Korean Diabetes J.
2008 Oct;32(5):418-427. 10.4093/kdj.2008.32.5.418.
The Correlation Between Visceral Fat Distance Measured by Ultrasonography and Visceral Fat Amount by Computed Tomography in Type 2 Diabetes
- Affiliations
-
- 1Department of Internal Medicine, School of Medicine, Catholic University of Daegu, Korea.
- 2Department of Radiology, School of Medicine, Catholic University of Daegu, Korea.
- KMID: 2298080
- DOI: http://doi.org/10.4093/kdj.2008.32.5.418
Abstract
- BACKGROUND
Visceral adipose tissue accumulation highly correlates with metabolic abnormalities and cardiovascular disease. Computed tomography (CT) is considered to be the standard method for visceral fat evaluation, but it is not used as a routine procedure. Ultrasonography (US) is a safe method, fairly inexpensive and widely available modality for measuring abdominal fat thickness. The aim of this study was to investigate the correlation between the intra-abdominal fat distance by US measurement and the visceral fat amount by CT and cardiovascular risk factors and to evaluate whether the intra-abdominal fat distance is better correlate with visceral fat amount by CT than other anthropometric parameters and to assess the cut-off value of intra-abdominal fat distance for visceral obesity in type 2 diabetic patients.
METHODS
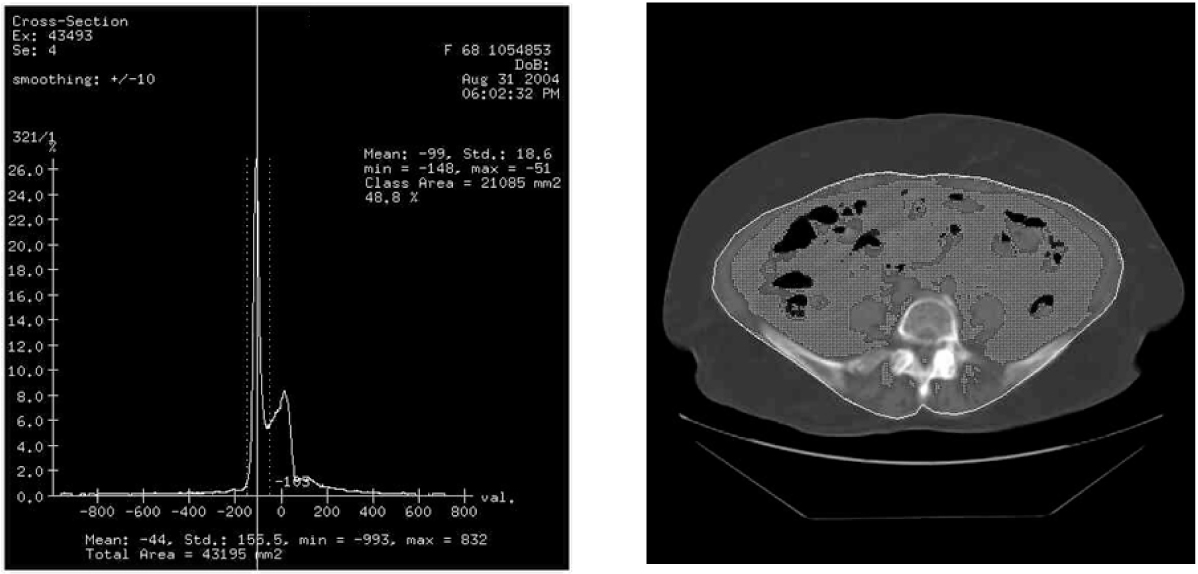
We obtained abdominal subcutaneous and intra-abdominal fat distance by using a high-resolution US (HDI 5000, ATL, Phillps, USA) at 1 cm above umbilical level in one hundred twenty-eight type 2 diabetic patients. CT scan (Light Speed plus, GE, USA) for the measurement of subcutaneous and intra-abdominal visceral fat area was also performed in the supine position at the L4-5 level. Lean body mass and % body fat were measured in a bioimpedance using DSM (Direct Segmental Measurement by 8-point electrode) method (InBody 3.0, Biospace, Seoul, Korea). We measured patient's height, weight, BMI (Body mass index), waist circumference, WHR(Waist-hip ratio) and blood pressure and also measured fasting blood glucose, HbA1c and lipid profiles.
