Nutr Res Pract.
2014 Jun;8(3):233-240.
Diet components can suppress inflammation and reduce cancer risk
- Affiliations
-
- 1Department of Biochemistry and Microbiology, Marshall University Joan C. Edwards School of Medicine, 1600 Medical Center Dr., Huntington, West Virginia 25701-3655, USA. hardmanw@marshall.edu
Abstract
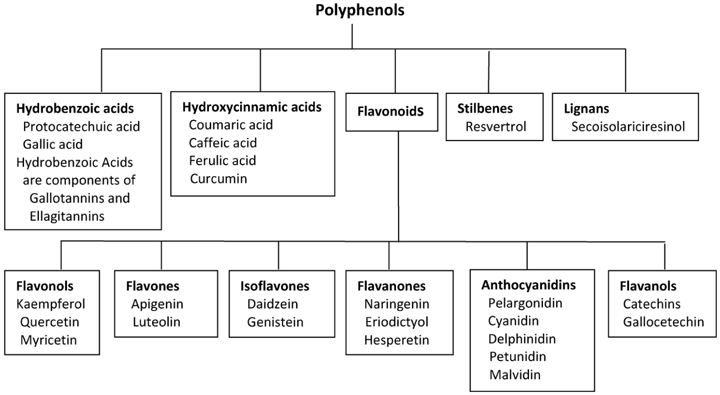
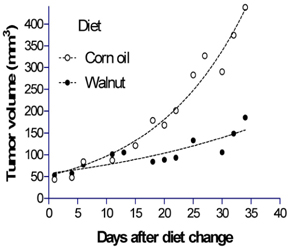
- Epidemiology studies indicate that diet or specific dietary components can reduce the risk for cancer, cardiovascular disease and diabetes. An underlying cause of these diseases is chronic inflammation. Dietary components that are beneficial against disease seem to have multiple mechanisms of action and many also have a common mechanism of reducing inflammation, often via the NFkappaB pathway. Thus, a plant based diet can contain many components that reduce inflammation and can reduce the risk for developing all three of these chronic diseases. We summarize dietary components that have been shown to reduce cancer risk and two studies that show that dietary walnut can reduce cancer growth and development. Part of the mechanism for the anticancer benefit of walnut was by suppressing the activation of NFkappaB. In this brief review, we focus on reduction of cancer risk by dietary components and the relationship to suppression of inflammation. However, it should be remembered that most dietary components have multiple beneficial mechanisms of action that can be additive and that suppression of chronic inflammation should reduce the risk for all three chronic diseases.
Keyword
MeSH Terms
Figure
Reference
-
1. Doll R, Peto R. The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. J Natl Cancer Inst. 1981; 66:1191–1308.
Article2. World Cancer Research Fund. American Institute for Cancer Research (US). Food, Nutrition and the Prevention of Cancer: a Global Perspective. Washington, D.C.: American Institute for Cancer Research;1997.3. World Cancer Research Fund. American Institute for Cancer Research (US). Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective. Washington, D.C.: American Institute for Cancer Research;2007.4. Rhodes JM. Unifying hypothesis for inflammatory bowel disease and associated colon cancer: sticking the pieces together with sugar. Lancet. 1996; 347:40–44.
Article5. Grce M, Mravak-Stipetić M. Human papillomavirus-associated diseases. Clin Dermatol. 2014; 32:253–258.
Article6. Rambau PF, Chalya PL, Jackson K. Schistosomiasis and urinary bladder cancer in North Western Tanzania: a retrospective review of 185 patients. Infect Agent Cancer. 2013; 8:19.
Article7. Qadri Q, Rasool R, Gulzar GM, Naqash S, Shah ZA. H. pylori infection, inflammation and gastric cancer. J Gastrointest Cancer. Forthcoming 2014.
Article8. Donath MY, Dalmas É, Sauter NS, Böni-Schnetzler M. Inflammation in obesity and diabetes: islet dysfunction and therapeutic opportunity. Cell Metab. 2013; 17:860–872.
