J Lipid Atheroscler.
2012 Dec;1(2):95-100. 10.12997/jla.2012.1.2.95.
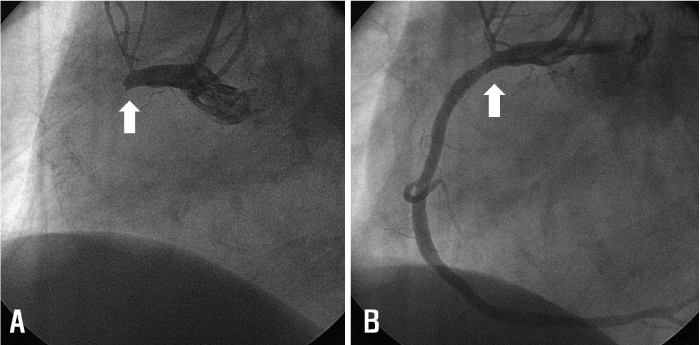
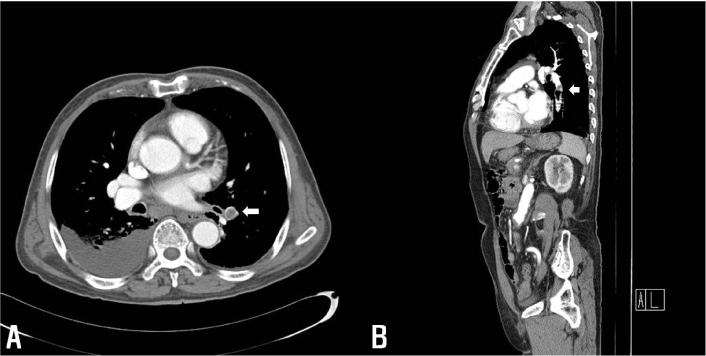
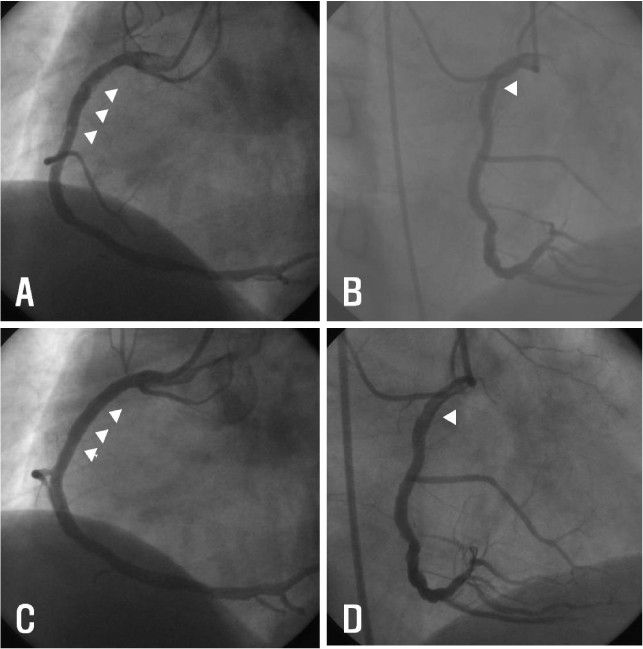
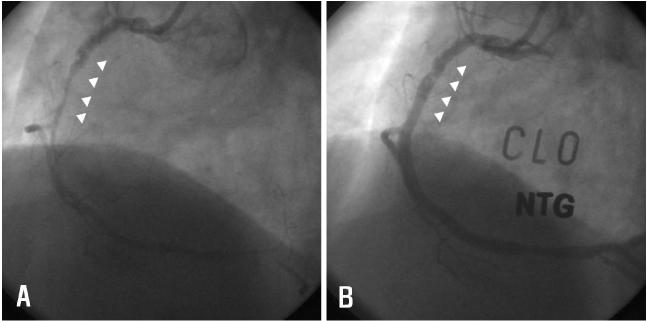
Recurrent Stent Thrombosis and Pulmonary Thromboembolism Associated with Hyperhomocysteinemia
- Affiliations
-
- 1The Heart Center of Chonnam National University Hospital, Gwangju, Korea. myungho@chollian.net
- KMID: 2198367
- DOI: http://doi.org/10.12997/jla.2012.1.2.95
Abstract
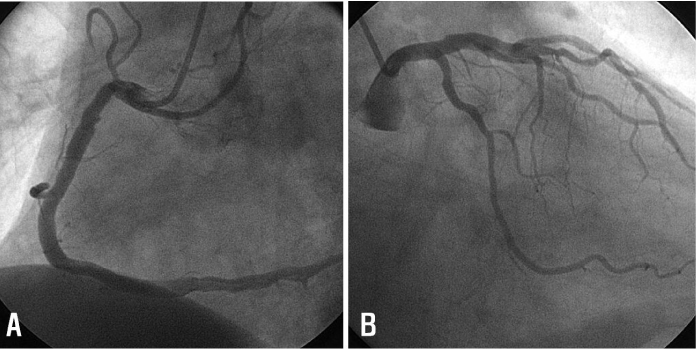
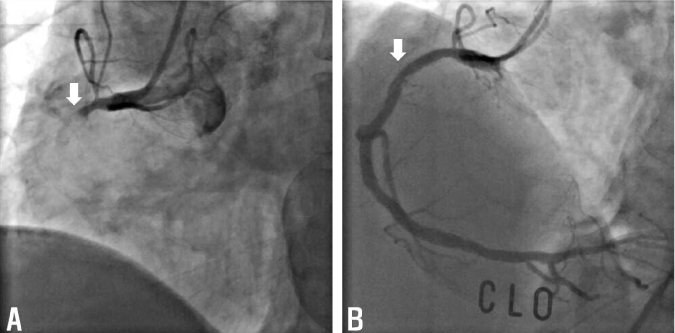
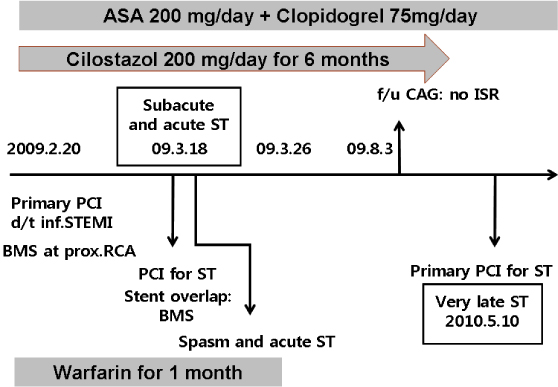
- Stent thrombosis is a fatal complication that can cause sudden cardiac death in patients implanted coronary stent. Also, pulmonary thromboembolism is associated with increased mortality. Usually, these vascular thromboembolic diseases did not occured simultaneously. If this circumstance develops, possible mechanisms and causes should be described. Here, we report a case of patient underwent percutaneous coronary intervention under diagnosis of ST-segment elevation myocardial infarction with recurrent stent thrombosis and pulmonary thromboembolism associated with hyperhomocysteinemia despite optimal medical therapy.
MeSH Terms
Figure
Reference
-
1. Cutlip DE, Baim DS, Ho KK, et al. Stent thrombosis in the modern era: a pooled analysis of multicenter coronary stent clinical trials. Circulation. 2001; 103:1967–1971.2. Konstantinides S. Clinical practice. Acute pulmonary embolism. N Engl J Med. 2008; 359:2804–2813.3. Park DW, Park SW. Stent thrombosis in the era of the drug-eluting stent. Korean Circ J. 2005; 35:791–794.
