Tuberc Respir Dis.
2012 Apr;72(4):360-366.
Four Year Trend of Carbapenem-Resistance in Newly Opened ICUs of a University-Affiliated Hospital of South Korea
- Affiliations
-
- 1Division of Pulmonary and Allergy, Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea. jykimmd@cau.ac.kr
Abstract
- BACKGROUND
Carbapenem-resistance is rapidly evolving among the pathogenic microbes in intensive care units (ICUs). This study aimed to determine annual trend of carbapenem-resistance in the ICU for 4 years, since the opening of a university-affiliated hospital in South Korea.
METHODS
From 2005 to 2008, microbial samples from consecutive 6,772 patients were screened in the ICU. Three hundred and ninety-seven patients (5.9%) and their first isolates of carbapenem-resistant pathogens were analyzed.
RESULTS
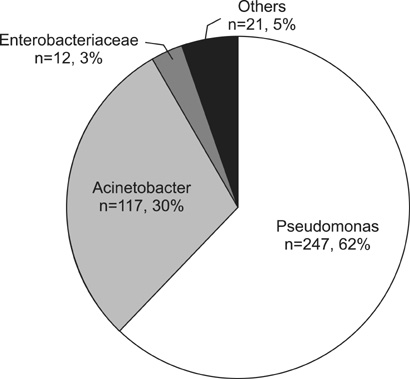
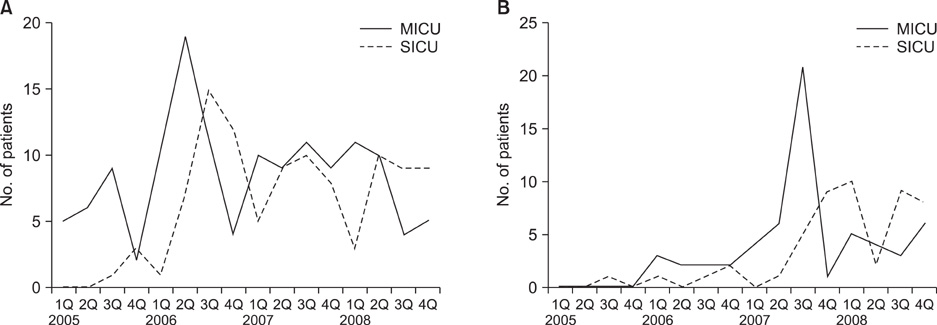
The percentage of patients infected with carbapenem-resistant organisms increased constantly during the initial three years (2.3% in 2005, 6.2% in 2006, 7.8% in 2007), then it declined to 6.5% in 2008. Acute Physiology and Chronic Health Evaluation (APACHE) III score at admission was 58.0+/-23.5, the median length of the ICU stay was 37 days, and the mortality rate was 37.5%. The sampling sites were endotracheal suction (67%), catheterized urine (17%), wound (6%) and others (10%). Bacteria with carbapenem-resistance were Pseudomonas aeruginosa (247 isolates, 62%), Acinetobacter baumannii (117 isolates, 30%), Enterobacteriaceae (12 isolates, 3%), and others (21, 5%). Of note, peak isolation of carbapenem-resistant microorganisms in medical ICU was followed by the same epidemic at surgical ICU.
CONCLUSION
Taken together, carbapenem-resistant pathogens are of growing concern in the ICU.