Article9. Crujeiras AB, Díaz-Lagares A, Carreira MC, Amil M, Casanueva FF. Oxidative stress associated to dysfunctional adipose tissue: a potential link between obesity, type 2 diabetes mellitus and breast cancer. Free Radic Res. 2013; 47:243–256.
Article10. Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001; 357:539–545.
Article11. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002; 420:860–867.
Article12. Aroor AR, McKarns S, Demarco VG, Jia G, Sowers JR. Maladaptive immune and inflammatory pathways lead to cardiovascular insulin resistance. Metabolism. 2013; 62:1543–1552.
Article13. Lee H, Lee IS, Choue R. Obesity, inflammation and diet. Pediatr Gastroenterol Hepatol Nutr. 2013; 16:143–152.
Article14. Tarantino G, Capone D. Inhibition of the mTOR pathway: a possible protective role in coronary artery disease. Ann Med. 2013; 45:348–356.
Article15. Chen F, Castranova V. Nuclear factor-kappaB, an unappreciated tumor suppressor. Cancer Res. 2007; 67:11093–11098.16. Aggarwal BB. Nuclear factor-kappaB: the enemy within. Cancer Cell. 2004; 6:203–208.17. Lin WW, Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J Clin Invest. 2007; 117:1175–1183.
Article18. Karin M, Greten FR. NF-kappaB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol. 2005; 5:749–759.
Article19. Miyamoto S. Nuclear initiated NF-kappaB signaling: NEMO and ATM take center stage. Cell Res. 2011; 21:116–130.
Article20. Bours V, Bonizzi G, Bentires-Alj M, Bureau F, Piette J, Lekeux P, Merville M. NF-kappaB activation in response to toxical and therapeutical agents: role in inflammation and cancer treatment. Toxicology. 2000; 153:27–38.
Article21. Clevers H. At the crossroads of inflammation and cancer. Cell. 2004; 118:671–674.
Article22. Cao Y, Karin M. NF-kappaB in mammary gland development and breast cancer. J Mammary Gland Biol Neoplasia. 2003; 8:215–223.23. Karin M, Cao Y, Greten FR, Li ZW. NF-kappaB in cancer: from innocent bystander to major culprit. Nat Rev Cancer. 2002; 2:301–310.
Article24. Jin RJ, Lho Y, Connelly L, Wang Y, Yu X, Saint Jean L, Case TC, Ellwood-Yen K, Sawyers CL, Bhowmick NA, Blackwell TS, Yull FE, Matusik RJ. The nuclear factor-kappaB pathway controls the progression of prostate cancer to androgen-independent growth. Cancer Res. 2008; 68:6762–6769.
Article25. Kim HJ, Hawke N, Baldwin AS. NF-kappaB and IKK as therapeutic targets in cancer. Cell Death Differ. 2006; 13:738–747.26. Bharti AC, Shishodia S, Reuben JM, Weber D, Alexanian R, Raj-Vadhan S, Estrov Z, Talpaz M, Aggarwal BB. Nuclear factor-kappaB and STAT3 are constitutively active in CD138 + cells derived from multiple myeloma patients, and suppression of these transcription factors leads to apoptosis. Blood. 2004; 103:3175–3184.
Article27. Gupta SC, Kim JH, Prasad S, Aggarwal BB. Regulation of survival, proliferation, invasion, angiogenesis, and metastasis of tumor cells through modulation of inflammatory pathways by nutraceuticals. Cancer Metastasis Rev. 2010; 29:405–434.
Article28. Potter JD, Steinmetz K. Vegetables, fruit and phytoestrogens as preventive agents. IARC Sci Publ. 1996; 61–90.29. Chan JM, Gann PH, Giovannucci EL. Role of diet in prostate cancer development and progression. J Clin Oncol. 2005; 23:8152–8160.
