Tuberc Respir Dis.
2006 May;60(5):564-570.
A Case of Cavitary Lung Lesion as a Consequence of Smoke Inhalation Injury
- Affiliations
-
- 1Department of Internal Medicine, Hallym University College of Medicine, Seoul, Korea. ighyun@hallym.ac.kr
- 2Department of Radiology, Hallym University College of Medicine, Seoul, Korea.
Abstract
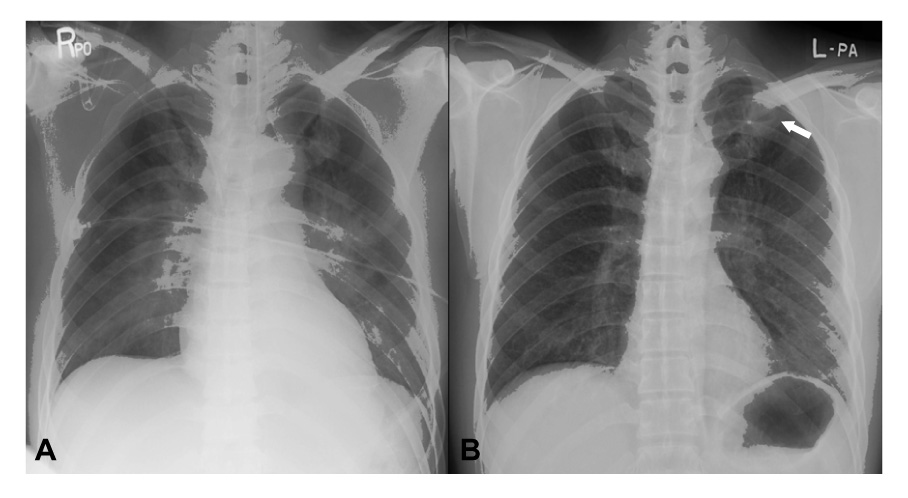
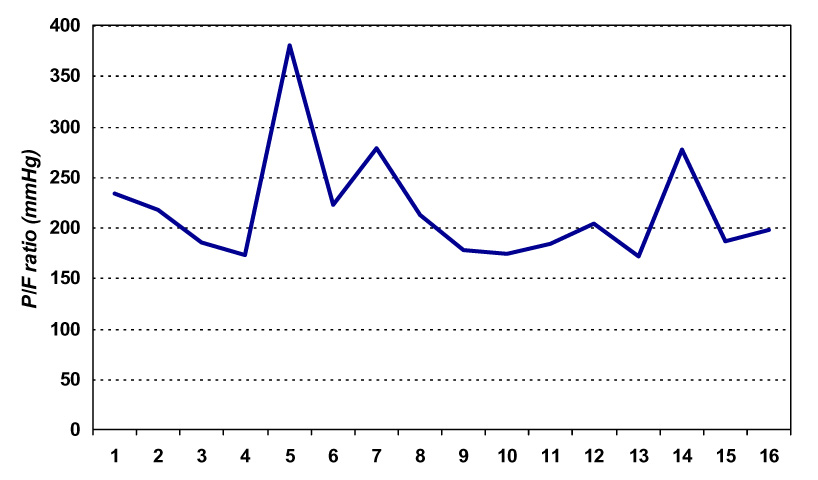
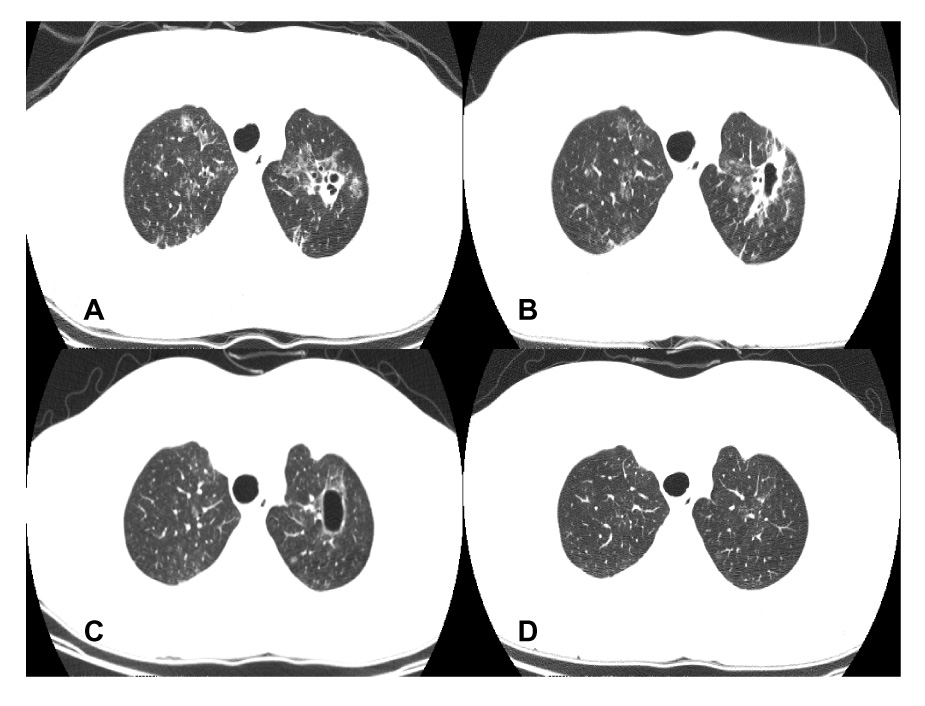
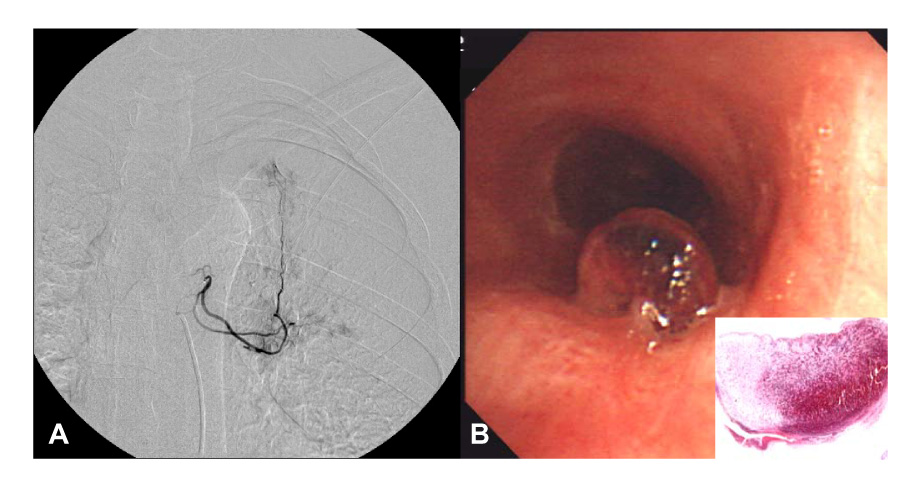
- Toxic gases and soot deposition as a consequence of smoke inhalation can cause direct injury to the upper and lower airways and even to the lung parenchyma. A delay in proper and prompt therapy can be detrimental to critically ill burn patients with an inhalation injury. Therefore, serial chest radiography is an important diagnostic tool for pulmonary complications during treatment. The radiographic findings of the chest include normal, consolidation, interstitial and alveolar infiltrates, peribronchial thickening, atelectasis, cardiogenic and non-cardiogenic pulmonary edema, and a pneumothorax as acute complications of smoke inhalation. In addition, bronchiectasis, bronchiolitis obliterans and pulmonary fibrosis can occur as late complications. We encountered a case of 44-year-old male who presented with acute lung injury after an inhalation injury. He required endotracheal intubation and mechanical ventilation due to respiratory failure. He was managed successfully with conservative treatment. Later, a cavitary lesion of the left upper lobe was observed on the chest radiography and computed tomography, which was complicated by massive hemoptysis during the follow-up. However, the cavitary lesion disappeared spontaneously without any clinical consequences.
