Tuberc Respir Dis.
2013 Aug;75(2):71-74.
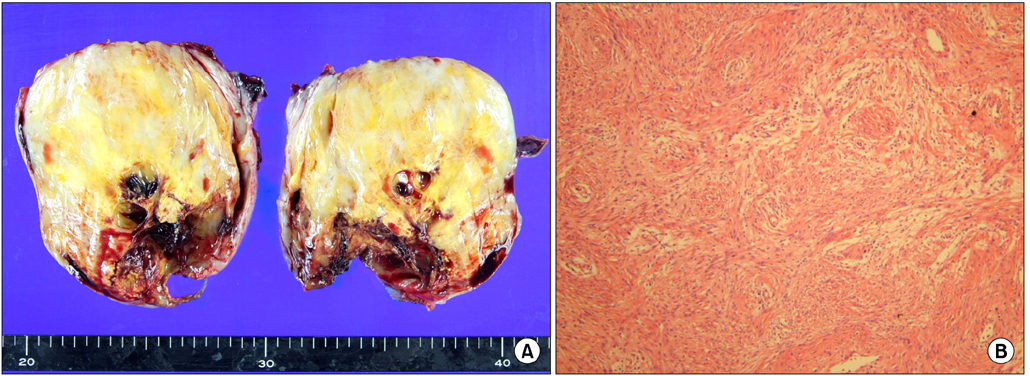
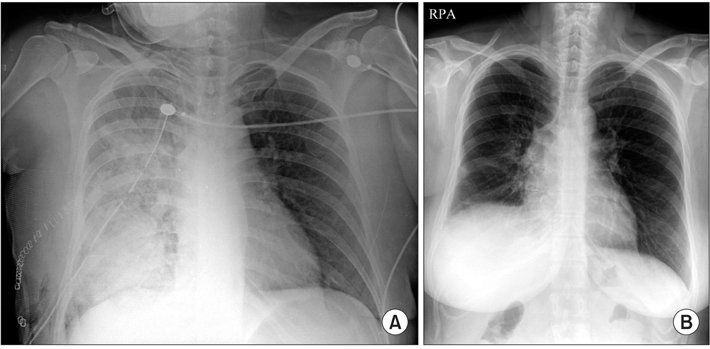
A Case of Giant, Benign Schwannoma Associated with Total Lung Collapse by Bloody Effusion
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea. jykimmd@cau.ac.kr
- 2Department of Chest Surgery, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Chung-Ang University College of Medicine, Seoul, Korea.
Abstract
- Benign schwannoma is the most common neurogenic tumor in the mediastinum. Mediastinal benign schwannomas are most often asymptomatic and rarely accompanied by bloody pleural effusion. In the clinical analysis of 7 cases of pulmonary schwannomas, pleural effusion, and blood invasion were evident in 3 patients with malignant schwannoma. Herein, we report a rare case of giant, benign schwannoma presented with total collapse of right lung by massive, bloody pleural effusion.
Keyword
Figure
Reference
-
1. Kim HG, Park SJ, Kwon SH, Hong SJ, Lee JS, Lee MS, et al. A case of schwannoma induced stenosis of superior mesenteric artery. Korean J Med. 2004; 66:86–90.2. Shao J, Zhu XH, Shi JY, Ma J, Ge XJ, You ZQ. Primary pulmonary schwannoma: clinical analysis of 7 cases and review of the literature. Zhonghua Jie He He Hu Xi Za Zhi. 2003; 26:3–6.3. Marchevsky AM. Mediastinal tumors of peripheral nervous system origin. Semin Diagn Pathol. 1999; 16:65–78.4. Fatimi SH, Bawany SA, Ashfaq A. Ganglioneuroblastoma of the posterior mediastinum: a case report. J Med Case Rep. 2011; 5:322.5. Kambayashi T, Suzuki T. Neurogenic tumors originated from vagus nerve and intercostal nerve simultaneously; report of a case. Kyobu Geka. 2011; 64:516–519.6. Lin MW, Chang YL, Lee YC, Huang PM. Non-functional paraganglioma of the posterior mediastinum. Interact Cardiovasc Thorac Surg. 2009; 9:540–542.7. Kato M, Shiota S, Shiga K, Takagi H, Mori H, Sekiya M, et al. Benign giant mediastinal schwannoma presenting as cardiac tamponade in a woman: a case report. J Med Case Rep. 2011; 5:61.8. Ishibashi H, Akamatsu H, Sunamori M, Komori H, Shirasawa S, Nomoto S. A case of giant dumbbell shaped schwannoma with massive pleural effusion. Kyobu Geka. 2001; 54:742–746.9. Cho JH, Kim KU, Park HK, Jeong YJ, Kim YD, Kim YS, et al. Two cases of benign solitary schwannoma with pleural effusion. Tuberc Respir Dis. 2007; 63:78–82.10. Miravitlles M, de Gracia J, Roca-Tey R, Monso E. Pleural effusion secondary to a malignant thoracic schwannoma. Med Clin (Barc). 1992; 99:117.11. Hazelrigg SR, Boley TM, Krasna MJ, Landreneau RJ, Yim AP. Thoracoscopic resection of posterior neurogenic tumors. Am Surg. 1999; 65:1129–1133.