J Gynecol Oncol.
2013 Jul;24(3):222-228. 10.3802/jgo.2013.24.3.222.
Multivariate prognostic analysis of adenocarcinoma of the uterine cervix treated with radical hysterectomy and systematic lymphadenectomy
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Hokkaido University Graduate School of Medicine, Sapporo, Japan. watarih@med.hokudai.ac.jp
- KMID: 2288528
- DOI: http://doi.org/10.3802/jgo.2013.24.3.222
Abstract
OBJECTIVE
The aim of this study was to investigate the prognostic factors and treatment outcome of patients with adenocarcinoma of the uterine cervix who underwent radical hysterectomy with systematic lymphadenectomy.
METHODS
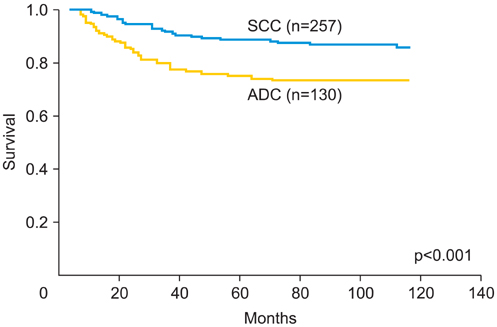
A total of 130 patients with stage IB to IIB cervical adenocarcinoma treated with hysterectomy and systematic lymphadenectomy from 1982 to 2005 were retrospectively analyzed. Clinicopathological data including age, stage, tumor size, the number of positive node sites, lymphovascular space invasion, parametrial invasion, deep stromal invasion (>2/3 thickness), corpus invasion, vaginal infiltration, and ovarian metastasis, adjuvant therapy, and survival were collected and Cox regression analysis was used to determine independent prognostic factors.
RESULTS
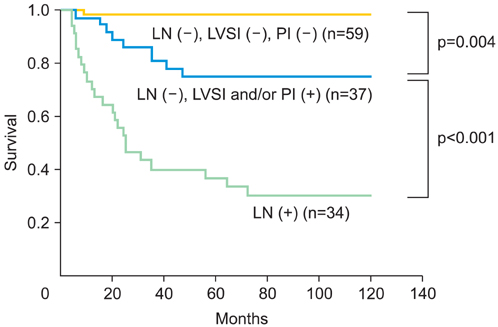
An estimated five-year survival rate of stage IB1 was 96.6%, 75.0% in stage IB2, 100% in stage IIA, and 52.8% in stage IIB. Prognosis of patients with one positive-node site is similar to that of those with negative-node. Prognosis of patients with multiple positive-node sites was significantly poorer than that of negative and one positive-node site. Multivariate analysis revealed that lymph node metastasis, lymphovascular space invasion, and parametrial invasion were independent prognostic factors for cervical adenocarcinoma. Survival of patients with cervical adenocarcinoma was stratified into three groups by the combination of three independent prognostic factors.
CONCLUSION
Lymph node metastasis, lymphovascular space invasion, and parametrial invasion were shown to be independent prognostic factors for cervical adenocarcinoma treated with hysterectomy and systematic lymphadenectomy.
MeSH Terms
Figure
Reference
-
1. Schorge JO, Knowles LM, Lea JS. Adenocarcinoma of the cervix. Curr Treat Options Oncol. 2004; 5:119–127.2. Look KY, Brunetto VL, Clarke-Pearson DL, Averette HE, Major FJ, Alvarez RD, et al. An analysis of cell type in patients with surgically staged stage IB carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol. 1996; 63:304–311.3. Eifel PJ, Burke TW, Morris M, Smith TL. Adenocarcinoma as an independent risk factor for disease recurrence in patients with stage IB cervical carcinoma. Gynecol Oncol. 1995; 59:38–44.4. Brand E, Berek JS, Hacker NF. Controversies in the management of cervical carcinoma. Obstet Gynecol. 1988; 71:261–269.5. Goodman HM, Buttlar CA, Niloff JM, Welch WR, Marck A, Feuer EJ, et al. Adenocarcinoma of the uterine cervix: prognostic factors and patterns of recurrence. Gynecol Oncol. 1989; 33:241–247.6. Lai CH, Hsueh S, Hong JH, Chang TC, Tseng CJ, Chou HH, et al. Are adenocarcinomas and adenosquamous carcinomas different from squamous carcinomas in stage IB and II cervical cancer patients undergoing primary radical surgery? Int J Gynecol Cancer. 1999; 9:28–36.7. Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet. 1997; 350:535–540.8. Kim SM, Choi HS, Byun JS. Overall 5-year survival rate and prognostic factors in patients with stage IB and IIA cervical cancer treated by radical hysterectomy and pelvic lymph node dissection. Int J Gynecol Cancer. 