J Korean Acad Conserv Dent.
2010 May;35(3):222-228. 10.5395/JKACD.2010.35.3.222.
The effect of several root-end filling materials on MG63 osteoblast-like cells
- Affiliations
-
- 1Department of Conservative Dentistry, Dental Hospital, East-West Neomedical Center, Seoul, Korea.
- 2Department of Conservative dentistry, School of Dentistry, Seoul National University, Seoul, Korea. shbaek@snu.ac.kr
- KMID: 2294348
- DOI: http://doi.org/10.5395/JKACD.2010.35.3.222
Abstract
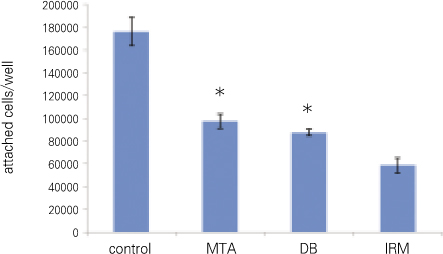
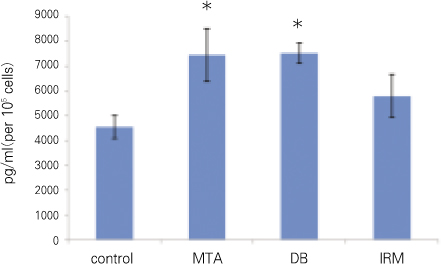
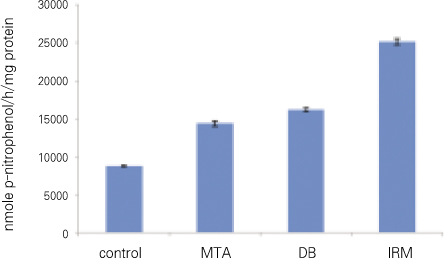
- The purpose of this study was to compare mineral trioxide aggregate (MTA; Dentsply, Tulsa Dental, Tulsa, OK, USA), which is widely used as root-end filling material, with DiaRoot BioAggregate (DB; Innovative BioCaramix Inc, Vancouver, BC, Canada), newly developed product, by using MG63 osteoblast-like cells. MTA, DB, and Intermediate Restorative Material (IRM; Dentsply Caulk, Milford, DE, USA) were used for root-end filling material while tissue culture plastic was used for control group. Each material was mixed and, the mixtures were left to set for 24 hours. MG63 cells were seeded to each group and then they were cultured for attachment for 4 hours. Following the attachment of cells to the root-end filling material, early cellular response was observed. After another 12 hours'culture, the level of attachment between cells and material was observed and in order to identify the effect of each material to bone formation, transforming growth factor beta1 (TGFbeta1) and osteocalin (OC) were estimated by using enzyme-linked immunosorbent assay (ELISA), and the amount of alkaline phosphatase (ALP) was also measured. The data were analyzed using one-way ANOVA. As a result, only at OC and the number of cells which were attached to materials, there was no statistical difference between MTA and DB. At other items, there was statistically significant difference in all groups. Although DB has not shown exactly the same cellular response like that of MTA, the number of attached cells shows that biocompatibility of the material and OC indicates bone formation rate. Therefore, if DB is used for root end filling material, it is expected to lead to similar results to MTA.
Keyword
MeSH Terms
-
Alkaline Phosphatase
Aluminum Compounds
Calcium Compounds
Calcium Hydroxide
Drug Combinations
Enzyme-Linked Immunosorbent Assay
Glutamates
Guanine
Hydroxyapatites
Osteogenesis
Oxides
Plastics
Polymethyl Methacrylate
Seeds
Silicates
Transforming Growth Factor beta1
Pemetrexed
Alkaline Phosphatase
Aluminum Compounds
Calcium Compounds
Calcium Hydroxide
Drug Combinations
Glutamates
Guanine
Hydroxyapatites
Oxides
Plastics
Polymethyl Methacrylate
Silicates
Transforming Growth Factor beta1
Figure
Cited by 2 articles
-
Biocompatibility of root-end filling materials: recent update
Payal Saxena, Saurabh Kumar Gupta, Vilas Newaskar
Restor Dent Endod. 2013;38(3):119-127. doi: 10.5395/rde.2013.38.3.119.Comparative analysis of physicochemical properties of root perforation sealer materials
Maura Cristiane Gonçales Orçati Dorileo, Fábio Luis Miranda Pedro, Matheus Coelho Bandeca, Orlando Aguirre Guedes, Ricardo Dalla Villa, Alvaro Henrique Borges
Restor Dent Endod. 2014;39(3):201-209. doi: 10.5395/rde.2014.39.3.201.
Reference
-
1. Torabinejad M, Chivian N. Clinical applications of mineral trioxide ag gregate. J Endod. 1999. 25:197–205.2. Yun YR, Yang IS, Hwang YC, Hwang IN, Choi HR, Yoon SJ, Kim SH, Oh WM. Pulp response of mineral trioxide aggregate, calcium sulfate or calcium hydroxide. J Korean Acad Conserv Dent. 2007. 32:95–101.