Article30. Manach C, Scalbert A, Morand C, Rémésy C, Jiménez L. Polyphenols: food sources and bioavailability. Am J Clin Nutr. 2004; 79:727–747.
Article31. Oseni T, Patel R, Pyle J, Jordan VC. Selective estrogen receptor modulators and phytoestrogens. Planta Med. 2008; 74:1656–1665.
Article32. Horia E, Watkins BA. Complementary actions of docosahexaenoic acid and genistein on COX-2, PGE2 and invasiveness in MDA-MB-231 breast cancer cells. Carcinogenesis. 2007; 28:809–815.
Article33. Sakamoto Y, Naka A, Ohara N, Kondo K, Iida K. Daidzein regulates proinflammatory adipokines thereby improving obesity-related inflammation through PPARγ. Mol Nutr Food Res. 2014; 58:718–726.
Article34. Brusselmans K, Vrolix R, Verhoeven G, Swinnen JV. Induction of cancer cell apoptosis by flavonoids is associated with their ability to inhibit fatty acid synthase activity. J Biol Chem. 2005; 280:5636–5645.
Article35. O'Leary KA, de Pascual-Teresa S, Needs PW, Bao YP, O'Brien NM, Williamson G. Effect of flavonoids and vitamin E on cyclooxygenase-2 (COX-2) transcription. Mutat Res. 2004; 551:245–254.36. Bae JH, Kim JY, Kim MJ, Chang SH, Park YS, Son CH, Park SJ, Chung JS, Lee EY, Kim SH, Kang CD. Quercetin enhances susceptibility to NK cell-mediated lysis of tumor cells through induction of NKG2D ligands and suppression of HSP70. J Immunother. 2010; 33:391–401.
Article37. Wang G, Zhang J, Liu L, Sharma S, Dong Q. Quercetin potentiates doxorubicin mediated antitumor effects against liver cancer through p53/Bcl-xl. PLoS One. 2012; 7:e51764.
Article38. Chen AY, Chen YC. A review of the dietary flavonoid, kaempferol on human health and cancer chemoprevention. Food Chem. 2013; 138:2099–2107.
Article39. Delgado L, Fernandes I, González-Manzano S, de Freitas V, Mateus N, Santos-Buelga C. Anti-proliferative effects of quercetin and catechin metabolites. Food Funct. 2014; 5:797–803.
Article40. Al-Hanbali M, Ali D, Bustami M, Abdel-Malek S, Al-Hanbali R, Alhussainy T, Qadan F, Matalka KZ. Epicatechin suppresses IL-6, IL-8 and enhances IL-10 production with NF-kappaB nuclear translocation in whole blood stimulated system. Neuro Endocrinol Lett. 2009; 30:131–138.41. Shan X, Li Y, Meng X, Wang P, Jiang P, Feng Q. Curcumin and (-)-epigallocatechin-3-gallate attenuate acrylamide-induced proliferation in HepG2 cells. Food Chem Toxicol. 2014; 66:194–202.
Article42. Saldanha SN, Kala R, Tollefsbol TO. Molecular mechanisms for inhibition of colon cancer cells by combined epigenetic-modulating epigallocatechin gallate and sodium butyrate. Exp Cell Res. Forthcoming 2014.
Article43. Thangapazham RL, Singh AK, Sharma A, Warren J, Gaddipati JP, Maheshwari RK. Green tea polyphenols and its constituent epigallocatechin gallate inhibits proliferation of human breast cancer cells in vitro and in vivo. Cancer Lett. 2007; 245:232–241.
Article44. Carter LG, D'Orazio JA, Pearson KJ. Resveratrol and cancer: a focus on in vivo evidence. Endocr Relat Cancer. Forthcoming 2014.45. Mezzanotte L, An N, Mol IM, Löwik CW, Kaijzel EL. A new multicolor bioluminescence imaging platform to investigate NF-κB activity and apoptosis in human breast cancer cells. PLoS One. 2014; 9:e85550.
