Korean J Hematol.
2006 Dec;41(4):297-301. 10.5045/kjh.2006.41.4.297.
A Case of Limbic Encephalitis Developed after Allogeneic Stem Cell Transplantation
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Chungnam National University, Daejeon, Korea. deogyeon@cnu.ac.kr
- 2Department of Neurology, College of Medicine, Chungnam National University, Daejeon, Korea.
- 3Department of Radiology, College of Medicine, Chungnam National University, Daejeon, Korea.
- KMID: 2305217
- DOI: http://doi.org/10.5045/kjh.2006.41.4.297
Abstract
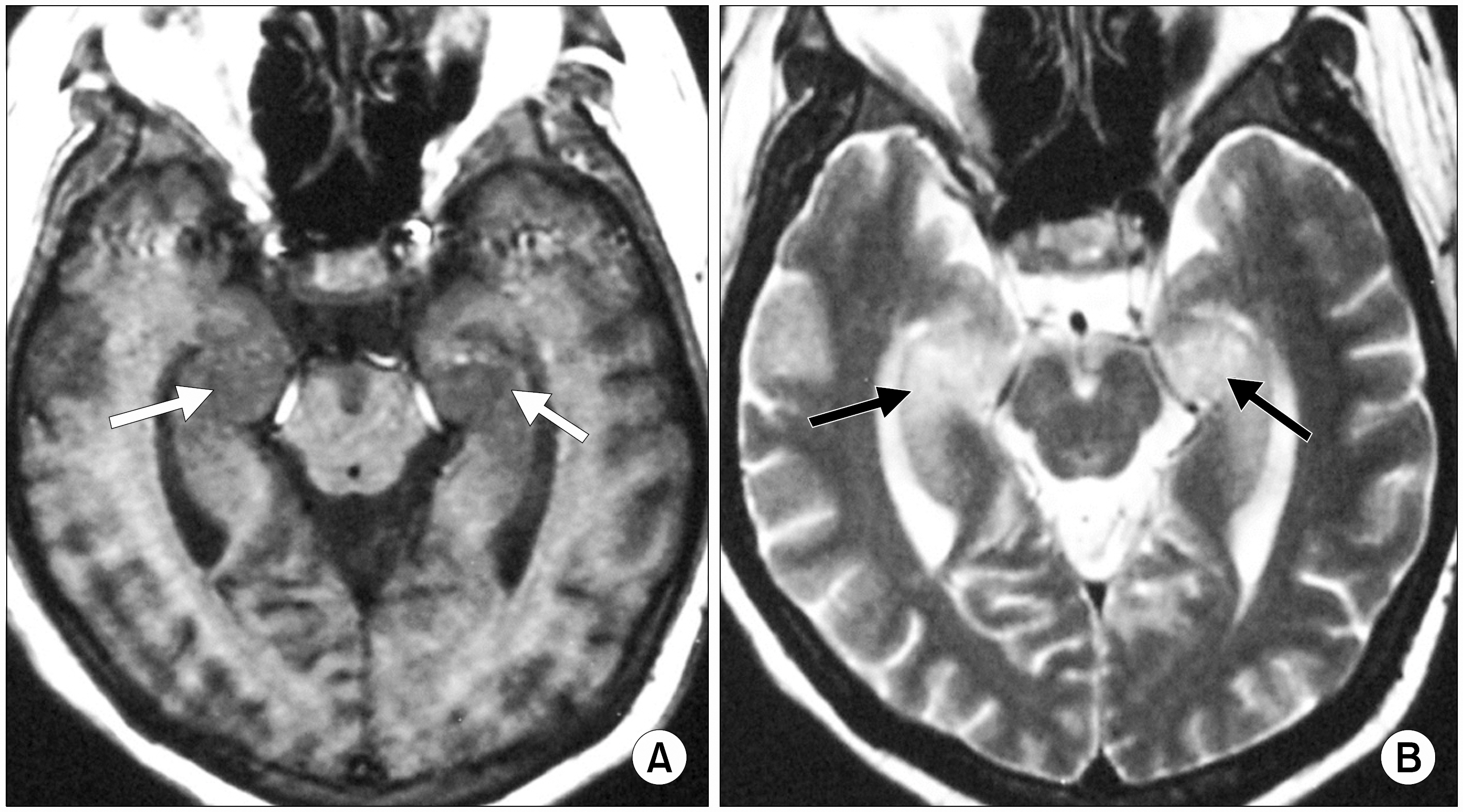
- Limbic encephalitis is a rare neurological syndrome, which develops after stem cell transplantation, and is characterized by a series of neurological symptoms, including retrograde amnesia, behavioral disturbance, and progressive intellectual deterioration and high signal intensity in the hippocampus on magnetic resonance imaging (MRI). Herein is described the case of a patient with limbic encephalitis, which developed after allogeneic bone marrow transplantation, and was possibly due to HHV-6 infection. An 18-year-old man, with acute lymphoid leukemia, who underwent HLA-matched unrelated donor bone marrow transplantation, developed a fever and chill accompanied by neurological symptoms, including behavioral disturbance and retrograde amnesia, during the bone marrow recovery phase. A brain MRI revealed bright signal-intensity in both hippocampi. Examination of his cerebrospinal fluid suggested viral encephalitis. Based on these findings, a diagnosis of viral limbic encephalitis was highly suspected. Tests for casual causes of viral limbic encephalitis, including the CMV, HZV and HSV-1 and 2, in serum or CSF were all negative. The encephalitis responded well to ganciclovir therapy.
