Tuberc Respir Dis.
2014 Mar;76(3):127-130.
Effect of Rivaroxaban on Fibrinolytic Therapy in Massive Pulmonary Embolism: Two Cases
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University College of Medicine, Seoul, Korea. kyklung@schmc.ac.kr
Abstract
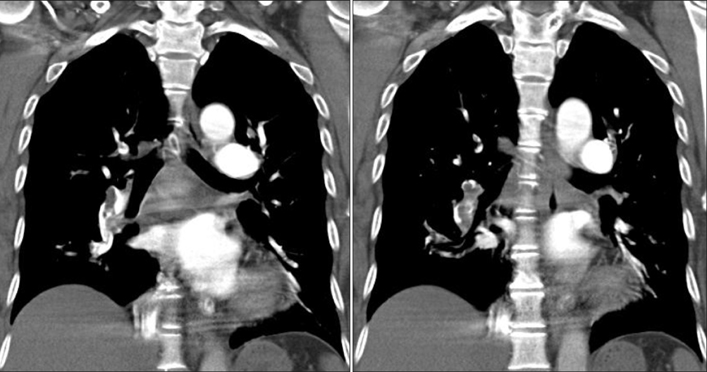
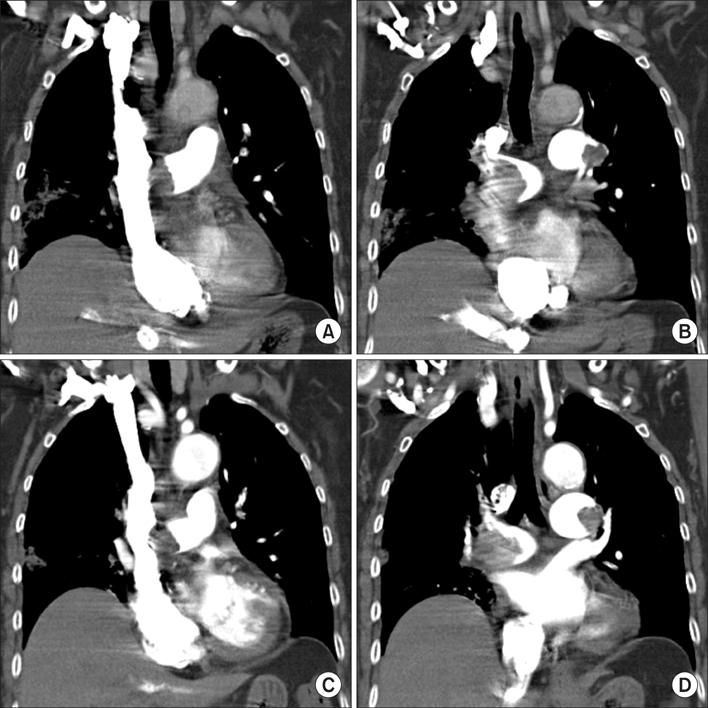
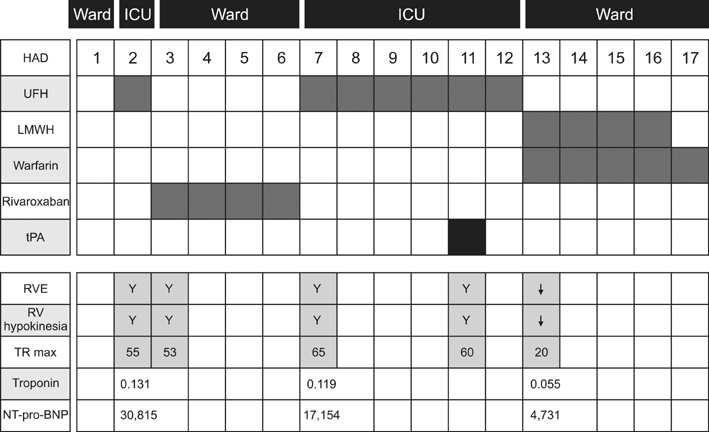
- The risk of dying from a pulmonary embolism (PE) is estimated to be about 30% if inotropic support is required and no cardiopulmonary arrest occurs. Fibrinolysis in massive PE is regarded as a life-saving intervention, unless there is a high risk of bleeding following the use of the fibrinolytic therapy. Rivaroxaban is an oral factor Xa inhibitor, however its anticoagulation effects before or after administration of fibrinolytics in massive PE are still unknown. Two patents were admitted: 61-year-old woman with repeated syncope, and a 73-year-old woman was admitted with dyspnea and poor oral intake. Systemic arterial hypotension with radiologic confirmation led to a diagnosis of massive PE in both patients. Rivaroxaban was administered before in one, and after firbrinolytic therapy in the other. One showed similar efficacy of rivaroxaban with currently used anticoagulants after successful fibrinolysis, and the other one without antecedent administration of the fibrinolytic agent showed unfavorable efficacy of rivaroxaban.
Keyword
MeSH Terms
Figure
Reference
-
1. Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011; 123:1788–1830.2. Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012; 141:e419S–e494S.3. Piazza G, Goldhaber SZ. Fibrinolysis for acute pulmonary embolism. Vasc Med. 2010; 15:419–428.4. EINSTEIN-PE Investigators. Büller HR, Prins MH, Lensin AW, Decousus H, Jacobson BF, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012; 366:1287–1297.5. EINSTEIN Investigators. Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010; 363:2499–2510.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Use of Thrombolytics for Massive Pulmonary Embolism by a Comparison of Cases
- Acute Massive Pulmonary Thromboembolism Occupying both Whole Pulmonary Arteries
- Acute Massive Pulmonary Embolism Improved by rt-PA Thrombolytic Therapy -Two Cases of Report-
- Short-term effects of fibrinolytic therapy on the hemodynamic parameters of patients with intermediate- and high-risk pulmonary embolism
- Thrombotic Occlusion of an Inferior Vena Cava Filter during Maintenance with a Novel Anticoagulant