MeSH Terms
Figure
Reference
-
1. Gaynes R, Edwards JR. National Nosocomial Infections Surveillance System. Overview of nosocomial infections caused by gram-negative bacilli. Clin Infect Dis. 2005. 41:848–854.2. Song JH. Current status and future strategies of antimicrobial resistance in Korea. Korean J Med. 2009. 77:143–151.3. Neuhauser MM, Weinstein RA, Rydman R, Danziger LH, Karam G, Quinn JP. Antibiotic resistance among gram-negative bacilli in US intensive care units: implications for fluoroquinolone use. JAMA. 2003. 289:885–888.4. Paterson DL, Ko WC, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H, et al. Antibiotic therapy for Klebsiella pneumoniae bacteremia: implications of production of extended-spectrum beta-lactamases. Clin Infect Dis. 2004. 39:31–37.5. Lee K, Lee HS, Jang SJ, Park AJ, Lee MH, Song WK, et al. Antimicrobial resistance surveillance of bacteria in 1999 in Korea with a special reference to resistance of enterococci to vancomycin and gram-negative bacilli to third generation cephalosporin, imipenem, and fluoroquinolone. J Korean Med Sci. 2001. 16:262–270.6. Dubois V, Arpin C, Melon M, Melon B, Andre C, Frigo C, et al. Nosocomial outbreak due to a multiresistant strain of Pseudomonas aeruginosa P12: efficacy of cefepime-amikacin therapy and analysis of beta-lactam resistance. J Clin Microbiol. 2001. 39:2072–2078.7. Rhomberg PR, Jones RN. Contemporary activity of meropenem and comparator broad-spectrum agents: MYSTIC program report from the United States component (2005). Diagn Microbiol Infect Dis. 2007. 57:207–215.8. Agodi A, Zarrilli R, Barchitta M, Anzaldi A, Di Popolo A, Mattaliano A, et al. Alert surveillance of intensive care unit-acquired Acinetobacter infections in a Sicilian hospital. Clin Microbiol Infect. 2006. 12:241–247.9. Winokur PL, Canton R, Casellas JM, Legakis N. Variations in the prevalence of strains expressing an extended-spectrum beta-lactamase phenotype and characterization of isolates from Europe, the Americas, and the Western Pacific region. Clin Infect Dis. 2001. 32:Suppl 2. S94–S103.10. WHO Collaborating Centre for Drug Statistics Methodology [Internet]. World Health Organization. 2011. cited 2011 Dec 1. Oslo: WHO;Available from: http://www.whocc.no/atcddd/.11. Norrby SR. Carbapenems. Med Clin North Am. 1995. 79:745–759.12. Brown S, Amyes S. OXA (beta)-lactamases in Acinetobacter: the story so far. J Antimicrob Chemother. 2006. 57:1–3.13. Lortholary O, Fagon JY, Hoi AB, Slama MA, Pierre J, Giral P, et al. Nosocomial acquisition of multiresistant Acinetobacter baumannii : risk factors and prognosis. Clin Infect Dis. 1995. 20:790–796.14. Richards MJ, Edwards JR, Culver DH, Gaynes RP. National Nosocomial Infections Surveillance System. Nosocomial infections in medical intensive care units in the United States. Crit Care Med. 1999. 27:887–892.15. Crespo MP, Woodford N, Sinclair A, Kaufmann ME, Turton J, Glover J, et al. Outbreak of carbapenem-resistant Pseudomonas aeruginosa producing VIM-8, a novel metallo-beta-lactamase, in a tertiary care center in Cali, Colombia. J Clin Microbiol. 2004. 42:5094–5101.16. Agarwal R, Gupta D, Ray P, Aggarwal AN, Jindal SK. Epidemiology, risk factors and outcome of nosocomial infections in a Respiratory Intensive Care Unit in North India. J Infect. 2006. 53:98–105.17. Pournaras S, Markogiannakis A, Ikonomidis A, Kondyli L, Bethimouti K, Maniatis AN, et al. Outbreak of multiple clones of imipenem-resistant Acinetobacter baumannii isolates expressing OXA-58 carbapenemase in an intensive care unit. J Antimicrob Chemother. 2006. 57:557–561.18. Koeleman JG, Parlevliet GA, Dijkshoorn L, Savelkoul PH, Vandenbroucke-Grauls CM. Nosocomial outbreak of multi-resistant Acinetobacter baumannii on a surgical ward: epidemiology and risk factors for acquisition. J Hosp Infect. 1997. 37:113–123.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antibiotic Resistance for Common Hospital Acquired-pneumonia Pathogens in the Intensive Care Unit of Newly Opened Hospital
- ISAba15 Inserted into Outer Membrane Protein Gene carO in Acinetobacter baumannii
- Carbapenem-resistant Enterobacteriaceae in Korea
- Antimicrobial Therapy for Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria
- Correlation between Carbapenem Prescription Trends and Imipenem Resistance in Acinetobacter baumannii at an Intensive Care Unit between 2006 and 2010