Keyword
MeSH Terms
-
Acute Lung Injury
Adult
Bronchiectasis
Bronchiolitis Obliterans
Burns
Critical Illness
Follow-Up Studies
Gases
Hemoptysis
Humans
Inhalation
Intubation, Intratracheal
Lung*
Male
Pneumothorax
Pulmonary Atelectasis
Pulmonary Edema
Pulmonary Fibrosis
Radiography
Respiration, Artificial
Respiratory Insufficiency
Smoke Inhalation Injury*
Smoke*
Soot
Thorax
Gases
Smoke
Soot
Figure
Reference
-
1. Herndon DN, Gore D, Cole M, Desai MH, Linares H, Abston S, et al. Determinants of mortality in pediatric patients with greater than 70% full-thickness total body surface area thermal injury treated by early total excision and grafting. J Trauma. 1987. 27:208–212.2. Saffle JR, Davis B, Williams P. Recent outcomes in the treatment of burn injury in the United States: a report from the American Burn Association Patient Registry. J Burn Care Rehabil. 1995. 16:219–232.3. Shirani KZ, Pruitt BA Jr, Mason AD Jr. The influence of inhalation injury and pneumonia on burn mortality. Ann Surg. 1987. 205:82–87.4. Moylan JA Jr, Wilmore DW, Mouton DE, Pruitt BA Jr. Early diagnosis of inhalation injury using 133 xenon lung scan. Ann Surg. 1972. 176:477–484.5. Putman CE, Loke J, Matthay RA, Ravin CE. Radiographic manifestations of acute smoke inhalation. AJR Am J Roentgenol. 1977. 129:865–870.6. Aberle DR, Brown K. Radiologic considerations in the adult respiratory distress syndrome. Clin Chest Med. 1990. 11:737–754.7. George A, Gupta R, Bang RL, Ebrahim MK. Radiological manifestation of pulmonary complications in deceased intensive care burn patients. Burns. 2003. 29:73–78.8. Lee MJ, O'Connell DJ. The plain chest radiograph after acute smoke inhalation. Clin Radiol. 1988. 39:33–37.9. Teixidor HS, Novick G, Rubin E. Pulmonary complications in burn patients. J Can Assoc Radiol. 1983. 34:264–270.10. Wittram C, Kenny JB. The admission chest radiograph after acute inhalation injury and burns. Br J Radiol. 1994. 67:751–754.11. Slutzker AD, Kinn R, Said SI. Bronchiectasis and progressive respiratory failure following smoke inhalation. Chest. 1989. 95:1349–1350.12. Tasaka S, Kanazawa M, Mori M, Fujishima S, Ishizaka A, Yamasawa F, et al. Long-term course of bronchiectasis and bronchiolitis obliterans as late complication of smoke inhalation. Respiration. 1995. 62:40–42.13. Chrysopoulo MT, Barrow RE, Muller M, Rubin S, Barrow LN, Herndon DN. Chest radiographic appearances in severely burned adults: a comparison of early radiographic and extravascular lung thermal volume changes. J Burn Care Rehabil. 2001. 22:104–110.14. Lee SH, Lee ES, Kim SH, Park JY, Kim SH, Hong SH, et al. Plain chest radiographic findings of smoke inhalation. J Korean Radiol Soc. 2000. 42:933–937.15. George A, Bang RL, Gupta R, Khalaf EM. Minor burns and pneumatocoeles: a case report. Burns. 2001. 27:504–508.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Plain Chest Radiographic Findings of Smoke Inhalation
- Tracheobronchial Polyps Following Thermal Inhalation Injury
- A case of lung injury caused by ammonia-gas inhalation
- A Case of Cavitary Pulmonary Metastases of Primary Cavitary Lung Cancer
- Roentgenogram of the Issue : Huge abscess Cavity in right lower lung