MeSH Terms
-
Adolescent
Amnesia, Retrograde
Bone Marrow
Bone Marrow Transplantation
Brain
Cerebrospinal Fluid
Diagnosis
Encephalitis
Encephalitis, Viral
Fever
Ganciclovir
Herpesvirus 1, Human
Herpesvirus 6, Human
Hippocampus
Humans
Limbic Encephalitis*
Magnetic Resonance Imaging
Precursor Cell Lymphoblastic Leukemia-Lymphoma
Stem Cell Transplantation*
Stem Cells*
Unrelated Donors
Ganciclovir
Figure
Reference
-
1). Cakirer S. Paraneoplastic limbic encephalitis: case report. Comput Med Imaging Graph. 2002. 26:55–8.2). Voltz R. Paraneoplastic neurological syndrome: an update on diagnosis, pathogenesis and therapy. Lancet Neurol. 2002. 1:294–305.3). Gultekin SH., Rosenfeld MR., Voltz R., Eichen J., Posner JB., Dalmau J. Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients. Brain. 2000. 123:1481–94.
Article4). Tattevin P., Schortgen F., de Broucker T., Dautheville S., Wolff M. Varicella-zoster virus limbic encephalitis in an immunocompromised patient. Scand J Infect Dis. 2001. 33:786–8.
Article5). Wainwright MS., Martin PL., Morse RP, et al. Human herpesvirus 6 limbic encephalitis after stem cell transplantation. Ann Neurol. 2001. 50:612–9.
Article6). Yang DH., Lee JJ., Wi JO, et al. Tacrolimus-induced leukoencephalopathy invading limbic system after unrelated allogeneic bone marrow transplantation. Korean J Hemato Stem Cell Trans. 2004. 9:41–4. ..7). Ances BM., Vitaliani R., Taylor RA, et al. Treatment-responsive limbic encephalitis identified by neuropil antibodies: MRI and PET correlates. Brain. 2005. 128:1764–77.
Article8). Bien CG., Schulze-Bonhage A., Deckert M, et al. Limbic encephalitis not associated with neoplasm as a cause of temporal lobe epilepsy. Neurology. 2000. 55:1823–8.
Article9). Thuerl C., Muller K., Laubenberger J., Volk B., Langer M. MR imaging of autopsy-proved paraneoplastic limbic encephalitis in non-Hodgkin lymphoma. AJNR Am J Neuroradiol. 2003. 24:507–11.10). Yamanishi K., Okuno T., Shiraki K, et al. Identification of human herpesvirus-6 as a causal agent for exanthem subitum. Lancet. 1988. 1:1065–7.
Article11). Caserta MT., Mock DJ., Dewhurst S. Human herpesvirus 6. Clin Infect Dis. 2001. 33:829–33.
Article12). Cone RW., Huang ML., Corey L., Zeh J., Ashley R., Bowden R. Human herpesvirus 6 infections after bone marrow transplantation: clinical and virologic manifestations. J Infect Dis. 1999. 179:311–8.
Article13). Ogata M., Kikuchi H., Satou T, et al. Human herpesvirus 6 DNA in plasma after allogeneic stem cell transplantation: incidence and clinical significance. J Infect Dis. 2006. 193:68–79.
Article14). MacLean HJ., Douen AG. Severe amnesia associated with human herpesvirus-6 encephalitis after bone marrow transplantation. Transplantation. 2002. 73:1086–9.15). Yoshihara S., Kato R., Inoue T, et al. Successful treatment of life threatening human herpesvirus-6 encephalitis with donor lymphocyte infusion in a patient with had undergone human leukocyte antigen haploidentical nonmyeloablative stem cell transplantation. Transplantation. 2004. 77:835–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Limbic Encephalitis Caused by Human Herpesvirus-6 Infection in Allogenic Hematopoietic Stem Cell Transplantation Patient
- Long-term Neurological Complication of HHV-6 Encephalitis after Allogeneic Hematopoietic Stem Cell Transplantation
- Anti-Ma2-Associated Encephalitis with Axonal Sensorimotor Polyneuropathy
- Two Cases of Generalized Vitiligo after Allogeneic Stem Cell Transplantation
- A case of pneumomediastinum combined with chronic graft-versus-host disease following allogeneic hematopoietic stem cell transplantation