Tuberc Respir Dis.
2011 Jan;70(1):74-78.
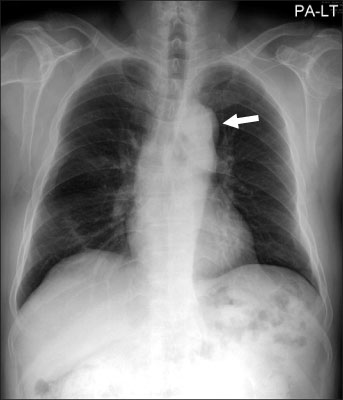
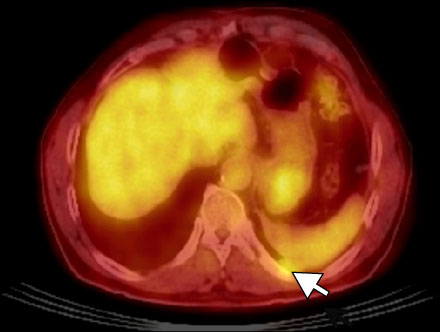
A Case of Pleural Metastasis 6 Years after Complete Surgical Resection of Invasive Thymoma
- Affiliations
-
- 1Department of Respiratory and Allergy Medicine, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea. uhs@hosp.sch.ac.kr
- 2Department of Pathology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- 3Department of, Diagnostic Radioloy, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- 4Department of Respiratory and Allergy Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea.
- 5Department of Respiratory and Allergy Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
Abstract
- Herein, we report a case of recurrent pleural metastasis after complete resection of invasive thymoma that was successfully treated with surgical resection. Thymoma and thymic carcinoma are uncommon neoplasms derived from the epithelial cells of the thymus. Approximately 30% to 50% of thymomas are asymptomatic at the time of diagnosis. However, these cancers may present with constitutional or local pressure symptoms and sometimes with paraneoplastic syndromes, especially myasthenia gravis. Surgical resection is the mainstay of thymoma treatment and has been shown to remarkably improve long-term survival. Despite complete resection, local recurrences are frequent, and surgery is the cornerstone of therapy even in cases of recurrent thymoma. We experienced a 67-year-old male patient with pleural metastasis that developed 6 years after complete surgical resection of invasive thymoma. The pleural mass was excised by video-assisted thoracoscopic surgery. Histopathological examination revealed an invasive World Health Organization (WHO) type B2 thymoma.
MeSH Terms
Figure
Reference
-
1. Debnath J, Chawla N, Talwar R, Vohra LS, George RA, Singh HP, et al. Pleural and transdiaphragmatic retroperitoneal metastasis developing two and half years after resection of invasive thymoma. Singapore Med J. 2008. 49:e64–e67.2. Awad WI, Symmans PJ, Dussek JE. Recurrence of stage I thymoma 32 years after total excision. Ann Thorac Surg. 1998. 66:2106–2108.3. Gielda BT, Peng R, Coleman JL, Thomas CR, Cameron RB. Treatment of early stage thymic tumors: surgery and radiation therapy. Curr Treat Options Oncol. 2008. 9:259–268.4. Kondo K. Optimal therapy for thymoma. J Med Invest. 2008. 55:17–28.5. Kurup A, Loehrer PJ Sr. Thymoma and thymic carcinoma: therapeutic approaches. Clin Lung Cancer. 2004. 6:28–32.6. Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest. 2005. 128:2893–2909.7. Song HS, Han SB, Kang YW, Jeon YJ, Kim H, Lee SS. Invasive thymoma. Korean J Intern Med. 1987. 33:548–556.8. Vaideeswar P, Padmanabhan A, Deshpande JR, Pandit SP. Thymoma: a pathological study of 50 cases. J Postgrad Med. 2004. 50:94–97.9. Welsh JS, Thurman SA, Howard SP. Thymoma and multiple malignancies: a case of five synchronous neoplasms and literature review. Clin Med Res. 2003. 1:227–232.10. Suster S, Moran CA. Thymoma classification: current status and future trends. Am J Clin Pathol. 2006. 125:542–554.11. Tomaszek S, Wigle DA, Keshavjee S, Fischer S. Thymomas: review of current clinical practice. Ann Thorac Surg. 2009. 87:1973–1980.12. Sakada T, Sugio K, Nishioka K, Tsukamoto S, Ushijima C, Yamazaki K, et al. Invasive thymoma with long-term survival by extensive reoperation. Respiration. 1999. 66:167–169.13. Reddy RH, Shah R, Kumar B, Thorpe JA. Recurrence of stage I thymoma in sternum, 13 years after "complete" excision. Eur J Cardiothorac Surg. 2003. 23:134–135.14. Nomori H, Watanabe K, Ohtsuka T, Naruke T, Suemasu K, Orikasa H, et al. Pulmonary metastasis 12 years after resection of thymoma with microscopic capsule invasion. Jpn J Clin Oncol. 2004. 34:630–633.15. Lucchi M, Basolo F, Mussi A. Surgical treatment of pleural recurrence from thymoma. Eur J Cardiothorac Surg. 2008. 33:707–711.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Resection of Hepatic Metastasis of Thymoma
- Malignant Solitary Fibrous Tumor in Anterior Mediastinum with Pleural Metastasis Simulating Invasive Thymoma
- A Case of Distal Seeding of Invasive Thymoma
- Surgical Treatment of Thymoma
- Empyema and Pericarditis by Salmonella Group D Complicating Malignant Thymoma with Pleural Metastasis: A case report