J Rheum Dis.
2014 Jun;21(3):147-150. 10.4078/jrd.2014.21.3.147.
Muscle Weakness in a Patient with History of Poliomyelitis: A Differential Diagnosis for Post-polio Syndrome (PPS) and Dermatomyositis
- Affiliations
-
- 1Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea. shlee@kuh.ac.kr
- KMID: 2297527
- DOI: http://doi.org/10.4078/jrd.2014.21.3.147
Abstract
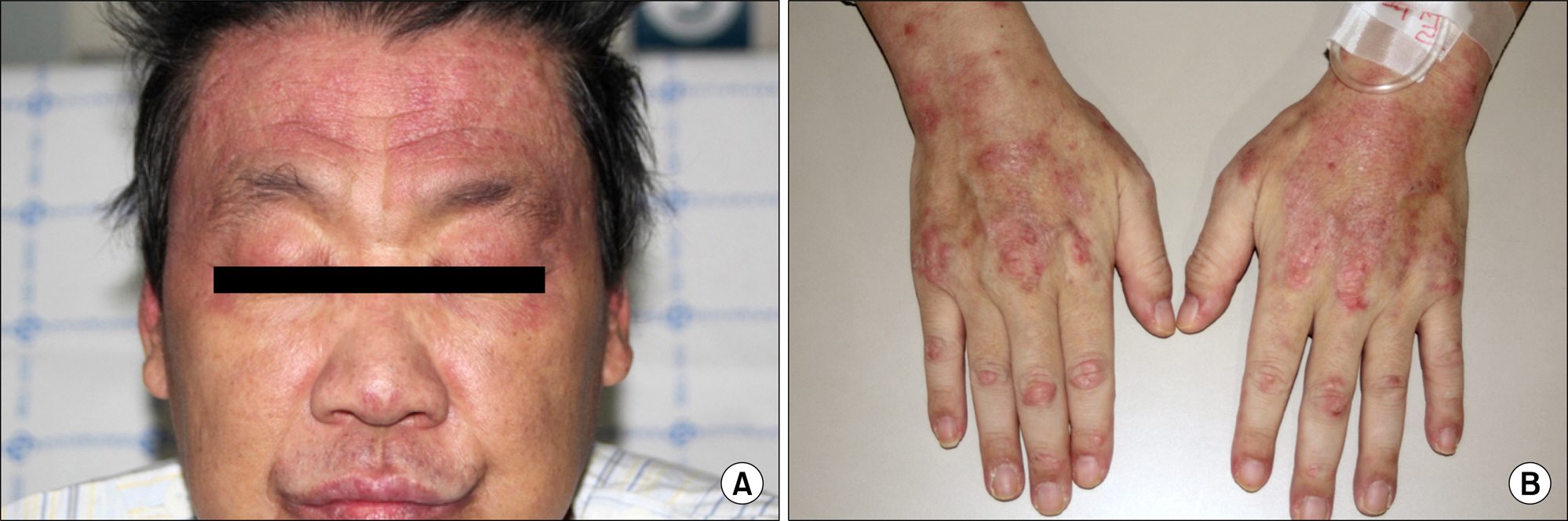
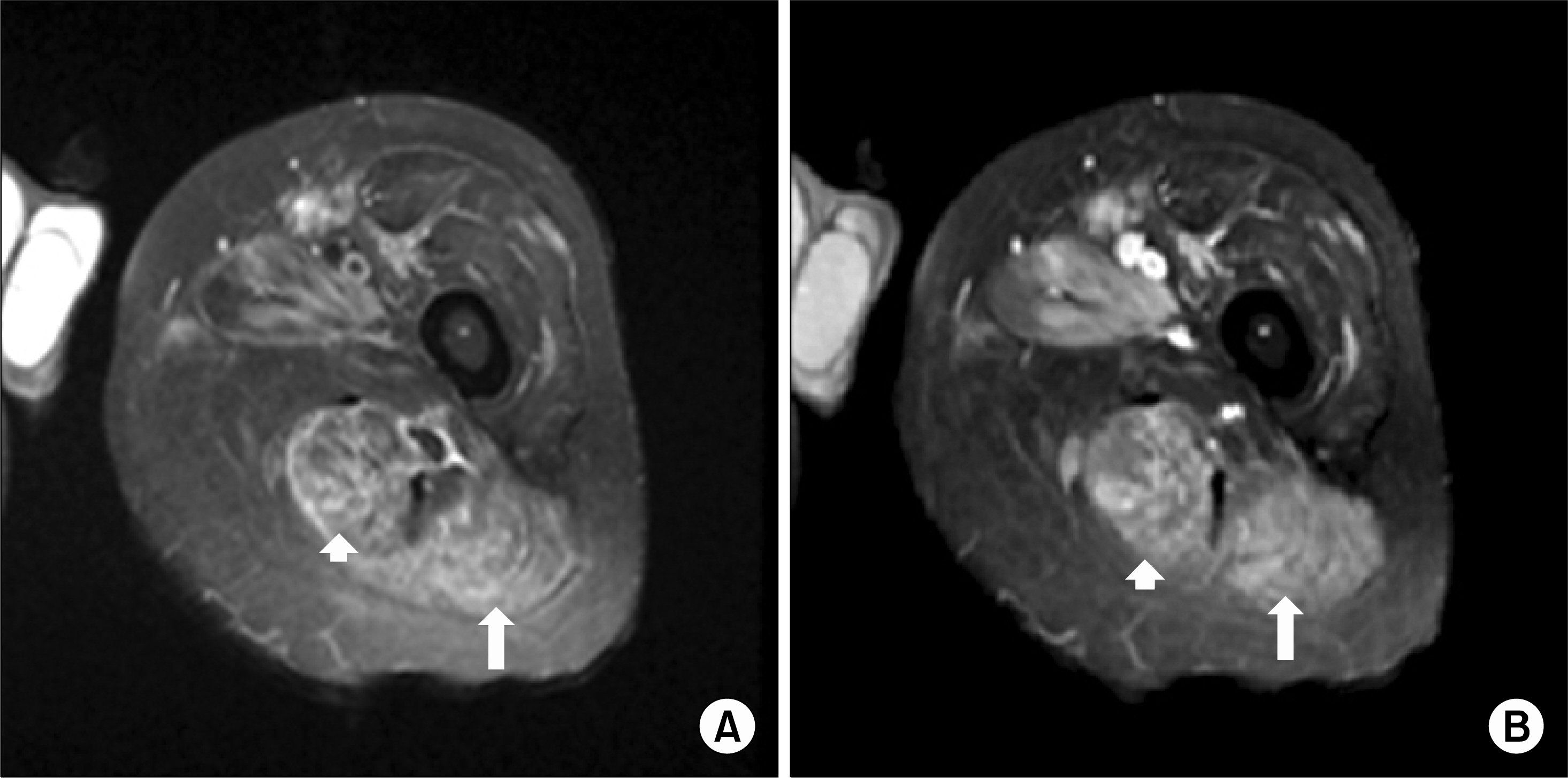
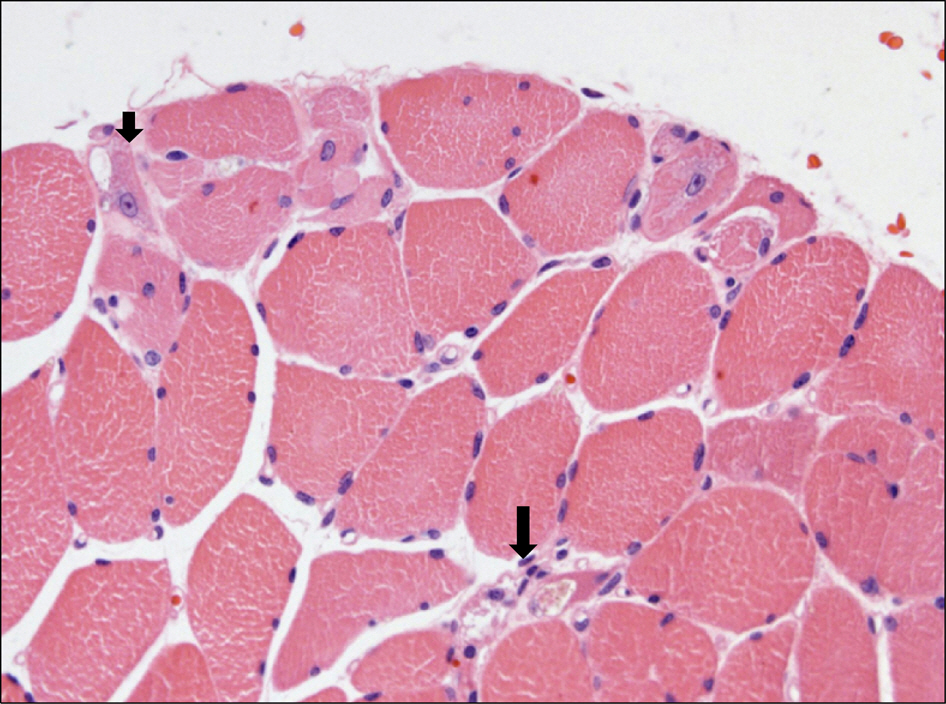
- Dermatomyositis (DM) is an idiopathic inflammatory myopathy, characterized by inflammation of the proximal skeletal muscles and typical skin manifestations, which results in symmetric muscle weakness. A 43-year-old man was presented with skin rash and left leg weakness, and he had a history of poliomyelitis. Initially, he was diagnosed as having post-polio syndrome (PPS) due to unilateral muscle weakness and a result of an the electromyography (EMG), which had shown patterns of PPS. After 4 months with conservative therapy for PPS, weakness of bilateral upper arms had developed and skin rashes on his entire body had aggravated and progressed. He was diagnosed as having dermatomyositis, based on elevated muscle enzyme levels, typical skin rashes, and typical EMG findings, which indicated muscle disease. When a patient with previous poliomyelitis has a newly developed muscle weakness or pain, we should consider various possible causes other than PPS.
MeSH Terms
Figure
Reference
-
1. Zong M, Lundberg IE. Pathogenesis, classification and treatment of inflammatory myopathies. Nat Rev Rheumatol. 2017; 297–306.
Article2. Chung JH, Seo PG. Clinical manifestations of dermatomyositis. Korean J Dermatol. 2002; 40:258–65.3. Bohan A, Peter JB. Polymyositis and dermatomyositis (second of two parts). N Engl J Med. 1975; 292:403–7.4. Gonzalez H, Olsson T, Borg K. Management of postpolio syndrome. Lancet Neurol. 2010; 9:634–42.
Article5. Miller FW. Polymyositis and dermatomyositis. Goldman L, Andrew IS, editors. Goldman's Cecil medicine. 24th ed.p. 1716–20. Philadelphia: Saunders Elsevier;2012.
Article6. Trojan DA, Cashman NR. Post-poliomyelitis syndrome. Muscle Nerve. 2005; 31:6–19.
Article7. Jubelt B, Agre JC. Characteristics and management of postpolio syndrome. JAMA. 2000; 284:412–4.
Article8. Dalakas MC. Polymyositis, dermatomyositis and in-clusion-body myositis. N Engl J Med. 1991; 325:1487–98.
Article9. Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet. 2003; 362:971–82.
Article10. Barkhaus PE, Nandedkar SD, Sanders DB. Quantitative EMG in inflammatory myopathy. Muscle Nerve. 1990; 13:247–53.
Article11. Parissis D, Karkavelas G, Taskos N, Milonas I. Inclusion body myositis in a patient with a presumed diagnosis of postpolio syndrome. J Neurol. 2003; 250:619–21.
Article