Pediatr Gastroenterol Hepatol Nutr.
2012 Sep;15(3):151-159.
Childhood Obesity and Pubertal Development
- Affiliations
-
- 1Department of Pediatrics, Inje University Sanggye Paik Hospital, Seoul, Korea. PMJ@paik.ac.kr
Abstract
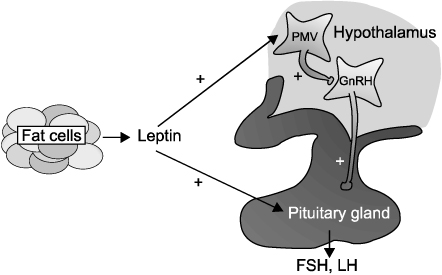
- During the past decades, advancement in pubertal maturation in children has been noticed worldwide. Growing evidence indicates that increasing prevalence of obesity in children is a major factor for the secular trend of earlier puberty. In girls, several epidemiologic studies suggest that earlier pubertal onset and earlier menarche might be caused by obesity. On the other hand, in boys, few research reported an association between obesity and pubertal development, and the results are inconsistent; Some studies found a link between obesity and delayed puberty, but others reported a causal relationship between obesity and early puberty. To date, mechanisms linking childhood obesity and earlier puberty remain unclear. In this review, we presented the potential impact of obesity on puberty-related hormones and summarized human studies on potential relationship of childhood adiposity and pubertal development.
Keyword
MeSH Terms
Figure
Reference
-
1. Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, Bourguignon JP. The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocr Rev. 2003. 24:668–693.
Article2. Tanner JM, Davies PS. Clinical longitudinal standards for height and height velocity for North American children. J Pediatr. 1985. 107:317–329.
Article3. National Center for Health Statistics. Analytic and reporting guidelines: the third National Health and Nutrition Examination Survey, NHANES III (1988-94). 1997. Hyattsville: Center for Disease Control and Prevention.4. Aksglaede L, Sørensen K, Petersen JH, Skakkebaek NE, Juul A. Recent decline in age at breast development: the Copenhagen Puberty Study. Pediatrics. 2009. 123:e932–e939.
Article5. Ma HM, Du ML, Luo XP, Chen SK, Liu L, Chen RM, et al. Pubertal Study Group of the Society of Pediatric Endocrinology and Genetic Disease, Chinese Medical Association. Onset of breast and pubic hair development and menses in urban chinese girls. Pediatrics. 2009. 124:e269–e277.
Article6. Park MJ, Lee IS, Shin EK, Joung H, Cho SI. The timing of sexual maturation and secular trends of menarchial age in Korean adolescents. Korean J Pediatr. 2006. 49:610–616.
Article7. Herman-Giddens ME, Slora EJ, Wasserman RC, Bourdony CJ, Bhapkar MV, Koch GG, et al. Secondary sexual characteristics and menses in young girls seen in office practice: a study from the Pediatric Research in Office Settings network. Pediatrics. 1997. 99:505–512.
Article8. Tsuzaki S, Matsuo N, Ogata T, Osano M. Lack of linkage between height and weight and age at menarche during the secular shift in growth of Japanese children. Ann Hum Biol. 1989. 16:429–436.
Article9. de Muinich Keizer SM, Mul D. Trends in pubertal development in Europe. Hum Reprod Update. 2001. 7:287–291.
Article10. Mul D, Fredriks AM, van Buuren S, Oostdijk W, Verloove-Vanhorick SP, Wit JM. Pubertal development in The Netherlands 1965-1997. Pediatr Res. 2001. 50:479–486.
Article11. Herman-Giddens ME, Wang L, Koch G. Secondary sexual characteristics in boys: estimates from the national health and nutrition examination survey III, 1988-1994. Arch Pediatr Adolesc Med. 2001. 155:1022–1028.12. Sørensen K, Aksglaede L, Petersen JH, Juul A. Recent changes in pubertal timing in healthy Danish boys: associations with body mass index. J Clin Endocrinol Metab. 2010. 95:263–270.
Article13. Song JE, Yi YY, Hwang IT, Lee HR, Lim JS, Yang S. Testicular volume in Korean boys. J Korean Soc Pediatr Endocrinol. 2010. 15:14–18.14. Ma HM, Chen SK, Chen RM, Zhu C, Xiong F, Li T, et al. Pubertal Study Group of the Society of Pediatric Endocrinology and Genetic Disease, Chinese Medical Association. Pubertal development timing in urban Chinese boys. Int J Androl. 2011. 34:e435–e445.
Article15. Ogden C, Carroll M. Prevalence of obesity among children and adolescents: United States, trends 1963-1965 through 2007-2008. Retrieved from National center for health statistics, Center for Disease Control and Prevention. Last accessed on 30 July 2012. Available from: http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.pdf.16. Chinn S, Rona RJ. Prevalence and trends in overweight and obesity in three cross sectional studies of British Children, 1974-94. BMJ. 2001. 322:24–26.
Article17. Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006. 1:11–25.