Article46. Mazué F, Delmas D, Murillo G, Saleiro D, Limagne E, Latruffe N. Differential protective effects of red wine polyphenol extracts (RWEs) on colon carcinogenesis. Food Funct. 2014; 5:663–670.
Article47. Garcia-Muñoz C, Vaillant F. Metabolic fate of ellagitannins: implications for health, and research perspectives for innovative functional foods. Crit Rev Food Sci Nutr. 2014; 54:1584–1598.
Article48. Rodriguez-Mateos A, Heiss C, Borges G, Crozier A. Berry (Poly) phenols and cardiovascular health. J Agric Food Chem. Forthcoming 2013.49. Nuñez-Sánchez MA, García-Villalba R, Monedero-Saiz T, García-Talavera NV, Gómez-Sánchez MB, Sánchez-Álvarez C, García-Albert AM, Rodríguez-Gil FJ, Ruiz-Marín M, Pastor-Quirante FA, Martínez-Díaz F, Yáñez-Gascón MJ, González-Sarrías A, Tomás-Barberán FA, Espín JC. Targeted metabolic profiling of pomegranate polyphenols and urolithins in plasma, urine and colon tissues from colorectal cancer patients. Mol Nutr Food Res. Forthcoming 2014.
Article50. Banerjee N, Kim H, Talcott S, Mertens-Talcott S. Pomegranate polyphenolics suppressed azoxymethane-induced colorectal aberrant crypt foci and inflammation: possible role of miR-126/VCAM-1 and miR-126/PI3K/AKT/mTOR. Carcinogenesis. 2013; 34:2814–2822.
Article51. González-Sarrías A, Miguel V, Merino G, Lucas R, Morales JC, Tomás-Barberán F, Alvarez AI, Espín JC. The gut microbiota ellagic acid-derived metabolite urolithin A and its sulfate conjugate are substrates for the drug efflux transporter breast cancer resistance protein (ABCG2/BCRP). J Agric Food Chem. 2013; 61:4352–4359.
Article52. Kita T, Imai S, Sawada H, Kumagai H, Seto H. The biosynthetic pathway of curcuminoid in turmeric (Curcuma longa) as revealed by 13C-labeled precursors. Biosci Biotechnol Biochem. 2008; 72:1789–1798.
Article53. Aggarwal BB, Sung B. Pharmacological basis for the role of curcumin in chronic diseases: an age-old spice with modern targets. Trends Pharmacol Sci. 2009; 30:85–94.
Article54. Anand P, Thomas SG, Kunnumakkara AB, Sundaram C, Harikumar KB, Sung B, Tharakan ST, Misra K, Priyadarsini IK, Rajasekharan KN, Aggarwal BB. Biological activities of curcumin and its analogues (Congeners) made by man and Mother Nature. Biochem Pharmacol. 2008; 76:1590–1611.
Article55. Liu T, Bohlken A, Kuljaca S, Lee M, Nguyen T, Smith S, Cheung B, Norris MD, Haber M, Holloway AJ, Bowtell DD, Marshall GM. The retinoid anticancer signal: mechanisms of target gene regulation. Br J Cancer. 2005; 93:310–318.
Article56. Moon RC, Constantinou AI. Dietary retinoids and carotenoids in rodent models of mammary tumorigenesis. Breast Cancer Res Treat. 1997; 46:181–189.
Article57. Tamimi RM, Hankinson SE, Campos H, Spiegelman D, Zhang S, Colditz GA, Willett WC, Hunter DJ. Plasma carotenoids, retinol, and tocopherols and risk of breast cancer. Am J Epidemiol. 2005; 161:153–160.
Article58. Rao AV, Rao LG. Carotenoids and human health. Pharmacol Res. 2007; 55:207–216.