2000; 10:305–312.9. Nakanishi T, Ishikawa H, Suzuki Y, Inoue T, Nakamura S, Kuzuya K. A comparison of prognoses of pathologic stage Ib adenocarcinoma and squamous cell carcinoma of the uterine cervix. Gynecol Oncol. 2000; 79:289–293.10. Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Outcomes after radical hysterectomy in patients with early-stage adenocarcinoma of uterine cervix. Br J Cancer. 2010; 102:1692–1698.11. Grisaru D, Covens A, Chapman B, Shaw P, Colgan T, Murphy J, et al. Does histology influence prognosis in patients with early-stage cervical carcinoma? Cancer. 2001; 92:2999–3004.12. Ayhan A, Al RA, Baykal C, Demirtas E, Yuce K, Ayhan A. A comparison of prognoses of FIGO stage IB adenocarcinoma and squamous cell carcinoma. Int J Gynecol Cancer. 2004; 14:279–285.13. Lee KB, Lee JM, Park CY, Lee KB, Cho HY, Ha SY. What is the difference between squamous cell carcinoma and adenocarcinoma of the cervix? A matched case-control study. Int J Gynecol Cancer. 2006; 16:1569–1573.14. Fregnani JH, Soares FA, Novik PR, Lopes A, Latorre MR. Comparison of biological behavior between early-stage adenocarcinoma and squamous cell carcinoma of the uterine cervix. Eur J Obstet Gynecol Reprod Biol. 2008; 136:215–223.15. Kasamatsu T, Onda T, Sawada M, Kato T, Ikeda S, Sasajima Y, et al. Radical hysterectomy for FIGO stage I-IIB adenocarcinoma of the uterine cervix. Br J Cancer. 2009; 100:1400–1405.16. Hosaka M, Watari H, Takeda M, Moriwaki M, Hara Y, Todo Y, et al. Adjuvant chemotherapy versus adjuvant radiotherapy after radical hysterectomy for patients with cervical squamous cell carcinoma. J Obstet Gynaecol Res. 2008; 34:552–556.17. Watari H, Kanuma T, Ohta Y, Hassan MK, Mitamura T, Hosaka M, et al. Clusterin expression inversely correlates with chemosensitivity an predicts poor survival in patients with locally advanced cervical cancer treated with cisplatin-based neoadjuvant chemotherapy and radical hysterectomy. Pathol Oncol Res. 2010; 16:345–352.18. Takeda N, Sakuragi N, Takeda M, Okamoto K, Kuwabara M, Negishi H, et al. Multivariate analysis of histopathologic prognostic factors for invasive cervical cancer treated with radical hysterectomy and systematic retroperitoneal lymphadenectomy. Acta Obstet Gynecol Scand. 2002; 81:1144–1151.19. Watari H, Todo Y, Takeda M, Ebina Y, Yamamoto R, Sakuragi N. Lymph-vascular space invasion and number of positive paraaortic node groups predict survival in node-positive patients with endometrial cancer. Gynecol Oncol. 2005; 96:651–657.20. Takeda M, Sakuragi N, Okamoto K, Todo Y, Minobe S, Nomura E, et al. Preoperative serum SCC, CA125, and CA19-9 levels and lymph node status in squamous cell carcinoma of the uterine cervix. Acta Obstet Gynecol Scand. 2002; 81:451–457.21. Kim SK, Choi HJ, Park SY, Lee HY, Seo SS, Yoo CW, et al. Additional value of MRI/PET fusion vompared with PET-CT in the detection of lymph node metastasis in cervical cancer patients. Eur J Cancer. 2009; 45:2103–2109.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinicopathologic characteristics and prognostic factors in adenocarcinoma of the uterine cervix
- The relationship between positive peritoneal cytology and the prognosis of patients with FIGO stage I/II uterine cervical cancer
- A case of massive serous ascites following radical hysterectomy with bilateral pelvic lymphadenectomy for cervical adenocarcinoma stage IB2
- Comparison of prognosis of FIGO stage IB 1 adenocarcinoma and squamous cell carcinoma who were treated primarily by surgery
- Comparisons of clinicopathologic characteristics and prognostic factors between squamous cell carcinoma and adenocarcinoma of the uterine cervical cancer patients underwent radical hysterectomy and pelvic lymphadenectomy