Tuberc Respir Dis.
2009 Aug;67(2):127-130.
Pneumocystis jiroveci Pneumonia Mimicking Miliary Tuberculosis in a Kidney Transplanted Patient
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. shimts@amc.seoul.kr
Abstract
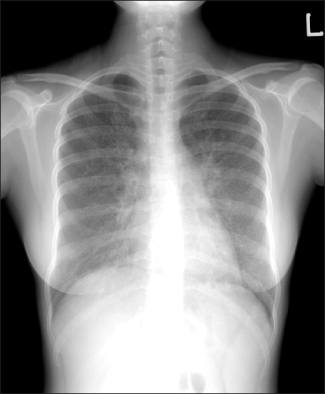
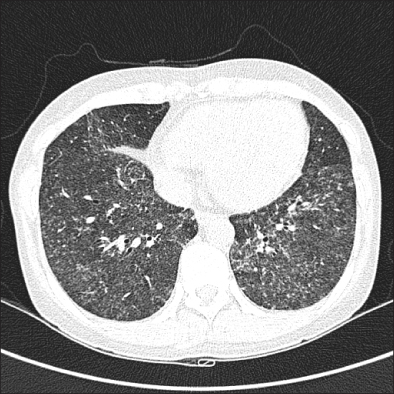
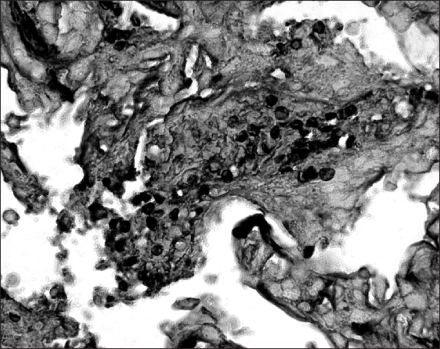
- Bilateral interstitial infiltration in chest radiography, which may be fine granular, reticular or of ground glass opacity, is the typical radiographic findings of Pneumocystis jiroveci pneumonia. Recently, atypical radiographic features, including cystic lung disease, spontaneous pneumothorax or nodular opacity, have been reported intermittently in patients with P. jiroveci pneumonia. We report the case of a 29-year-old woman with a transplanted kidney whose simple chest radiography and HRCT scan showed numerous miliary nodules in both lungs, mimicking miliary tuberculosis (TB). Under the presumptive diagnosis of miliary TB, empirical anti-TB medication was started. However, Grocott methenamine silver nitrate staining of a transbronchial lung biopsy tissue revealed P. jiroveci infection without evidence of TB. These findings suggest that even in TB-endemic area other etiology such as P. jiroveci as well as M. tuberculosis should be considered as an etiology of miliary lung nodules in immunocompromised patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Bartlett JG. Pneumonia in the patient with HIV infection. Infect Dis Clin North Am. 1998. 12:807–820.2. McGuinness G, Gruden JF. Viral and Pneumocystis carinii infections of the lung in the immunocompromised host. J Thorac Imaging. 1999. 14:25–36.3. Flannery MT, Quiroz E, Grundy LS, Brantley S. Pneumocystis carinii pneumonia with an atypical granulomatous response. South Med J. 1996. 89:409–410.4. Ong EL, Murray H, Ellis ME. Miliary Pneumocystis carinii pneumonia in acquired immunodeficiency syndrome. Int J STD AIDS. 1992. 3:54–55.5. Kennedy CA, Goetz MB. Atypical roentgenographic manifestations of Pneumocystis carinii pneumonia. Arch Intern Med. 1992. 152:1390–1398.6. Hazzan M, Copin MC, Pruvot FR, Codaccioni MX, Dracon M, Lelievre G, et al. Lung granulomatous pneumocystosis after kidney transplantation: an uncommon complication. Transplant Proc. 1997. 29:2409.7. Leroy X, Copin MC, Ramon P, Jouet JP, Gosselin B. Nodular granulomatous Pneumocystis carinii pneumonia in a bone marrow transplant recipient: case report. APMIS. 2000. 108:363–366.8. Cohen WN, McAlister WH. Pneumocystis carinii pneumonia: report of four cases. Am J Roentgenol Radium Ther Nucl Med. 1963. 89:1032–1037.9. Lee JY, Lee KS, Jung KJ, Han J, Kwon OJ, Kim J, et al. Pulmonary tuberculosis: CT and pathologic correlation. J Comput Assist Tomogr. 2000. 24:691–698.10. Kroe DM, Kirsch CM, Jensen WA. Diagnostic strategies for Pneumocystis carinii pneumonia. Semin Respir Infect. 1997. 12:70–78.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chest x-ray findings of opportunistic infections
- A Case of Successfully Treated Pneumocystis jiroveci Pneumonia in CMV-associated IgA Nephropathy
- Hypoglycemic Seizures Associated with Pentamidine for Pneumocystis jiroveci Pneumonia in a HIV Patient
- Pneumocystis jiroveci Pneumonia in a 5-month-old Boy with Agammaglobulinemia: A Case Report
- CT Findings of Granulomatous Pneumocystis jiroveci Pneumonia in a Patient with Multiple Myeloma