Article3. Schmitt D, Lee J, Bogen G. Multifaceted use of ProRoot MTA root canal repair material. Pediatr Dent. 2001. 23:326–330.4. Koh ET, Torabinejad M, Pitt Ford TR, Brady K, McDonald F. Mineral trioxide aggregate stimulates a biological response in human osteoblasts. J Biomed Mater Res. 1997. 37:432–439.
Article5. Koh ET, McDonald F, Pitt Ford TR, Torabinejad M. Cellular response to mineral trioxide aggregate. J Endod. 1998. 24:543–547.
Article6. Mitchell PJC, Pitt Ford TR, Torabinejad M, McDonald F. Osteoblast biocompatibility of mineral trioxide aggregate. Biomaterials. 1999. 20:167–173.
Article7. Rausch-fan X, Qu Z, Wieland M, Matejka M, Schedle A. Differentiation and cytokine synthesis of human alveolar osteoblasts compared to osteoblast-like cells(MG63) in response to titanium surfaces. Dent Mater. 2008. 24:102–110.
Article8. Qu Z, Rausch-fan X, Wieland M, Matejka M, schedle A. The initial attachment and subsequent behavior regulation of osteoblasts by dental implant surface modification. J Biomed Mater Res A. 2007. 82:658–668.
Article9. Perez AL, Spears R, Gutmann JL, Opperman LA. Osteoblasts and MG-63 osteosarcoma cells behave differently when in contact with ProRoot MTA and white MTA. Int Endod J. 2003. 36:564–570.
Article10. Schmalz G. Use of cell cultures for toxicity testing of dental materials - advantages and limitations. J Dent. 1994. 22:suppl 2. S6–S11.11. Kang MK, Bae IH, Koh JT, Hwang YC, Hwang IN, Oh WM. Comparison of biocompatibility of four root perforation repair materials. J Korean Acad Conserv Dent. 2009. 34:192–198.
Article12. Calvo MS, Eyre DR, Gundberg CM. Molecular basis and clinical application of biological markers of bone turnover. Endocr Rev. 1996. 17:333–368.
Article13. Kassem M, Kveiborg M, Eriksen EF. Production and action of transforming growth factor-β in human osteoblast cultures: dependence on cell differentiation and modulation by calcitriol. Eur J Clin Invest. 2000. 30:429–437.
Article14. Diadent group international. Material safety data sheet DiaRoot bioAggregate. 2007.15. De-Deus G, Canabarro A, Alves G, Linhares A, Senne MI, Granjeiro JM. Optimal cytocompatibility of a bioceramic nanoparticulate cement in primary human mesenchymal cells. J Endod. 2009. 35:1387–1390.
Article16. Zhang H, Pappen FG, Haapasalo M. Dentin enhances the antibacterial effect of mineral trioxide aggregate and bioaggregate. J Endod. 2009. 35:221–224.
Article17. Apaydin ES, Shabahang S, Torabinejad M. Hard-tissue healing after application of fresh or set MTA as root-end-filling material. J Endod. 2004. 30:21–24.
Article18. AL-Rabeah E, Perinpanayagam H, MacFarland D. Human alveolar bone cells interact with ProRoot and tooth-colored MTA. J Endod. 2006. 32:872–875.
Article19. Zhu Q, Haglund R, Safavi KE, Spangberg LSW. Adhesion of human osteoblasts on root-end filling materials. J Endod. 2000. 26:404–406.
Article20. Bender MedSystems GmbH. BMS2020INST human osteocalcin. 2006.21. Thomson TS, Berry JE, Somerman MJ, Kirkwood KL. Cementoblasts maintain expression of osteocalcin in the presence of mineral trioxide aggregate. J Endod. 2003. 29:407–412.
Article22. Cassidy N, Fahey M, Prime SS, Smith AJ. Comparative analysis of transforming growth factor-β isoforms 1-3 in human and rabbit dentine matrices. Arch Oral Biol. 1997. 42:219–223.
Article23. Sakai R, Eto Y. Involvement of activin in the regulation of bone metabolism. Mol Cell Endocrinol. 2001. 180:183–188.
Article24. Kwon JY, Lim SS, Baek SH, Bae KS, Kang MH, Lee WC. The effect of mineral trioxide aggregate on the production of growth factors and cytokine by human periodontal ligament fibroblasts. J Korean Acad Conserv Dent. 2007. 32:191–197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biocompatibility of root-end filling materials: recent update
- Effect of titanium surface roughness on cell adhesion of human osteoblast-like cells (MG63)
- Effects of nicotine on the formation of osteocalcin and osteoprotegerin and synthesis of its mRNA in MG63 osteoblast-like cell
- Spectrophotometric evaluation of sealing effects of several root-end filling materials
- A comparative study on radiopacity of canal filling and retrograde root-end filling materials