Article59. Wang L, Li B, Pan MX, Mo XF, Chen YM, Zhang CX. Specific carotenoid intake is inversely associated with the risk of breast cancer among Chinese women. Br J Nutr. 2014; 111:1686–1695.
Article60. Takeshima M, Ono M, Higuchi T, Chen C, Hara T, Nakano S. Anti-proliferative and apoptosis-inducing activity of lycopene against three subtypes of human breast cancer cell lines. Cancer Sci. 2014; 105:252–257.
Article61. Zu K, Mucci L, Rosner BA, Clinton SK, Loda M, Stampfer MJ, Giovannucci E. Dietary lycopene, angiogenesis, and prostate cancer: a prospective study in the prostate-specific antigen era. J Natl Cancer Inst. 2014; 106:djt430.
Article62. Brigelius-Flohé R, Traber MG. Vitamin E: function and metabolism. FASEB J. 1999; 13:1145–1155.
Article63. Campbell SE, Stone WL, Whaley SG, Qui M, Krishnan K. Gamma (γ) tocopherol upregulates peroxisome proliferator activated receptor (PPAR) gamma (γ) expression in SW 480 human colon cancer cell lines. BMC Cancer. 2003; 3:25.
Article64. Lee HJ, Ju J, Paul S, So JY, DeCastro A, Smolarek A, Lee MJ, Yang CS, Newmark HL, Suh N. Mixed tocopherols prevent mammary tumorigenesis by inhibiting estrogen action and activating PPAR-gamma. Clin Cancer Res. 2009; 15:4242–4249.
Article65. Dolfi SC, Yang Z, Lee MJ, Guan F, Hong J, Yang CS. Inhibitory effects of different forms of tocopherols, tocopherol phosphates, and tocopherol quinones on growth of colon cancer cells. J Agric Food Chem. 2013; 61:8533–8540.
Article66. Lu G, Xiao H, Li GX, Picinich SC, Chen YK, Liu A, Lee MJ, Loy S, Yang CS. A gamma-tocopherol-rich mixture of tocopherols inhibits chemically induced lung tumorigenesis in A/J mice and xenograft tumor growth. Carcinogenesis. 2010; 31:687–694.
Article67. Park HS, Han MH, Kim GY, Moon SK, Kim WJ, Hwang HJ, Park KY, Choi YH. Sulforaphane induces reactive oxygen species-mediated mitotic arrest and subsequent apoptosis in human bladder cancer 5637 cells. Food Chem Toxicol. 2014; 64:157–165.
Article68. Hussain A, Mohsin J, Prabhu SA, Begum S, Nusri Qel A, Harish G, Javed E, Khan MA, Sharma C. Sulforaphane inhibits growth of human breast cancer cells and augments the therapeutic index of the chemotherapeutic drug, gemcitabine. Asian Pac J Cancer Prev. 2013; 14:5855–5860.
Article69. Lenzi M, Fimognari C, Hrelia P. Sulforaphane as a promising molecule for fighting cancer. Cancer Treat Res. 2014; 159:207–223.
Article70. Wolf MA, Claudio PP. Benzyl isothiocyanate inhibits HNSCC cell migration and invasion, and sensitizes HNSCC cells to cisplatin. Nutr Cancer. 2014; 66:285–294.
Article71. Tse G, Eslick GD. Cruciferous vegetables and risk of colorectal neoplasms: a systematic review and meta-analysis. Nutr Cancer. 2014; 66:128–139.
Article72. Tusskorn O, Senggunprai L, Prawan A, Kukongviriyapan U, Kukongviriyapan V. Phenethyl isothiocyanate induces calcium mobilization and mitochondrial cell death pathway in cholangiocarcinoma KKU-M214 cells. BMC Cancer. 2013; 13:571.
Article73. Liu H, Talalay P. Relevance of anti-inflammatory and antioxidant activities of exemestane and synergism with sulforaphane for disease prevention. Proc Natl Acad Sci U S A. 2013; 110:19065–19070.
