Korean J Urol.
2011 Dec;52(12):809-814.
Prostate-Specific Antigen Density as a Powerful Predictor of Extracapsular Extension and Positive Surgical Margin in Radical Prostatectomy Patients with Prostate-Specific Antigen Levels of Less than 10 ng/ml
- Affiliations
-
- 1Department of Urology, Konyang Universtiy College of Medicine, Daejeon, Korea. doc71377@hanmail.net
- 2Department of Urology, Korea University School of Medicine, Seoul, Korea.
Abstract
- PURPOSE
To assess the ability of preoperative variables to predict extracapsular extension (ECE) and positive surgical margin (PSM) in radical prostatectomy patients with prostate-specific antigen (PSA) levels of less than 10 ng/ml.
MATERIALS AND METHODS
From January 2008 to December 2009, 121 patients with prostate cancer with PSA levels lower than 10 ng/ml who underwent radical prostatectomy were enrolled in the study. The differences in clinical factors (age, PSA, PSA density [PSAD], digital rectal examination [DRE] positivity, positive magnetic resonance imaging [MRI], Gleason sum, positive core number, and positive biopsy core percentage) with ECE and the presence of positive margins were determined and their independent predictive significances were analyzed.
RESULTS
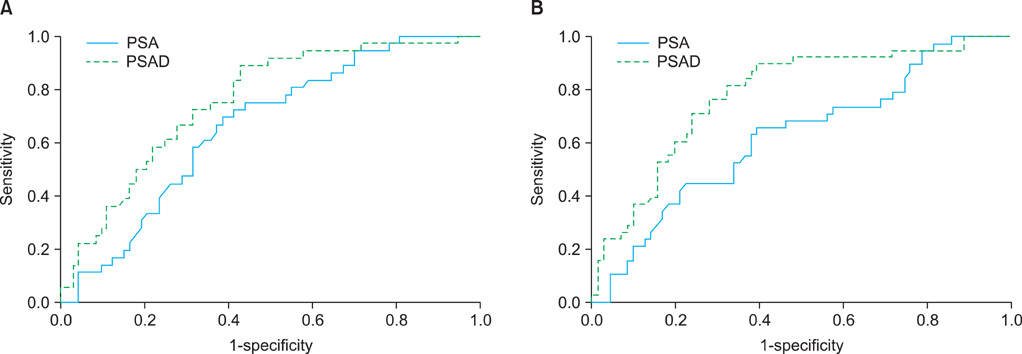
The ECE-positive patients had higher PSA, PSAD, and MRI-positive percentages, and PSM patients had higher PSA, PSAD, MRI-positive percentages, Gleason sum, and positive biopsy core percentages for prostate cancer. In the multivariate analysis, PSAD and MRI positivity were the best independent predictors for ECE, and PSA and PSAD were the best independent predictors of PSM. By receiver operating characteristic curve analysis, PSAD had better discriminative area under the curve value than did PSA for ECE (0.765 vs 0.661) and PSM (0.780 vs 0.624). The best predictive PSAD value was 0.29 ng/ml/cc for ECE and 0.27 ng/ml/cc for PSM.
CONCLUSIONS
PSAD has relevance to ECE (plus MRI findings) and PSM (plus PSA). PSAD might be a powerful predictor of ECE and PSM preoperatively in patients undergoing a radical prostatectomy with PSA levels of less than 10 ng/ml.
MeSH Terms
Figure
Reference
-
1. Hara I, Miyake H, Hara S, Yamanaka N, Ono Y, Eto H, et al. Value of the serum prostate-specific antigen-alpha 1-antichymotrypsin complex and its density as a predictor for the extent of prostate cancer. BJU Int. 2001. 88:53–57.2. Smith JA Jr, Scardino PT, Resnick MI, Hernandez AD, Rose SC, Egger MJ. Transrectal ultrasound versus digital rectal examination for the staging of carcinoma of the prostate: results of a prospective, multi-institutional trial. J Urol. 1997. 157:902–906.3. Zheng XY, Xie LP, Wang YY, Ding W, Yang K, Shen HF, et al. The use of prostate specific antigen (PSA) density in detecting prostate cancer in Chinese men with PSA levels of 4-10 ng/mL. J Cancer Res Clin Oncol. 2008. 134:1207–1210.4. Rietbergen JB, Hoedemaeker RF, Kruger AE, Kirkel WJ, Schröder FH. The changing pattern of prostate cancer at the time of diagnosis: characteristics of screen detected prostate cancer in a population based screening study. J Urol. 1999. 161:1192–1198.5. Shinohara K, Wolf JS Jr, Narayan P, Carroll PR. Comparison of prostate specific antigen with prostate specific antigen density for 3 clinical applications. J Urol. 1994. 152:120–123.6. Partin AW, Carter HB, Chan DW, Epstein JI, Oesterling JE, Rock RC, et al. Prostate specific antigen in the staging of localized prostate cancer: influence of tumor differentiation, tumor volume and benign hyperplasia. J Urol. 1990. 143:747–752.7. Graefen M, Haese A, Pichlmeier U, Hammerer PG, Noldus J, Butz K, et al. A validated strategy for side specific prediction of organ confined prostate cancer: a tool to select for nerve sparing radical prostatectomy. J Urol. 2001. 165:857–863.8. Ohori M, Kattan MW, Koh H, Maru N, Slawin KM, Shariat S, et al. Predicting the presence and side of extracapsular extension: a nomogram for staging prostate cancer. J Urol. 2004. 171:1844–1849.9. Choi H, Ko YH, Kang SG, Kang SH, Park HS, Cheon J, et al. Biopsy related prostate status does not affect on the clinicopathological outcome of robotic assisted laparoscopic radical prostatectomy. Cancer Res Treat. 2009. 41:205–210.10. Gancarczyk KJ, Wu H, McLeod DG, Kane C, Kusuda L, Lance R, et al. Using the percentage of biopsy cores positive for cancer, pretreatment PSA, and highest biopsy Gleason sum to predict pathologic stage after radical prostatectomy: the Center for Prostate Disease Research nomograms. Urology. 2003. 61:589–595.11. Ishida M, Nakashima J, Hashiguchi A, Mizuno R, Shinoda K, Kikuchi E, et al. Are predictive models for cancer volume clinically useful in localized prostate cancer. Int J Urol. 2009. 