Article18. Magarey AM, Daniels LA, Boulton TJ. Prevalence of overweight and obesity in Australian children and adolescents: reassessment of 1985 and 1995 data against new standard international definitions. Med J Aust. 2001. 174:561–564.
Article19. Wang Y, Monteiro C, Popkin BM. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am J Clin Nutr. 2002. 75:971–977.
Article20. Murata M. Secular trends in growth and changes in eating patterns of Japanese children. Am J Clin Nutr. 2000. 72:5 Suppl. 1379S–1383S.
Article21. Chu MA, Choe BH. Obesity and metabolic syndrome among children and adolescents in Korea. J Korean Med Assoc. 2010. 53:142–152.
Article22. Moon JS. Secular trends of body sizes in Korean children and adolescents: from 1965 to 2010. Korean J Pediatr. 2011. 54:436–442.
Article23. Kaplowitz PB, Slora EJ, Wasserman RC, Pedlow SE, Herman-Giddens ME. Earlier onset of puberty in girls: relation to increased body mass index and race. Pediatrics. 2001. 108:347–353.
Article24. Wang Y. Is obesity associated with early sexual maturation? A comparison of the association in American boys versus girls. Pediatrics. 2002. 110:903–910.
Article25. Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Relation of age at menarche to race, time period, and anthropometric dimensions: the Bogalusa Heart Study. Pediatrics. 2002. 110:e43.
Article26. Frisch RE, Revelle R. Height and weight at menarche and a hypothesis of menarche. Arch Dis Child. 1971. 46:695–701.
Article27. Grumbach MM. The neuroendocrinology of human puberty revisited. Horm Res. 2002. 57:Suppl 2. 2–14.
Article28. Coleman DL. Obese and diabetes: two mutant genes causing diabetes-obesity syndromes in mice. Diabetologia. 1978. 14:141–148.
Article29. Chehab FF, Lim ME, Lu R. Correction of the sterility defect in homozygous obese female mice by treatment with the human recombinant leptin. Nat Genet. 1996. 12:318–320.
Article30. Clément K, Vaisse C, Lahlou N, Cabrol S, Pelloux V, Cassuto D, et al. A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction. Nature. 1998. 392:398–401.
Article31. Strobel A, Issad T, Camoin L, Ozata M, Strosberg AD. A leptin missense mutation associated with hypogonadism and morbid obesity. Nat Genet. 1998. 18:213–215.
Article32. Farooqi IS, Jebb SA, Langmack G, Lawrence E, Cheetham CH, Prentice AM, et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N Engl J Med. 1999. 341:879–884.
Article33. Welt CK, Chan JL, Bullen J, Murphy R, Smith P, DePaoli AM, et al. Recombinant human leptin in women with hypothalamic amenorrhea. N Engl J Med. 2004. 351:987–997.
Article34. Cheung CC, Thornton JE, Kuijper JL, Weigle DS, Clifton DK, Steiner RA. Leptin is a metabolic gate for the onset of puberty in the female rat. Endocrinology. 1997. 138:855–858.
Article35. Cheung CC, Thornton JE, Nurani SD, Clifton DK, Steiner RA. A reassessment of leptin's role in triggering the onset of puberty in the rat and mouse. Neuroendocrinology. 2001. 74:12–21.
Article36. Clayton PE, Gill MS, Hall CM, Tillmann V, Whatmore AJ, Price DA. Serum leptin through childhood and adolescence. Clin Endocrinol (Oxf). 1997. 46:727–733.
Article37. Ahmed ML, Ong KK, Morrell DJ, Cox L, Drayer N, Perry L, et al. Longitudinal study of leptin concentrations during puberty: sex differences and relationship to changes in body composition. J Clin Endocrinol Metab. 1999. 84:899–905.
Article38. Jin L, Burguera BG, Couce ME, Scheithauer BW, Lamsan J, Eberhardt NL, et al. Leptin and leptin receptor expression in normal and neoplastic human pituitary: evidence of a regulatory role for leptin on pituitary cell proliferation. J Clin Endocrinol Metab. 1999. 84:2903–2911.
Article39. Yu WH, Kimura M, Walczewska A, Karanth S, McCann SM. Role of leptin in hypothalamic-pituitary function. Proc Natl Acad Sci U S A. 1997. 94:1023–1028.40. Donato J Jr, Cravo RM, Frazão R, Gautron L, Scott MM, Lachey J, et al. Leptin's effect on puberty in mice is relayed by the ventral premammillary nucleus and does not require signaling in Kiss1 neurons. J Clin Invest. 2011. 121:355–368.
Article41. Dennis MS, Melvin MG. Shlomo M, Kenneth SP, Larsen PR, Kronenberg HM, editors. Chapter 25. Puberty: Ontogeny, neuroendocrinology, physiology, and disorders. Williams textbook of endocrinology. 2011. 12th ed. Philadelphia: WB Saunders Co.;1087–1104.42. Moran A, Jacobs DR Jr, Steinberger J, Cohen P, Hong CP, Prineas R, et al. Association between the insulin resistance of puberty and the insulin-like growth factor-I/growth hormone axis. J Clin Endocrinol Metab. 2002. 87:4817–4820.
