Korean J Gynecol Oncol.
2008 Mar;19(1):93-98. 10.3802/kjgo.2008.19.1.93.
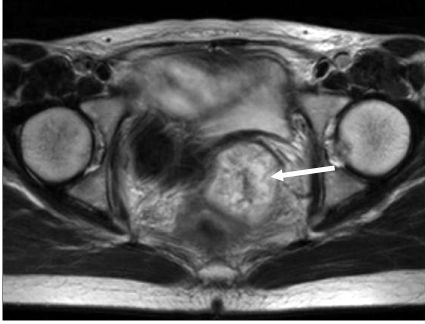
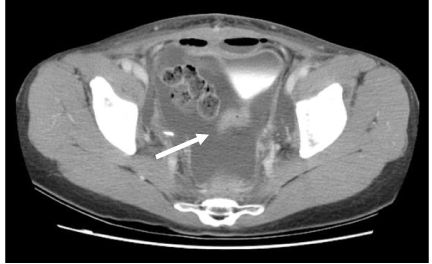
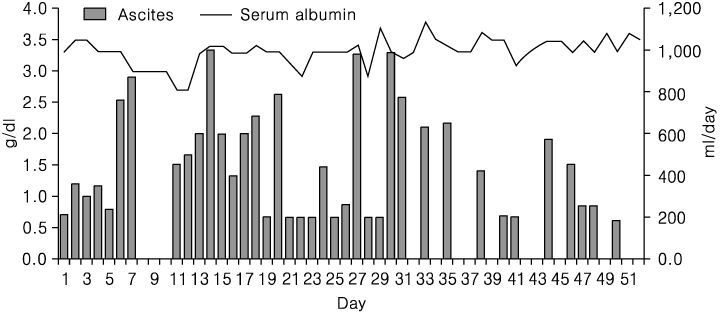
A case of massive serous ascites following radical hysterectomy with bilateral pelvic lymphadenectomy for cervical adenocarcinoma stage IB2
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kyungpook National University School of Medicine, Daegu, Korea. ylcho@mail.knu.ac.kr
- KMID: 1979507
- DOI: http://doi.org/10.3802/kjgo.2008.19.1.93
Abstract
- Ascites following radical hysterectomy with retroperitoneal lymphadenectomy for invasive cervical cancer has been reported previously. Most of these reports described chylous ascites. The chylous ascitic fluid is milky; further, chylous ascites leads to nutritional problems. Authors present the case of a patient who developed serous ascites following radical hysterectomy with bilateral pelvic lymphadenectomy. The amount of ascites was approximately 18,000 ml over 52 days. The patient had no nutritional problems or complications. Although the etiology could not be determined, Authors surmise that the ascites may have been due to massive drainage from injured lymphatic channels below the cisterna chyli. Authors could not found any literatures which described massive serous ascites following surgery in gynecologic malignancy and reports this case with review of literatures.
MeSH Terms
Figure
Reference
-
1. Geisler JP, Foster RS, Sutton GP. Chyloperitoneum following treatment for advanced gynecologic malignancies. Obstet Gynecol. 1994. 83:883–885.2. Aalami OO, Allen DB, Organ CH Jr. Chylous ascites: A collective review. Surgery. 2000. 128:761–778.
Article3. Hibbeln JF, Wehmueller MD, Wilbur AC. Chylous ascites: CT and ultrasound appearance. Abdom Imaging. 1995. 20:138–140.
Article4. Leibovitch I, Mor Y, Golomb J, Ramon J. The diagnosis and management of postoperative chylous ascites. J Urol. 2002. 167:449–457.
Article5. Baniel J, Foster RS, Rowland RG, Bihrle R, Donohue JP. Management of chylous ascites after retroperitoneal lymph node dissection for testicular cancer. J Urol. 1993. 150:1422–1424.