16:936–940.12. Lee JT, Lee S, Yun CJ, Jeon BJ, Kim JM, Ha HK, et al. Prediction of perineural invasion and its prognostic value in patients with prostate cancer. Korean J Urol. 2010. 51:745–751.13. Nakanishi H, Troncoso P, Babaian RJ. Prediction of extraprostatic extension in men with biopsy Gleason score of 8 or greater. J Urol. 2008. 180:2441–2445.14. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Schnall M, Tomaszewski JE, et al. A multivariate analysis of clinical and pathological factors that predict for prostate specific antigen failure after radical prostatectomy for prostate cancer. J Urol. 1995. 154:131–138.15. Mian BM, Troncoso P, Okihara K, Bhadkamkar V, Johnston D, Reyes AO, et al. Outcome of patients with Gleason score 8 or higher prostate cancer following radical prostatectomy alone. J Urol. 2002. 167:1675–1680.16. Kattan MW, Stapleton AM, Wheeler TM, Scardino PT. Evaluation of a nomogram used to predict the pathologic stage of clinically localized prostate carcinoma. Cancer. 1997. 79:528–537.17. Partin AW, Kattan MW, Subong EN, Walsh PC, Wojno KJ, Oesterling JE. Combination of prostate specific antigen, clinical stage, and Gleason score to predict pathological stage of localized prostate cancer. A multi-institutional update. JAMA. 1997. 277:1445–1451.18. Graefen M, Haese A, Pichlmeier U, Hammerer PG, Noldus J, Butz K, et al. A validated strategy for side specific prediction of organ confined prostate cancer: a tool to select for nerve sparing radical prostatectomy. J Urol. 2001. 165:857–863.19. Naya Y, Slaton JW, Troncoso P, Okihara K, Babaian RJ. Tumor length and location of cancer on biopsy predict for side specific extraprostatic cancer extension. J Urol. 2004. 171:1093–1097.20. Tsuzuki T, Hernandez DJ, Aydin H, Trock B, Walsh PC, Epstein JI. Prediction of extraprostatic extension in the neurovascular bundle based on prostate needle biopsy pathology, serum prostate specific antigen and digital rectal examination. J Urol. 2005. 173:450–453.21. Cookson MS, Fleshner NE, Soloway SM, Fair WR. Correlation between Gleason score of needle biopsy and radical prostatectomy specimen: accuracy and clinical implications. J Urol. 1997. 157:559–562.22. Wang X, Brannigank RE, Rademaker AW, McVary KT, Oyasu R. One core positive prostate biopsy is a poor predictor of cancer volume in the radical prostatectomy specimen. J Urol. 1997. 158:1431–1435.23. Cheng L, Slezak J, Bergstralh EJ, Myers RP, Zincke H, Bostwick DG. Preoperative prediction of surgical margin status in patients with prostate cancer treated by radical prostatectomy. J Clin Oncol. 2000. 18:2862–2868.24. Gancarczyk KJ, Wu H, McLeod DG, Kane C, Kusuda L, Lance R, et al. Using the percentage of biopsy cores positive for cancer, pretreatment PSA, and highest biopsy Gleason sum to predict pathologic stage after radical prostatectomy: the Center for Prostate Disease Research nomograms. Urology. 2003. 61:589–595.25. Noguchi M, Stamey TA, McNeal JE, Yemoto CM. Relationship between systematic biopsies and histological features of 222 radical prostatectomy specimens: lack of prediction of tumor significance for men with nonpalpable prostate cancer. J Urol. 2001. 166:104–109.26. Noldus J, Stamey TA. Limitations of serum prostate specific antigen in predicting peripheral and transition zone cancer volumes as measured by correlation coefficients. J Urol. 1996. 155:232–237.27. Seaman EK, Whang IS, Cooner W, Olsson CA, Benson MC. Predictive value of prostate-specific antigen density for the presence of micrometastatic carcinoma of the prostate. Urology. 1994. 43:645–648.28. Taneja SS, Hsu EI, Cheli CD, Walden P, Bartsch G, Horninger W, et al. Complexed prostate-specific antigen as a staging tool: results based on a multicenter prospective evaluation of complexed prostate-specific antigen in cancer diagnosis. Urology. 2002. 60:4 Suppl 1. 10–17.29. Naya Y, Fritsche HA, Cheli CD, Stamey TA, Bartsch G, Brawer MK, et al. Volume indexes of total, free, and complexed prostate- specific antigen enhance prediction of extraprostatic disease extension in men with nonpalpable prostate cancer. Urology. 2003. 62:1058–1062.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcome of Radical Prostatectomy in Prostate Cancer Patients with Prostate-Specific Antigen (PSA) Level Equal to or More Than 20 ng/ml and No Distant Metastasis Preoperatively
- Radical Prostatectomy
- The Impact of PSA on Pathologic Characteristics in the Radical Prostatectomy with PSA Level of 4-10ng/ml
- The Preoperative Factors Predicting a Positive Frozen Section during Radical Prostatectomy for Prostate Cancer
- Prostate specific antigen as a tumor marker for adenocarcinoma of the prostate