RESULTS
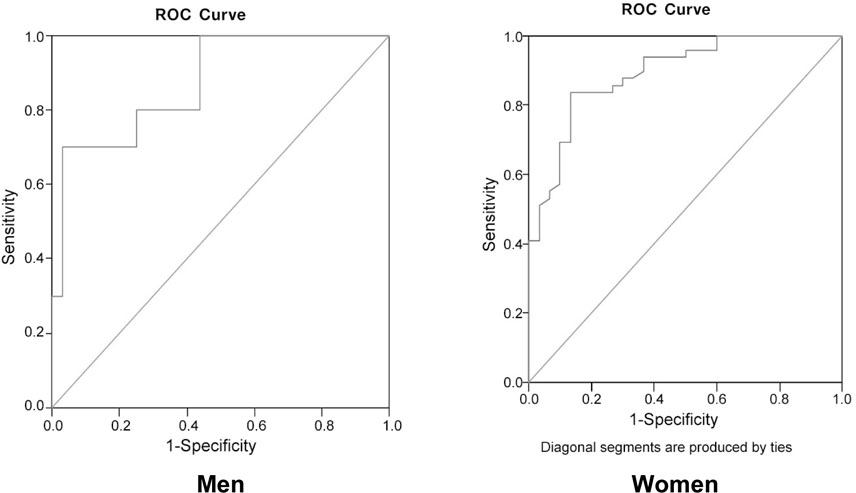
Abdominal subcutaneous and visceral fat distance measured by US is 2.05 +/- 0.52 cm, 4.43 +/- 1.54 cm, respectively. In pearson's correlations, visceral fat distance were correlated with BMI (r = 0.681, P < 0.001), waist circumference (r = 0.661, P < 0.001), WHR (r = 0.571, P < 0.001), triglyceride (r = 0.316, P < 0.001), HDL-cholesterol (r = -0.207, P < 0.004). US-determined visceral fat distance was also correlated with visceral fat amount by CT (r = 0.674, P < 0.001) and BMI (r = 0.610, P < 0.001), waist circumference (r = 0.626, P < 0.001), WHR (r = 0.557, P < 0.001). When we used waist circumference (men: 90 cm, women: 85 cm) as parameters for visceral obesity, the cutoff value of visceral fat distance, obtained by the receiver operating characteristic curve analysis, were 4.670 cm in men, 3.695 cm in women diabetic patients.
CONCLUSION
Intra-abdominal fat distance measured by US reveals strongly correlated with visceral fat area, which is determined by CT and also well correlated with anthropometric parameters and lipid profiles. We suggest that US provided a better index compared to anthropometry for the prediction of visceral obesity and could be an alternative method for CT for visceral fat determination in diabetic patients.
MeSH Terms
Figure
Reference
-
1. Fujioka S, Matsuzawa Y, Tokunaga K, Tauri S. Contribution of intraabdominal fat accumulation to the impairment of glucose and lipid metabolism in human obesity. Metabolism. 1987. 36:54–59.2. Kim SK, Kim HJ, Hur KY, Choi SH, Ahn CW, Lim SK, Kim KR, Lee HC, Huh KB, Cha BS. Visceral fat thickness measured by ultrasonography can estimate not only visceral obesity but also risks of cardiovascular and metabolic disease. Am J Clin Nutr. 2004. 79:593–599.3. Bjorntorp P. Portal adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis. 1990. 10:493–496.4. Guldiken S, Tuncbilek N, Okten OO, Arikan E, Tugrul A. Visceral fat thickness determined using ultrasonography is associated with anthropometric and clinical parameters of metabolic syndrome. Int J Clin Pract. 2006. 60:1576–1581.5. Leite CC, Wajchenberg BL, Radominski R, Matsuda D, Cerri GG, Halpern A. Intra-abdominal thickness by ultrasonography to predict risk factors for cardiovascular disease and its correlation with anthropometric measurements. Metabolism. 2002. 51:1034–1040.6. Zamboni M, Armellini F, Sheiban F, De Marchi M, Todesco T, Bergamo Andreis IA, Cominacini L, Bosello O. Relation of body fat distribution in men and degree of coronary narrowings in coronary artery disease. Am J Cardiol. 1992. 70:1135–1138.7. Armellini F, Zamboni M, Robbi R, Todesco T, Rigo L, Bergami-Andreis IA, Bosello O. Total and intra-abdominal fat measurements by ultrasound and computerized tomography. Int J Obes Relat Metab Disord. 1993. 17:209–214.8. Kim SK, Kim SH, Rhee YM, Choi SH, Cho YL, Ahn CW, Cha BS, Lim SK, Kim KR, Lee HC, Huh KB. The comparison of intra-abdominal fat distance (I-A Fat Distance) and visceral adipose tissue area (VAT) or visceral fat to skeletal muscle are ratio (VMR) measured by computed tomography (CT). Korean J Med. 2003. 64:49–59.9. Hirooka M, Kumagi T, Kurose K, Nakanishi S, Michitaka K, Matsuura B, Horike N, Onji M. A technique for the measurement of visceral fat by ultrasonography: Comparision of measurements by ultrasonography and computed tomography. Internal Medicine. 2005. 44:794–799.10. Depres JP, Prud'Homme D, Pouliot MC, Tremblay A, Bouchard C. Estimation of deep abdominal adipose-tissue accumulation from simple anthropometric measurements in men. Am J Clin Nutr. 1991. 54:471–477.11. Seidell JC, Cigolini M, Charzewska J, Ellisinger BM, Deslypere JP, Cruz A. Fat distribution in European men: a comparision of anthropometric measurements in relation to cardiovascular risk factors. Int J Obes Relat Metab Disord. 1992. 16:17–22.12. Ross R, Rissanen J, Hudson R. Sensitivity associated with the identification of visceral adipose tissue levels using waist circumference in men and women: Effects of weight loss. Int J Obes Relat Metab Disord. 