Tuberc Respir Dis.
2009 Feb;66(2):98-103.
Clinical Features of Pulmonary Langerhans Cell Histiocytosis in Korea
- Affiliations
-
- 1Department of Internal Medicine, Gachon University Gil Medical Center, Incheon, Korea.
- 2Department of Internal Medicine, Guro Hospital, Korea University Medical Center, Seoul, Korea.
- 3Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea.
- 4Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea.
- 5Department of Internal Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 7Department of Internal Medicine, Soonchunhyang University College of Medicine, Seoul, Korea. uhs@hosp.sch.ac.kr
- 8Department of Internal Medicine, Soonchunhyang University College of Medicine, Bucheon, Korea.
- 9Department of Internal Medicine, Asan Medical Center, Seoul, Korea.
- 10Department of Internal Medicine, Ulsan University College of Medicine, Ulsan, Korea.
- 11Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 12Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul, Korea.
- 13Department of Internal Medicine, College of Medicine, Inje University, Busan, Korea.
- 14Department of Internal Medicine, College of Medicine, Inha University, Incheon, Korea.
- 15Department of Internal Medicine, College of Medicine, Hallym University, Seoul, Korea.
Abstract
- BACKGROUND
Pulmonary Langerhans cell histiocytosis (PLCH) is characterized by a proliferation of Langerhans cells and this results in granulomas that involve multiple organs of the body. Because the incidence of PLCH is very low in Korea and worldwide, collecting the clinical data of patients with PLCH nationwide is needed to determine the clinical features of Korean patients with PLCH.
METHODS
The patients with PLCH confirmed by biopsy at any body site were included and the patients should have lung lesions present. A questionnaire that had items on the symptoms, lung function tests, the roentgenographic findings and the treatment was collected retrospectively at a Korean ILD Research Meeting.
RESULTS
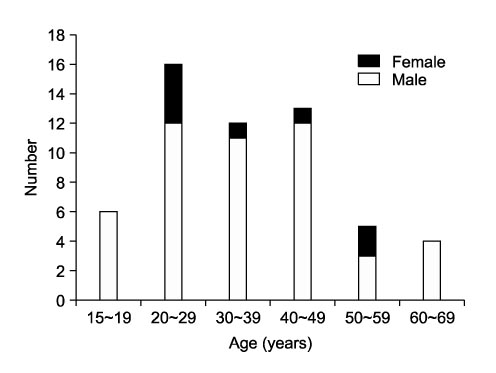
A total of 56 cases were collected. The number of males and females was 48 and 8, respectively, and their median age was 43 years (range: 18~67 years). The patients were current or ex-smokers in 79% of the cases. The most frequent symptom was coughing (39%), followed in decreasing order by dyspnea (38%), sputum (20%) and chest pain (20%). Pneumothorax was observed in 16 (29%) patients. Lung function tests showed a normal, restrictive, mixed or obstructive pattern in 26 (61%), 7 (16%), 7 (16%) and 3 patients (7%), respectively. Nodular-cystic lesion was most frequently observed in 59% of the patients on HRCT. The lung lesions were located in the middle and upper lobes in almost the cases. The median follow-up period was 90 months (range: 1~180 months) and only two patients died during this period.
CONCLUSION
This study provides a national survey of the patients with PLCH during a long follow-up period.
MeSH Terms
Figure
Reference
-
1. Tazi A. Adult pulmonary Langerhans' cell histiocytosis. Eur Respir J. 2006. 27:1272–1285.2. Gaensler EA, Carrington CB. Open biopsy for chronic diffuse infiltrative lung disease: clinical, roentgenographic, and physiological correlations in 502 patients. Ann Thorac Surg. 1980. 30:411–426.3. Kim YM, Park YI, Choi YK, Lee JS, Lee WC, Hong JH, et al. A case of primary pulmonary histiocytosis-X associated with central diabetes insipidus. Tuberc Respir Dis. 1999. 46:110–115.4. Hong SJ, Ahn KH, Lee WY, Kong SJ, Yong SJ, Shin KC. A case of pulmonary histiocytosis-X associated with bilateral, recurrent, and spontaneous pneumo thorax. Tuberc Respir Dis. 1994. 41:152–157.5. Hwang YI, Park GM, Yim JJ, Yoo CG, Lee CT, Kim YW, et al. Clinical characteristics of pulmonary histiocytosis X. Tuberc Respir Dis. 2001. 51:346–353.6. Howarth DM, Gilchrist GS, Mullan BP, Wiseman GA, Edmonson JH, Schomberg PJ. Langerhans cell histiocytosis: diagnosis, natural history, management, and outcome. Cancer. 1999. 85:2278–2290.7. Travis WD, Borok Z, Roum JH, Zhang J, Feuerstein I, Ferrans VJ, et al. Pulmonary Langerhans cell granulomatosis (histiocytosis X). A clinicopathologic study of 48 cases. Am J Surg Pathol. 1993. 17:971–986.8. Zeid NA, Muller HK. Tobacco smoke induced lung granulomas and tumors: association with pulmonary Langerhans cells. Pathology. 