Article4. Jensen LO, Maeng M, Kaltoft A, et al. Stent thrombosis, myocardial infarction, and death after drug-eluting and bare-metal stent coronary interventions. J Am Coll Cardiol. 2007; 50:463–470.
Article5. Celik T, Iyisoy A, Celik M, Isik E. A case of very late stent thrombosis after bare metal coronary stent implantation: a neglected complication. Int J Cardiol. 2009; 134:111–113.
Article6. Lentz SR. Mechanisms of homocysteine-induced atherothrombosis. J Thromb Haemost. 2005; 3:1646–1654.
Article7. Den Heijer M, Lewington S, Clarke R. Homocysteine, MTHFR and risk of venous thrombosis: a meta-analysis of published epidemiological studies. J Thromb Haemost. 2005; 3:292–299.
Article8. Grifoni E, Marcucci R, Giutu G, et al. The thrombophilic pattern of different clinical manifestations of venous thromboembolism: a survey of 443 cases of venous thromboembolism. Semin thromb Hemost. 2012; 38:230–234.
Article9. Karalezli A, Parlak ES, Kanbay A, Senturk A, Hassanoglu HC. Homocysteine and serum-lipid levels in pulmonary embolism. Clin Appl Thromb Hemost. 2011; 17:E186–E189.
Article10. Holmes DR Jr, Kereiakes DJ, Kleiman NS, Moliterno DJ, Patti G, Crines CL. Combining antiplatelet and anticoagulant therapies. J Am Coll Cardiol. 2009; 54:95–109.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- lilac Vein Thrombosis: A Case Report of Treatment with Inferior Vena Cava Filter, Urokinase and Vascular Stent
- A Case of Pulmonary Thromboembolism in a Patient with Hyperhomocysteinemia
- A Case of Hyperhomocysteinemia Manifested by Deep Vein Thrombosis and Pulmonary Embolism
- Pulmonary Embolism Caused by Popliteal Venous Aneurysm
- Clinical Year in Review of Venous Thromboembolism