1996. 20:533–538.13. Seidell JC, Andres R, Sorkin JD, Muller DC. The sagittal waist diameter and mortality in men: The Baltimore Longitudinal Study on aging. Int J Obes Relat Metab Disord. 1994. 18:61–67.14. Ribeiro-Filho FF, Faria AN, Kohlmann O Jr, Ajzen S, Ribeiro AB, Zanella MT, Ferreira SRG. Ultrasonography for the evaluation of visceral fat and cardiovascular risk. Hypertension. 2001. 38:713–717.15. Tomaghi G, Raiteri R, Pozzato C, Rispoli A, Bramani M, Cipolat M, Craveri A. Anthropometric or ultrasonic measurements in assessment of visceral fat?: a comparative study. Int J Obes Relat Metab Disord. 1994. 18:771–775.16. Ribeiro-Filho FF, Faria AN, Azjen S, Zanella MT, Ferreira SRG. Methods of estimation of visceral fat: Advantages of ultrasonography. Obes Res. 2003. 11:1488–1494.17. Liu KH, Chan YL, Chan WB, Kong WL, Kong MO, Chan JCN. Sonographic measurement of mesenteric fat thickness is a good correlate with cardiovascular risk factors: comparison with subcutaneous and preperitoneal fat thickness, magnetic resonance imaging and anthropometric indexes. Int J Obes Relat Metab Disord. 2003. 27:1267–1273.18. Armellini F, Zamboni M, Rigo L, Todesco T, Bergamo-Andris IA, Procacci C, Bosello O. The contribution of sonography to the measurement of intra-abdominal fat. J Clin Ultrasound. 1990. 18:563–567.19. Armellini F, Zamboni M, Rigo L, Bergamo-Andreis IA, Robbi R, De Marchi M, Bosello O. Sonography detection of small intra-abdominal fat variations. Int J Obe. 1991. 15:847–852.20. Jeong GH, Kim SK, Chung JO, Cho DH, Chung DJ, Chung MY. Association between ultrasonographic visceral fat indices and cardiovascular risk factors in type 2 diabetic patients. Korean J Med. 2007. 73:618–630.21. Rebuffe-Scrive M, Anderson B, Olbe L, Bjorntorp P. Metabolism of adipose tissue in intra abdominal depots of non obese men and women. Metabolism. 1989. 38:453–458.22. Bjorntorp P. Portal adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis. 1990. 10:493–496.23. Ahima RS, Jeffery SF. Adipose tissue as an endocrine organ. Trends Endocrinol Metab. 2000. 11:327–332.24. Choi SH, Kim DJ, Lee KE, Kim YM, Song YD, Kim HD, Ahn CW, Cha BS, Huh KB, Lee HC. Cut-off Value of Waist Circumference for Metabolic Syndrome Patients in Korean Adult Population. Korean J Obes. 2004. 13:53–60.25. Kim JA, Choi CJ, Yum KS. Cut-off values of visceral fat area and waist circumference: Diagnostic criteria for abdominal obesity in a Korean population. J Korean Med Sci. 2006. 21:1048–1053.26. Lee HJ, Kwon HS, Park YM, Chun HN, Choi YH, Ko SH, Lee JM, Yoon KH, Cha BY, Lee WC, Lee KW, Son HY, Kang SK, Ahn MS, Kang JM, Kim DS. Waist circumference as s risk factor for metabolic syndrome in Korean adult: Evaluation from 5 different criteria of metabolic syndrome. J Kor Diabetes Assoc. 2005. 29:48–56.27. Lee S, Park HS, Kim SM, Kwon HS, Kim DY, Kim DJ, Cho GJ, Han JH, Kim SR, Park CY, Oh SJ, Lee CB, Kim KS, Oh SW, Kim YS, Choi WH, Yoo HJ. Cut-off Points of Waist Circumference for Defining Abdominal Obesity in the Korean Population. Korean J Obes. 2006. 15:1–9.28. Examination Committee of Criteria for 'Obesity Disease' in Japan. Japan Society for the Study of Obesity. New criteria for 'obesity disease' in Japan. Circ J. 2002. 66:987–992.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Correlation between the Triglyceride to High Density Lipoprotein Cholesterol Ratio and Computed Tomography-Measured Visceral Fat and Cardiovascular Disease Risk Factors in Local Adult Male Subjects
- Comparison of DEXA and CT for Truncal Obesity in Adult Women Related to Metabolic Complications
- The correlation between simple anthropometric indices and abdominal visceral fat accumulation by computed tomography
- Relationship of Metabolic Syndrome and Truncal Obesity Measured by Dual Energy X-ray Absorptiometry and Computed Tomography in Obese Women
- The comparison of intra-abdominal fat distance (I-A Fat Distance) and visceral adipose tissue area (VAT) or visceral fat to skeletal muscle area ratio (VMR) measured by computed tomography (CT)