Tuberc Respir Dis.
2013 Oct;75(4):170-173.
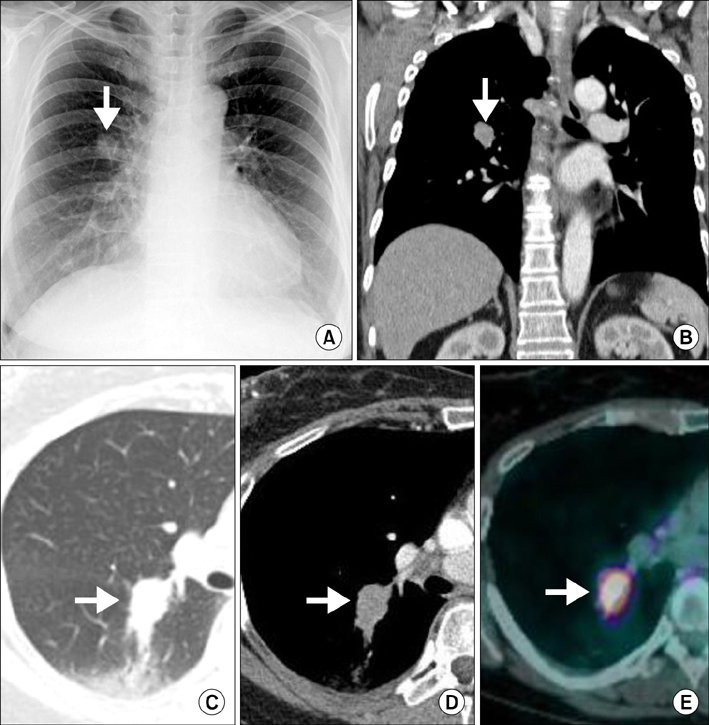
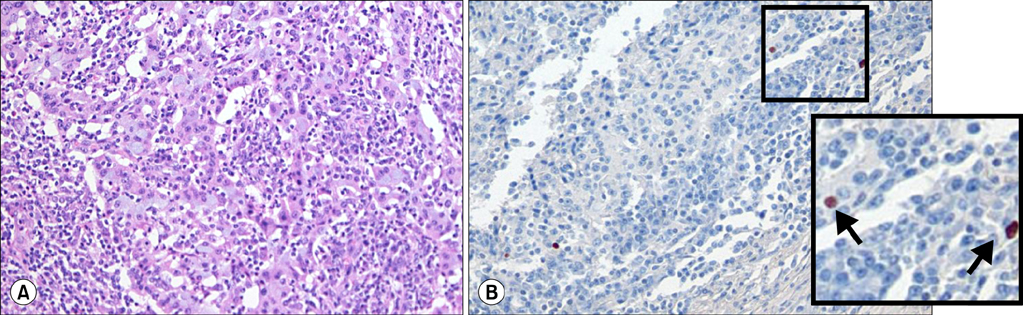
A Case of Primary Pulmonary Lymphoepithelioma-like Carcinoma Misdiagnosed as Adenocarcinoma
- Affiliations
-
- 1Department of Internal Medicine, Chonbuk National University Medical School, Jeonju, Korea. leeyc@jbnu.ac.kr
- 2Research Center for Pulmonary Disorders, Chonbuk National University Medical School, Jeonju, Korea.
- 3Department of Pathology, Chonbuk National University Medical School, Jeonju, Korea.
Abstract
- Primary pulmonary lymphoepithelioma-like carcinoma (LELC) is rare, with a more favorable prognosis compared with that of other types of non-small cell lung cancers. Herein, we describe an interesting case of primary pulmonary LELC confirmed postoperatively, which had been initially diagnosed as poorly differentiated adenocarcinoma. We suggest that despite the rarity of pulmonary LELC, it should be included as one of the differential diagnoses for lung malignancies. Physicians should consider taking a larger biopsy, especially when histologic examination shows undifferentiated nature.
MeSH Terms
Figure
Reference
-
1. Begin LR, Eskandari J, Joncas J, Panasci L. Epstein-Barr virus related lymphoepithelioma-like carcinoma of lung. J Surg Oncol. 1987; 36:280–283.2. Ho JC, Wong MP, Lam WK. Lymphoepithelioma-like carcinoma of the lung. Respirology. 2006; 11:539–545.3. Jung CY, Shim SW, Park CK, Kwon KY, Jeon YJ. A case of lymphoepithelioma-like carcinoma of the lung. Tuberc Respir Dis. 2011; 71:363–367.4. Wei WI, Sham JS. Nasopharyngeal carcinoma. Lancet. 2005; 365:2041–2054.5. Huang CJ, Feng AC, Fang YF, Ku WH, Chu NM, Yu CT, et al. Multimodality treatment and long-term follow-up of the primary pulmonary lymphoepithelioma-like carcinoma. Clin Lung Cancer. 2012; 13:359–362.6. Liang Y, Wang L, Zhu Y, Lin Y, Liu H, Rao H, et al. Primary pulmonary lymphoepithelioma-like carcinoma: fifty-two patients with long-term follow-up. Cancer. 2012; 118:4748–4758.7. Hayashi T, Haba R, Tanizawa J, Katsuki N, Kadota K, Miyai Y, et al. Cytopathologic features and differential diagnostic considerations of primary lymphoepithelioma-like carcinoma of the lung. Diagn Cytopathol. 2012; 40:820–825.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mixed lymphoepithelioma-like carcinoma and adenocarcinoma of the gallbladder
- Lymphoepithelioma-like Carcinoma of the Renal Pelvis
- A Case of Lymphoepithelioma - Like Carcinoma of Uterine Cervix
- A Case of Lymphoepithelioma-Like Carcinoma in the Thyroid Gland
- Epstein-Barr Virus-associated Mixed Lymphoepithelioma-like Carcinoma and Adenocarcinoma of the Gall Bladder: An Unusual Entity