Article6. Ablan CJ, Littooy FN, Freeark RJ. Postoperative chylous ascites: Diagnosis and treatment. A series report and literature review. Arch Surg. 1990. 125:270–273.7. Jansen TT, Debruyne FM, Delaere KP, de Vries JD. Chylous ascites after retroperitoneal lymph node dissection. Urology. 1984. 23:565–567.
Article8. Ward PC. Interpretation of ascitic fluid data. Postgrad Med. 1982. 71:171–173. 176–178.
Article9. Staats BA, Ellefson RD, Budahn LL, Dines DE, Prakash UB, Offord K. The lipoprotein profile of chylous and nonchylous pleural effusions. Mayo Clin Proc. 1980. 55:700–704.10. Lentz SS, Schary MF, Wilson TO. Chylous ascites after whole-abdomen irradiation for gynecologic malignancy. Int J Radiat Oncol Biol Phys. 1990. 19:435–438.
Article11. Nurettin B, Aylin PC, Gokhan T, Nejat O, M. Faruk K. Chylous ascites following paraaortic lymphadenectomy: A case report. Gynecol Oncol. 2004. 93:711–714.12. Susan LS, Michael N, John RL. Chylous ascites: A sequel of pelvic radiation therapy. Gynecol Oncol. 1985. 66:832–835.13. Janetschek G, Hobisch A, Hittmair A, Höltl L, Peschel R, Bartsch G. Laparoscopic retroperitoneal lymphadenectomy after chemotherapy for stage IIB nonseminomatous testicular carcinoma. J Urol. 1999. 161:477–481.
Article14. Baniel J, Foster RS, Rowland RG, Bihrle R, Donohue JP. Complications of post-chemotherapy retroperitoneal lymph node dissection. J Urol. 1995. 153:976–980.15. James H. Pathogenic effects of a high peritoneal transport rate. Semin Dial. 2000. 13:188–193.16. Richard HT, Benjamin DLL, John CM. Townsend Courtney M., Daniel Beauchamp R., Mark Evers B., Mattox Kenneth, editors. Abdominal wall, umbilicus, peritoneum, mesenteries, omentum and retroperitoneum. Sabiston Textbook of Surgery. 2004. 17th ed. Philadelphia, Pennsylvania: Elsevier Saunders;1181–1182.17. Franchi M, Trimbos JB, Zanaboni F, v d Velden J, Reed N, Coens C, et al. Randomized trial of drains versus no drains following radical hysterectomy and pelvic lymph node dissection: A European Organization for Research and Treatment of Cancer-Gynecological Cancer Group(EORTC-GCG) study in 234 patients. Eur J Cancer. 2007. 43:1265–1268.18. Srisomboon J, Phongnarisorn C, Suprasert P, Cheewakriangkrai C, Siriaree S, Charoenkwan K. A prospective randomized study comparing retroperitoneal drainage with no drainage and no peritonealization following radical hysterectomy and pelvic lymphadenectomy for invasive cervical cancer. J Obstet Gyneacol Res. 2002. 28:149–153.19. Al-Ghamdi MY, Bedi A, Reddy SB, Tanton RT, Peltekian KM. Chylous ascites secondary to pancreatitis: management of an uncommon entity using parenteral nutrition and octreotide. Dig Dis Sci. 2007. 52:2261–2266.
Article20. Tom PM, Shahab A, Jeffrey MF. Chylous ascites following treatment for gynecologic malignancies. Gynecol Oncol. 2002. 86:370–374.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pelvic Drainage Following Radical Hysterectomy with Pelvic Lymphadenectomy for Cervical Cancer: Is it Necessary?
- Chylous ascites, following radical hysterectomy with pelvic lymph node dissection in a patient with cervical cancer
- Laparoscopic Pelvic Lymphadenectomy in Cervical Cancer
- Multivariate prognostic analysis of adenocarcinoma of the uterine cervix treated with radical hysterectomy and systematic lymphadenectomy
- Recent Management of FIGO stage IB2 Cervical Cancer