Korean J Hematol.
2006 Jun;41(2):110-114. 10.5045/kjh.2006.41.2.110.
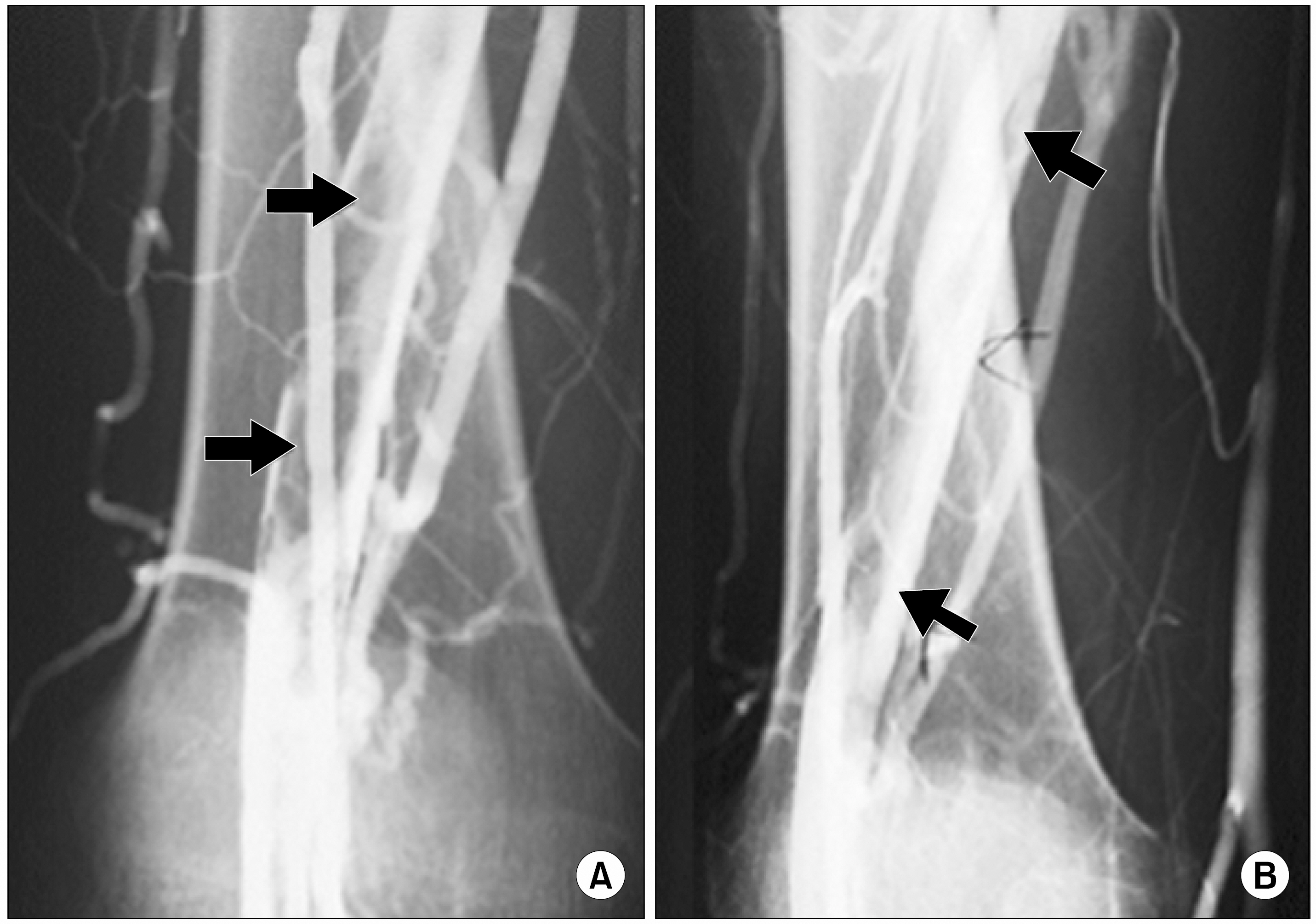
A Case of Hyperhomocysteinemia Manifested by Deep Vein Thrombosis and Pulmonary Embolism
- Affiliations
-
- 1Department of Internal Medicine, National Medical Center, Seoul, Korea. sbjookr@nate.com
- KMID: 2083485
- DOI: http://doi.org/10.5045/kjh.2006.41.2.110
Abstract
- Homocysteine has been reported as an independent risk factor of intravascular thrombosis and atherosclerosis by its participation in vascular endothelial cell dysfunction, platelet activation and thrombus formation. The serum homocysteine concentration is influenced by not only heredity, but also by environmental factors, and it interacts with the former reported risk factors of atherosclerosis. We report here on a case of a young patient with hyperhomocysteinemia that manifested by deep vein thrombosis and pulmonary embolism.