Article74. Schäfer G, Kaschula CH. The immunomodulation and anti-inflammatory effects of garlic organosulfur compounds in cancer chemoprevention. Anticancer Agents Med Chem. 2014; 14:233–240.
Article75. Zhou XF, Ding ZS, Liu NB. Allium vegetables and risk of prostate cancer: evidence from 132,192 subjects. Asian Pac J Cancer Prev. 2013; 14:4131–4134.
Article76. Borkowska A, Knap N, Antosiewicz J. Diallyl trisulfide is more cytotoxic to prostate cancer cells PC-3 than to noncancerous epithelial cell line PNT1A: a possible role of p66Shc signaling axis. Nutr Cancer. 2013; 65:711–717.
Article77. García JJ, López-Pingarrón L, Almeida-Souza P, Tres A, Escudero P, García-Gil FA, Tan DX, Reiter RJ, Ramírez JM, Bernal-Pérez M. Protective effects of melatonin in reducing oxidative stress and in preserving the fluidity of biological membranes: a review. J Pineal Res. 2014; 56:225–237.
Article78. Reiter RJ, Tan DX, Manchester LC, Korkmaz A, Fuentes-Broto L, Hardman WE, Rosales-Corral SA, Qi W. A walnut-enriched diet reduces the growth of LNCaP human prostate cancer xenografts in nude mice. Cancer Invest. 2013; 31:365–373.
Article79. Lv D, Cui PL, Yao SW, Xu YQ, Yang ZX. Melatonin inhibits the expression of vascular endothelial growth factor in pancreatic cancer cells. Chin J Cancer Res. 2012; 24:310–316.
Article80. Srinivasan V, Spence DW, Pandi-Perumal SR, Trakht I, Esquifino AI, Cardinali DP, Maestroni GJ. Melatonin, environmental light, and breast cancer. Breast Cancer Res Treat. 2008; 108:339–350.
Article81. García-Navarro A, González-Puga C, Escames G, López LC, López A, López-Cantarero M, Camacho E, Espinosa A, Gallo MA, Acuña-Castroviejo D. Cellular mechanisms involved in the melatonin inhibition of HT-29 human colon cancer cell proliferation in culture. J Pineal Res. 2007; 43:195–205.
Article82. Rodriguez C, Martín V, Herrera F, García-Santos G, Rodriguez-Blanco J, Casado-Zapico S, Sánchez-Sánchez AM, Suárez S, Puente-Moncada N, Anítua MJ, Antolín I. Mechanisms involved in the pro-apoptotic effect of melatonin in cancer cells. Int J Mol Sci. 2013; 14:6597–6613.
Article83. Wu KK. Control of cyclooxygenase-2 transcriptional activation by pro-inflammatory mediators. Prostaglandins Leukot Essent Fatty Acids. 2005; 72:89–93.
Article84. Akinsete JA, Ion G, Witte TR, Hardman WE. Consumption of high omega-3 fatty acid diet suppressed prostate tumorigenesis in C3(1) Tag mice. Carcinogenesis. 2012; 33:140–148.
Article85. Badawi AF, El-Sohemy A, Stephen LL, Ghoshal AK, Archer MC. The effect of dietary n-3 and n-6 polyunsaturated fatty acids on the expression of cyclooxygenase 1 and 2 and levels of p21ras in rat mammary glands. Carcinogenesis. 1998; 19:905–910.
Article86. Berquin IM, Edwards IJ, Chen YQ. Multi-targeted therapy of cancer by omega-3 fatty acids. Cancer Lett. 2008; 269:363–377.
Article87. Biondo PD, Brindley DN, Sawyer MB, Field CJ. The potential for treatment with dietary long-chain polyunsaturated n-3 fatty acids during chemotherapy. J Nutr Biochem. 2008; 19:787–796.
Article88. Blok WL, Katan MB, van der Meer JW. Modulation of inflammation and cytokine production by dietary (n-3) fatty acids. J Nutr. 1996; 126:1515–1533.
