Tuberc Respir Dis.
2010 Jan;68(1):29-33.
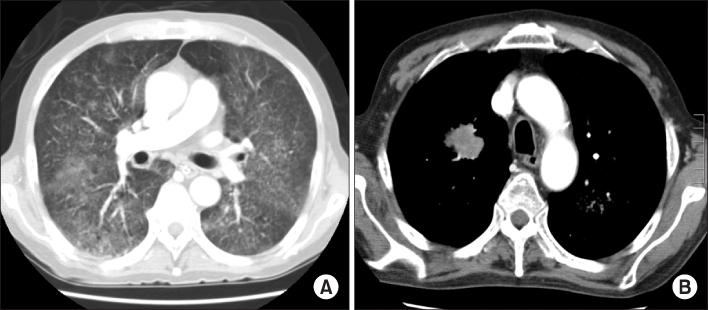
A Case of Fatal Hyperinfective Strongyloidiasis with Acute Respiratory Failure and Intestinal Perforation in Lung Cancer Patient
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University School of Medicine, Jinju, Korea. dr202202@yahoo.co.kr
Abstract
- Strongyloides stercoralis is an intestinal nematode that is a parasite to humans. The infecting filariform larvae of S. stercoralis enters the host body via the bloodstream, passes through the lungs, penetrates the alveoli, and then ascends the airway to transit down the esophagus into the small bowel. The infection can persist for decades without causing major symptoms and can elicit eosinophilia of varying magnitudes. Of note, this infection can also develop into a disseminated, often fatal, disease (hyperinfection) in patients receiving immunosuppressive corticosteroids. A 65-year-old man who was receiving corticosteroid therapy for the treatment of spinal stenosis was admitted to the emergency room with complaints of abdominal pain and severe dyspnea. We detected many S. stercoralis larvae in the sputum and in the bronchoalveolar-lavage sample collected by bronchoscopy. Here, we report a fatal case of strongyloidiasis with acute respiratory failure and intestinal perforation. In addition, we provide a brief review of the relevant medical literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Segarra-Newnham M. Manifestations, diagnosis, and treatment of Strongyloides stercoralis infection. Ann Pharmacother. 2007. 41:1992–2001.2. Pearlman E. Mahmoud AA, editor. Pathogenesis and immunity in helminthic infection. Parasitic lung diseases. 1997. New York: Marcel Dekker;33–46.3. Keiser PB, Nutman TB. Strongyloides stercoralis in the immunocompromised population. Clin Microbiol Rev. 2004. 17:208–217.4. Weller PF. Adkinson NF, Busse WW, Bochner BS, Holgate ST, Simons FE, Lemanske RF, editors. Eosinophilia and eosinophil-related disorders. Middleton's allergy: principles & practice. 2009. 7th ed. Philadelphia: Mosby;859–877.5. Siddiqui AA, Berk SL. Diagnosis of Strongyloides stercoralis infection. Clin Infect Dis. 2001. 33:1040–1047.6. Wehner JH, Kirsch CM. Pulmonary manifestations of strongyloidiasis. Semin Respir Infect. 1997. 12:122–129.7. Mahmoud AA. Strongyloidiasis. Clin Infect Dis. 1996. 23:949–952.8. Fishman JA. Fishman AP, Elias JA, Fishman JA, Grippi MA, Senior RM, Pack AI, editors. Helminthic diseases of the lungs. Fishman's pulmonary diseases and disorders. 2008. 4th ed. New York: McGraw-Hill;2413–2426.9. Newberry AM, Williams DN, Stauffer WM, Boulware DR, Hendel-Paterson BR, Walker PF. Strongyloides hyperinfection presenting as acute respiratory failure and gram negative sepsis. Chest. 2005. 128:3681–3684.10. Feldman M, Friedman LS, Sleisenger MH. Sleisenger & Fordtran's gastrointestinal and liver disease. 2002. 7th ed. Philadelphia: W.B. Saunders;1954–1955.11. Wilson ME, Weller PF. Guerrant RL, Walker DH, Weller PF, editors. Eosinophilia. Tropical infectious diseases: principles, pathogenesis, and practice. 2006. 2nd ed. Philadelphia: Churchill Livingstone;1478–1495.12. Savage D, Foadi M, Haworth C, Grant A. Marked eosinophilia in an immunosuppressed patient with strongyloidiasis. J Intern Med. 1994. 236:473–475.13. Gill GV, Bailey JW. Eosinophilia as a marker for chronic strongyloidiasis: use of a serum ELISA test to detect asymptomatic cases. Ann Trop Med Parasitol. 1989. 83:249–252.14. Igual-Adell R, Oltra-Alcaraz C, Soler-Company E, Sánchez-Sánchez P, Matogo-Oyana J, Rodríguez-Calabuig D. Efficacy and safety of ivermectin and thiabendazole in the treatment of strongyloidiasis. Expert Opin Pharmacother. 2004. 5:2615–2619.15. Satoh M, Kokaze A. Treatment strategies in controlling strongyloidiasis. Expert Opin Pharmacother. 2004. 5:2293–2301.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Steroid-induced Hyperinfective Strongyloidiasis with Bacterial Meningitis
- The Evaluation of Postoperative Acute Respiratory Failure in Primary Lung Cancer with Interstitial Pneumonia
- Gefitinib-induced Acute Fatal Respiratory Failure in a Woman who Never Smoked and had Adenocarinoma of the Lung with EGFR Mutation
- Small Bowel Perforation by a Fish Bone in Intestinal Obstruction: A Case Report
- Two Lethal Cases of Monomorphic Epitheliotropic Intestinal T-cell Lymphoma Deteriorated Rapidly After Emergency Surgery for Intestinal Perforation