MeSH Terms
Figure
Reference
-
1). Welch GN., Loscalzo J. Homocysteine and athero-thrombosis. N Engl J Med. 1998. 338:1042–50.
Article2). Refsum H., Ueland PM. Recent data are not in conflict with homocysteine as a cardiovascular risk factor. Curr Opin Lipidol. 1998. 9:533–9.
Article3). Adcock DM., Fink L., Marlar RA. A laboratory approach to the evaluation of hereditary hypercoagulability. Am J Clin Pathol. 1997. 108:434–49.
Article4). McCully KS., Wilson RB. Homocysteine theory of atherosclerosis. Atherosclerosis. 1975. 22:215–27.5). den Heijer M., Koster T., Blom HJ, et al. Hyperhomocysteinemia as a risk factor for deep-vein thrombosis. N Engl J Med. 1996. 334:759–62.
Article6). Key NS., McGlennen RC. Hyperhomocysteinemia and thrombophilia. Arch Pathol Lab Med. 2002. 126:1367–75.
Article7). Langman LJ., Ray JG., Evrovski J., Yeo E., Cole DE. Hyperhomocysteinemia and the increased risk of venous thromboembolism: more evidence from a case-control study. Arch Intern Med. 2000. 160:961–4.8). Tsai JC., Perrella MA., Yoshizumi M, et al. Promotion of vascular smooth muscle cell growth by homocysteine: a link to atherosclerosis. Proc Natl Acad Sci USA. 1994. 91:6369–73.
Article9). Ou T., Yamakawa-Kobayashi K., Arinami T, et al. Methylenetetrahydrofolate reductase and apolipoprotein E polymorphims are independent risk factors for coronary heart disease in Japanese: a case-control study. Atherosclerosis. 1998. 137:23–8.10). Gardemann A., Weidemann H., Philipp M, et al. The TT genotype of the methylenetetrahydrofolate reductase C677T gene polymorphism is associated with the extent of coronary atherosclerosis in patients at high risk for coronary artery disease. Eur Heart J. 1999. 20:584–92.
Article11). Refsum H., Ueland PM., Nygard O., Vollset SE. Homocysteine and cardiovascular disease. Annu Rev Med. 1998. 49:31–62.
Article12). Kasper DL., Braunwald E., Fauci AS., Hauser SL., Longo DL., Jameson JL. Harrison's principles of internal medicine. 16th ed.New York: McGraw-Hill;2005. 2334.13). Kuch B., Bobak M., Fobker M, et al. Associations between homocysteine and coagulation factors—a cross-sectional study in two populations of central Europe. Thromb Res. 2001. 103:265–73.14). Brattstrom LE., Israelsson B., Jeppsson JO., Hultberg BL. Folic acid—an innocuous means to reduce plasma homocysteine. Scand J Clin Lab Invest. 1988. 48:215–21.15). Brouwer IA., van Dusseldorp M., Thomas CM, et al. Low-dose folic acid supplementation decreases plasma homocysteine concentrations: a randomized trial. Am J Clin Nutr. 1999. 69:99–104.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Hereditary Antithrombin III Deficiency Manifested by Myocardial Infarction and Deep Vein Thrombosis
- A Case of Upper Extremity Deep Vein Thrombosis and Pulmonary Thromboembolism in a Severely Obese Man
- An Acute Pulmonary Embolism Accompanying Greater Saphenous Vein Thrombosis
- A Case of Deep Vein Thrombosis Associated with Pulmonary and Renal Thromboembolism
- A Case of Antiphospholipid Syndrome Refractory to Secondary Anticoagulating Prophylaxis after Deep Vein Thrombosis-Pulmonary Embolism