1995. 27:247–254.9. Youkeles LH, Grizzanti JN, Liao Z, Chang CJ, Rosenstreich DL. Decreased tobacco-glycoprotein-induced lymphocyte proliferation in vitro in pulmonary eosinophilic granuloma. Am J Respir Crit Care Med. 1995. 151:145–150.10. Boehler A. Lung transplantation for cystic lung diseases: lymphangioleiomyomatosis, histiocytosis X, and sarcoidosis. Semin Respir Crit Care Med. 2001. 22:509–516.11. Sulica R, Teirstein A, Padilla ML. Lung transplantation in interstitial lung disease. Curr Opin Pulm Med. 2001. 7:314–322.12. Etienne B, Bertocchi M, Gamondes JP, Thevenet F, Boudard C, Wiesendanger T, et al. Relapsing pulmonary Langerhans cell histiocytosis after lung transplan tation. Am J Respir Crit Care Med. 1998. 157:288–291.13. Gabbay E, Dark JH, Ashcroft T, Milne D, Gibson GJ, Healy M, et al. Recurrence of Langerhans' cell granulomatosis following lung transplantation. Thorax. 1998. 53:326–327.14. Habib SB, Congleton J, Carr D, Partridge J, Corrin B, Geddes DM, et al. Recurrence of recipient Langerhans' cell histiocytosis following bilateral lung transplanta tion. Thorax. 1998. 53:323–325.15. Basset F, Corrin B, Spencer H, Lacronique J, Roth C, Soler P, et al. Pulmonary histiocytosis X. Am Rev Respir Dis. 1978. 118:811–820.16. Vassallo R, Ryu JH, Schroeder DR, Decker PA, Limper AH. Clinical outcomes of pulmonary Langerhans'-cell histiocytosis in adults. N Engl J Med. 2002. 346:484–490.17. Watanabe R, Tatsumi K, Hashimoto S, Tamakoshi A, Kuriyama T. Clinico-epidemiological features of pulmonary histiocytosis X. Intern Med. 2001. 40:998–1003.18. Colby TV, Lombard C. Histiocytosis X in the lung. Hum Pathol. 1983. 14:847–856.19. Crausman RS, Jennings CA, Tuder RM, Ackerson LM, Irvin CG, King TE Jr. Pulmonary histiocytosis X: pulmonary function and exercise pathophysiology. Am J Respir Crit Care Med. 1996. 153:426–435.20. Delobbe A, Durieu J, Duhamel A, Wallaert B. Determinants of survival in pulmonary Langerhans' cell granulomatosis (histiocytosis X). Groupe d'Etude en Pathologie Interstitielle de la Société de Pathologie Thoracique du Nord. Eur Respir J. 1996. 9:2002–2006.21. Friedman PJ, Liebow AA, Sokoloff J. Eosinophilic granuloma of lung. Clinical aspects of primary histiocytosis in the adult. Medicine (Baltimore). 1981. 60:385–396.22. Schonfeld N, Frank W, Wenig S, Uhrmeister P, Allica E, Preussler H, et al. Clinical and radiologic features, lung function and therapeutic results in pulmonary histiocytosis X. Respiration. 1993. 60:38–44.23. Minghini A, Trogdon SD. Recurrent spontaneous pneumothorax in pulmonary histiocytosis X. Am Surg. 1998. 64:1040–1042.24. Mendez JL, Nadrous HF, Vassallo R, Decker PA, Ryu JH. Pneumothorax in pulmonary Langerhans cell histiocytosis. Chest. 2004. 125:1028–1032.25. Tazi A, Soler P, Hance AJ. Adult pulmonary Lan gerhans' cell histiocytosis. Thorax. 2000. 55:405–416.26. Vassallo R, Ryu JH, Colby TV, Hartman T, Limper AH. Pulmonary Langerhans'-cell histiocytosis. N Engl J Med. 2000. 342:1969–1978.27. Moore AD, Godwin JD, Muller NL, Naidich DP, Hammar SP, Buschman DL, et al. Pulmonary histiocytosis X: comparison of radiographic and CT findings. Radiology. 1989. 172:249–254.28. Lacronique J, Roth C, Battesti JP, Basset F, Chretien J. Chest radiological features of pulmonary histiocytosis X: a report based on 50 adult cases. Thorax. 1982. 37:104–109.29. Sundar KM, Gosselin MV, Chung HL, Cahill BC. Pulmonary Langerhans cell histiocytosis: emerging concepts in pathobiology, radiology, and clinical evolution of disease. Chest. 2003. 123:1673–1683.30. Von Essen S, West W, Sitorius M, Rennard SI. Complete resolution of roentgenographic changes in a patient with pulmonary histiocytosis X. Chest. 1990. 98:765–767.31. Mogulkoc N, Veral A, Bishop PW, Bayindir U, Pickering CA, Egan JJ. Pulmonary Langerhans' cell histiocytosis: radiologic resolution following smoking cessation. Chest. 1999. 115:1452–1455.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Langerhans Cell Histiocytosis Accompanied by Active Pulmonary Tuberculosis
- A Case of Pulmonary Langerhans Cell Histiocytosis with Pneumothorax
- Spontaneous Pneumothorax due to Pulmonary Invasion in Multisystemic Langerhans Cell Histiocytosis: A case report
- Radiologic manifestation of pulmonary Langerhans' cell histiocytosis
- A Case of Orbital Langerhans' cell histiocytosis