Article43. Roemmich JN, Clark PA, Lusk M, Friel A, Weltman A, Epstein LH, et al. Pubertal alterations in growth and body composition. VI. Pubertal insulin resistance: relation to adiposity, body fat distribution and hormone release. Int J Obes Relat Metab Disord. 2002. 26:701–709.
Article44. Saenger P, Dimartino-Nardi J. Premature adrenarche. J Endocrinol Invest. 2001. 24:724–733.
Article45. Shalitin S, Phillip M. Role of obesity and leptin in the pubertal process and pubertal growth--a review. Int J Obes Relat Metab Disord. 2003. 27:869–874.
Article46. Ong KK, Loos RJ. Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions. Acta Paediatr. 2006. 95:904–908.
Article47. Ibáñez L, Dimartino-Nardi J, Potau N, Saenger P. Premature adrenarche--normal variant or forerunner of adult disease? Endocr Rev. 2000. 21:671–696.
Article48. Ong KK, Potau N, Petry CJ, Jones R, Ness AR, Honour JW, et al. Avon Longitudinal Study of Parents and Children Study Team. Opposing influences of prenatal and postnatal weight gain on adrenarche in normal boys and girls. J Clin Endocrinol Metab. 2004. 89:2647–2651.
Article49. Ibáñez L, Jiménez R, de Zegher F. Early puberty-menarche after precocious pubarche: relation to prenatal growth. Pediatrics. 2006. 117:117–121.
Article50. Ibáñez L, Ong K, Valls C, Marcos MV, Dunger DB, de Zegher F. Metformin treatment to prevent early puberty in girls with precocious pubarche. J Clin Endocrinol Metab. 2006. 91:2888–2891.
Article51. Holly JM, Smith CP, Dunger DB, Howell RJ, Chard T, Perry LA, et al. Relationship between the pubertal fall in sex hormone binding globulin and insulin-like growth factor binding protein-I. A synchronized approach to pubertal development? Clin Endocrinol (Oxf). 1989. 31:277–284.
Article52. Poretsky L, Cataldo NA, Rosenwaks Z, Giudice LC. The insulin-related ovarian regulatory system in health and disease. Endocr Rev. 1999. 20:535–582.
Article53. Ahmed ML, Ong KK, Dunger DB. Childhood obesity and the timing of puberty. Trends Endocrinol Metab. 2009. 20:237–242.
Article54. Himes JH, Obarzanek E, Baranowski T, Wilson DM, Rochon J, McClanahan BS. Early sexual maturation, body composition, and obesity in African-American girls. Obes Res. 2004. 12:Suppl. 64S–72S.
Article55. Anderson SE, Dallal GE, Must A. Relative weight and race influence average age at menarche: results from two nationally representative surveys of US girls studied 25 years apart. Pediatrics. 2003. 111:844–850.
Article56. Rosenfield RL, Lipton RB, Drum ML. Thelarche, pubarche, and menarche attainment in children with normal and elevated body mass index. Pediatrics. 2009. 123:84–88.
Article57. Mamun AA, Hayatbakhsh MR, O'Callaghan M, Williams G, Najman J. Early overweight and pubertal maturation--pathways of association with young adults' overweight: a longitudinal study. Int J Obes (Lond). 2009. 33:14–20.
Article58. Buyken AE, Karaolis-Danckert N, Remer T. Association of prepubertal body composition in healthy girls and boys with the timing of early and late pubertal markers. Am J Clin Nutr. 2009. 89:221–230.
Article59. Boyne MS, Thame M, Osmond C, Fraser RA, Gabay L, Reid M, et al. Growth, body composition, and the onset of puberty: longitudinal observations in Afro-Caribbean children. J Clin Endocrinol Metab. 2010. 95:3194–3200.
Article60. Yoon JR, Ahn JH, Huh K, Park MJ. Body composition in girls with precocious puberty. Korean J Obes. 2010. 19:95–100.61. Vignolo M, Naselli A, Di Battista E, Mostert M, Aicardi G. Growth and development in simple obesity. Eur J Pediatr. 1988. 147:242–244.
Article62. Lee JM, Kaciroti N, Appugliese D, Corwyn RF, Bradley RH, Lumeng JC. Body mass index and timing of pubertal initiation in boys. Arch Pediatr Adolesc Med. 2010. 164:139–144.
Article63. Burt Solorzano CM, McCartney CR. Obesity and the pubertal transition in girls and boys. Reproduction. 2010. 140:399–410.
Article64. Vizmanos B, Martí-Henneberg C. Puberty begins with a characteristic subcutaneous body fat mass in each sex. Eur J Clin Nutr. 2000. 54:203–208.
Article65. He Q, Karlberg J. Bmi in childhood and its association with height gain, timing of puberty, and final height. Pediatr Res. 2001. 49:244–251.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Growth and Puberty in Obese Children and Implications of Body Composition
- A Clinical Study of the Relationship between Obesity and Pubertal Development in Girls
- A Review of Childhood Obesity
- Link between obesity and growth in children and adolescents
- What is the disease burden from childhood and adolescent obesity?: a narrative review