2014.77.2.85.
A Case of IgG4-Related Lung Disease Presenting as Interstitial Lung Disease
- Affiliations
-
- 1Department of Internal Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. jwsong@amc.seoul.kr
- 2Department of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 3Department of Pathology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 2320544
- DOI: http://doi.org/10.4046/trd.2014.77.2.85
Abstract
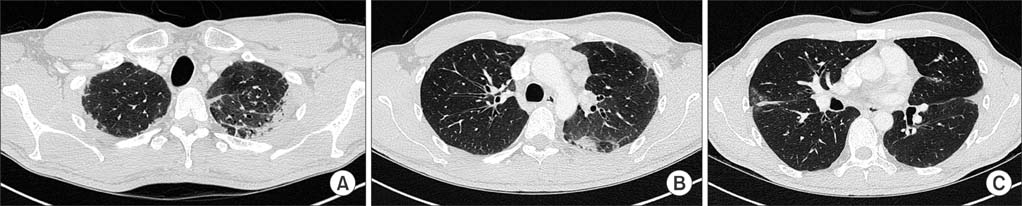
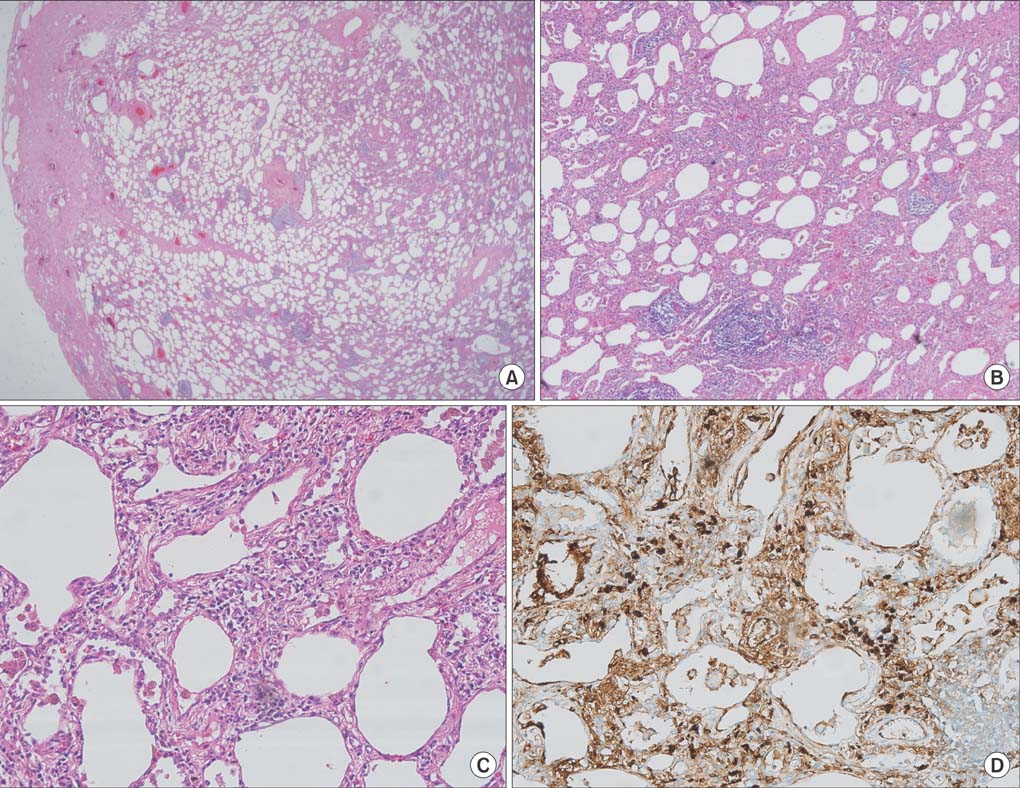
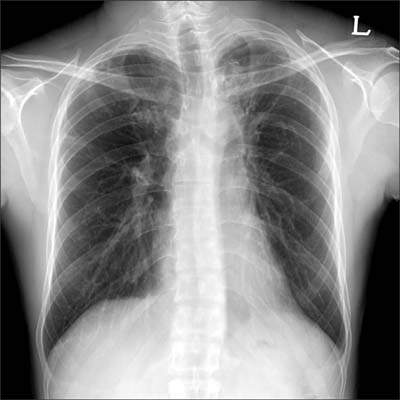
- Intrathoracic involvement of immunoglobulin G4 (IgG4)-related disease has recently been reported. However, a subset of the disease presenting as interstitial lung disease is rare. Here, we report a case of a 35-year-old man with IgG4-related lung disease with manifestations similar to those of interstitial lung disease. Chest computed tomography showed diffuse ground glass opacities and rapidly progressive pleural and subpleural fibrosis in both upper lobes. Histological findings showed diffuse interstitial lymphoplasmacytic infiltration with an increased number of IgG4-positive plasma cells. Serum levels of IgG and IgG4 were also increased. The patient was diagnosed with IgG4-related lung disease, treated with anti-inflammatory agents, and showed improvement. Lung involvement of IgG4-related disease can present as interstitial lung disease and, therefore, should be differentiated when evaluating interstitial lung disease.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Rare Case of Adenosquamous Carcinoma Arising in the Background of IgG4-Related Lung Disease
Sangjoon Choi, Sujin Park, Man Pyo Chung, Tae Sung Kim, Jong Ho Cho, Joungho Han
J Pathol Transl Med. 2019;53(3):188-191. doi: 10.4132/jptm.2019.02.21.