Article89. Bougnoux P, Germain E, Chajès V, Hubert B, Lhuillery C, Le Floch O, Body G, Calais G. Cytotoxic drugs efficacy correlates with adipose tissue docosahexaenoic acid level in locally advanced breast carcinoma. Br J Cancer. 1999; 79:1765–1769.
Article90. Calviello G, Serini S, Piccioni E. N-3 polyunsaturated fatty acids and the prevention of colorectal cancer: molecular mechanisms involved. Curr Med Chem. 2007; 14:3059–3069.
Article91. Cavazos DA, Price RS, Apte SS, deGraffenried LA. Docosahexaenoic acid selectively induces human prostate cancer cell sensitivity to oxidative stress through modulation of NF-kappaB. Prostate. 2011; 71:1420–1428.
Article92. Fahrmann JF, Ballester OF, Ballester G, Witte TR, Salazar AJ, Kordusky B, Cowen KG, Ion G, Primerano DA, Boskovic G, Denvir J, Hardman WE. Inhibition of nuclear factor kappa B activation in early-stage chronic lymphocytic leukemia by omega-3 fatty acids. Cancer Invest. 2013; 31:24–38.
Article93. Ion G, Akinsete JA, Hardman WE. Maternal consumption of canola oil suppressed mammary gland tumorigenesis in C3(1) TAg mice offspring. BMC Cancer. 2010; 10:81.
Article94. Reddy BS. Studies with the azoxymethane-rat preclinical model for assessing colon tumor development and chemoprevention. Environ Mol Mutagen. 2004; 44:26–35.
Article95. Rose DP, Connolly JM, Rayburn J, Coleman M. Influence of diets containing eicosapentaenoic or docosahexaenoic acid on growth and metastasis of breast cancer cells in nude mice. J Natl Cancer Inst. 1995; 87:587–592.
Article96. Ross JA, Maingay JP, Fearon KC, Sangster K, Powell JJ. Eicosapentaenoic acid perturbs signalling via the NFkappaB transcriptional pathway in pancreatic tumour cells. Int J Oncol. 2003; 23:1733–1738.97. Sauer LA, Dauchy RT, Blask DE. Mechanism for the antitumor and anticachectic effects of n-3 fatty acids. Cancer Res. 2000; 60:5289–5295.98. United States Department of Agriculture (US). USDA Nutrient Database, walnut composition [Internet]. Washington, D.C.: United States Department of Agriculture;2011. cited 2014 March 14. Available from: http://ndb.nal.usda.gov/.99. Reiter RJ, Manchester LC, Tan DX. Melatonin in walnuts: influence on levels of melatonin and total antioxidant capacity of blood. Nutrition. 2005; 21:920–924.
Article100. McKay DL, Chen CY, Yeum KJ, Matthan NR, Lichtenstein AH, Blumberg JB. Chronic and acute effects of walnuts on antioxidant capacity and nutritional status in humans: a randomized, cross-over pilot study. Nutr J. 2010; 9:21.
Article101. Hardman WE, Ion G. Suppression of implanted MDA-MB 231 human breast cancer growth in nude mice by dietary walnut. Nutr Cancer. 2008; 60:666–674.
Article102. Hardman WE, Ion G, Akinsete JA, Witte TR. Dietary walnut suppressed mammary gland tumorigenesis in the C(3)1 TAg mouse. Nutr Cancer. 2011; 63:960–970.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Communicating clinical research to reduce cancer risk through diet: Walnuts as a case example
- Vegetable Diet in Cancer Prevention
- The Changes of Expression of Survivin by Butyrate in HCT116 Colon Cancer Cells
- Food, Nutrient, and the Risk of Breast Cancer
- Efficacy of monounsaturated fatty acids in reducing risk of the cardiovascular diseases, cancer, inflammation, and insulin resistance: a narrative review