Tuberc Respir Dis.
2008 Jun;64(6):460-465.
Two Cases of Pulmonary Thromboembolism in Young Patients with Hyperhomocysteinemia
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. kyh30med@catholic.ac.kr
Abstract
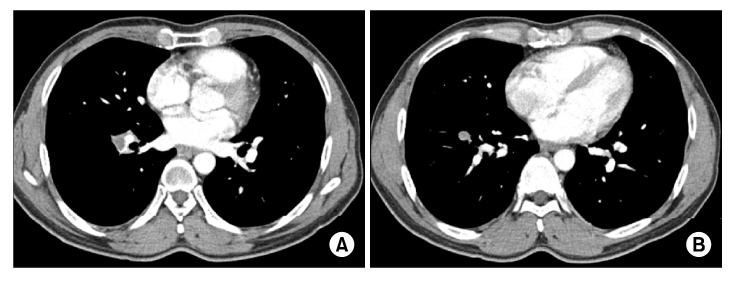
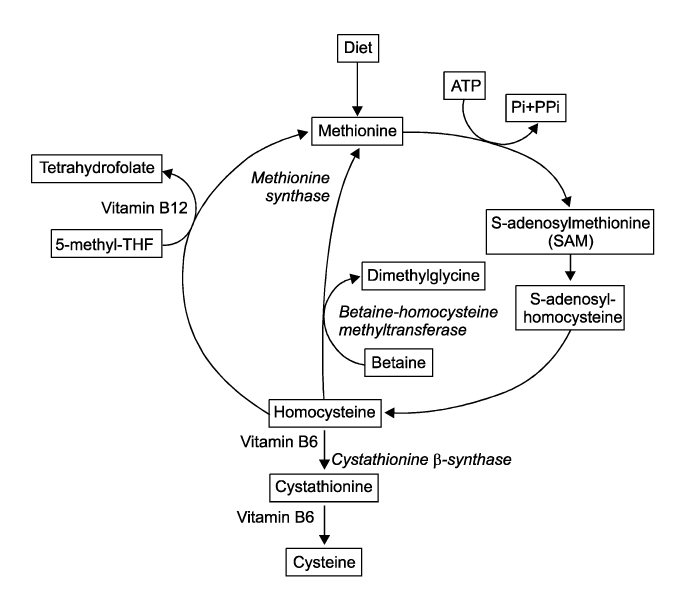
- Incidences of pulmonary thromboembolism markedly increase with age. Risk factors of pulmonary thromboembolism are surgery, trauma, acute medical illness, immobilization, pregnancy, usage of hormone, and advanced age. In the cases of thrombomembolism occurred in young age, the possibility of thrombophilc state is needed to be investigated. Among many diseases or state associated thrombophilic state, homocyteinemia should be considered a cause of thromboembolism before fifth decade. Homocyteinemia is caused by deficiency of N-5-methyltetrahydrofolate, cystathionie beta-synthase and vitamin B12. The presence of the mutation of 5,10-methyleneterahydrofolate lead to homocyteinemia by deficiency of N-5-methyltetrahydrofolate. Homocysteine is acknowledged the risk factor of cardiovascular event, and storke. Homocysteinemia can be the cause of thromboemboism via damaging endotheial cell. We present two cases of pulmonary thromboembolism in young age which seem to be associated with homocysteinemia precipitated by mutation of 5,10-methyleneterahydrofolate.
MeSH Terms
Figure
Reference
-
1. Kim V, Spandorfer J. Epidemiology of venous thromboembolic disease. Emerg Med Clin North Am. 2001. 19:839–859.2. The British Committee for Standards in Haematology. Guidelines on the investigation and management of thrombophilia. J Clin Pathol. 1990. 43:703–709.3. Tapson VF. Acute pulmonary embolism. N Engl J Med. 2008. 358:1037–1052.4. Maron BA, Loscalzo J. Homocysteine. Clin Lab Med. 2006. 26:591–609. vi.5. Selhub J. Homocysteine metabolism. Annu Rev Nutr. 1999. 19:217–246.6. Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet. 1995. 10:111–113.7. Silverstein MD, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ 3rd. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998. 158:585–593.8. den Heijer M, Koster T, Blom HJ, Bos GM, Briet E, Reitsma PH, et al. Hyperhomocysteinemia as a risk factor for deep-vein thrombosis. N Engl J Med. 1996. 334:759–762.9. Cushman M. Epidemiology and risk factors for venous thrombosis. Semin Hematol. 2007. 44:62–69.10. Oh SE, Jung JH, Yoon SB, Yoon HY, Park JK, Lee DH, et al. A case of pulmonary thromboembolism in a patient with hyperhomocysteinemia. Tuberc Respir Dis. 2007. 62:211–216.11. Weiss N, Keller C, Hoffmann U, Loscalzo . Endothelial dysfunction and atherothrombosis in mild hyperhomocysteinemia. Vasc Med. 2002. 7:227–239.12. Ray JG, Kearon C, Yi Q, Sheridan P, Lonn E. Homocysteine-lowering therapy and risk for venous thromboembolism: a randomized trial. Ann Intern Med. 2007. 146:761–767.13. Toole JF, Malinow MR, Chambless LE, Spence JD, Pettigrew LC, Howard VJ, et al. Lowering homocysteine in patients with ischemic stroke to prevent recurrent stroke, myocardial infarction, and death: the Vitamin Intervention for Stroke Prevention (VISP) randomized controlled trial. JAMA. 2004. 291:565–575.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pulmonary Thromboembolism in a Patient with Hyperhomocysteinemia
- Recurrent Stent Thrombosis and Pulmonary Thromboembolism Associated with Hyperhomocysteinemia
- A Case of Multiple Thromboembolisms in Hyperhomocysteinemia
- A Case of Hyperhomocysteinemia Manifested by Deep Vein Thrombosis and Pulmonary Embolism
- Pulmonary thromboembolism due to severe hyperhomocysteinemia associated with a methyltetrahydrofolate reductase mutation