Reference
-
1. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012; 366:539–551.2. Shrestha B, Sekiguchi H, Colby TV, Graziano P, Aubry MC, Smyrk TC, et al. Distinctive pulmonary histopathology with increased IgG4-positive plasma cells in patients with autoimmune pancreatitis: report of 6 and 12 cases with similar histopathology. Am J Surg Pathol. 2009; 33:1450–1462.3. Zen Y, Inoue D, Kitao A, Onodera M, Abo H, Miyayama S, et al. IgG4-related lung and pleural disease: a clinicopathologic study of 21 cases. Am J Surg Pathol. 2009; 33:1886–1893.4. Fujinaga Y, Kadoya M, Kawa S, Hamano H, Ueda K, Momose M, et al. Characteristic findings in images of extra-pancreatic lesions associated with autoimmune pancreatitis. Eur J Radiol. 2010; 76:228–238.5. Duvic C, Desrame J, Leveque C, Nedelec G. Retroperitoneal fibrosis, sclerosing pancreatitis and bronchiolitis obliterans with organizing pneumonia. Nephrol Dial Transplant. 2004; 19:2397–2399.6. Takato H, Yasui M, Ichikawa Y, Fujimura M, Nakao S, Zen Y, et al. Nonspecific interstitial pneumonia with abundant IgG4-positive cells infiltration, which was thought as pulmonary involvement of IgG4-related autoimmune disease. Intern Med. 2008; 47:291–294.7. Tanaka K, Nagata K, Tomii K, Imai Y. A case of isolated IgG4-related interstitial pneumonia: a new consideration for the cause of idiopathic nonspecific interstitial pneumonia. Chest. 2012; 142:228–230.8. Taniguchi T, Ko M, Seko S, Nishida O, Inoue F, Kobayashi H, et al. Interstitial pneumonia associated with autoimmune pancreatitis. Gut. 2004; 53:770.9. Wibmer T, Kropf-Sanchen C, Rudiger S, Blanta I, Stoiber KM, Rottbauer W, et al. Isolated IgG4-related interstitial lung disease: unusual histological and radiological features of a pathologically proven case. Multidiscip Respir Med. 2013; 8:22.10. Yoo JW, Roh JH, Lim CM, Lee SD, Kim WS, Kim DS, et al. Two cases of pulmonary involvement of immunoglobulin G4 related autoimmune disease. Tuberc Respir Dis. 2009; 67:359–363.11. Kwon SH, Lee YK, Shim MS, Lee HI. A case of immunoglobulin G4-related sclerosing disease mimicking lung cancer. J Korean Soc Radiol. 2013; 69:53–56.12. Park HY, Han J, Kang G, Yi CA, Chung MP. IgG4-related lung disease presenting as a consolidative mass: a case report. J Lung Cancer. 2010; 9:103–105.13. Choi IH, Jang SH, Lee S, Han J, Kim TS, Chung MP. A case report of IgG4-related disease clinically mimicking pleural mesothelioma. Tuberc Respir Dis. 2014; 76:42–45.14. Kim DH, Koh KH, Oh HS, Kim SJ, Kang SH, Jung BW, et al. A case of immunoglobulin g4-related disease presenting as a pleural mass. Tuberc Respir Dis. 2014; 76:38–41.15. Deshpande V, Zen Y, Chan JK, Yi EE, Sato Y, Yoshino T, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012; 25:1181–1192.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneously Regressed Immunoglobulin IgG4-related Lung Disease Presenting as Multiple Cavitary Nodules
- A Case of IgG4-Related Lung Disease Mimicking Non-Specific Interstitial Pneumonia
- A Rare Case of Adenosquamous Carcinoma Arising in the Background of IgG4-Related Lung Disease
- Immunoglobulin G4-Related Lung Disease Mimicking Lung Cancer: Two Case Reports
- IgG4-Related Lung Disease Presenting as a Consolidative Mass: A Case Report