J Gynecol Oncol.
2013 Jul;24(3):215-221. 10.3802/jgo.2013.24.3.215.
p16INK4a immunohistochemistry is a promising biomarker to predict the outcome of low grade cervical intraepithelial neoplasia: comparison study with HPV genotyping
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Keio University School of Medicine, Tokyo, Japan. fujiit44@gmail.com
- 2Department of Pathology, Keio University School of Medicine, Tokyo, Japan.
- 3Department of Obstetrics and Gynecology, Ohashi Medical Center, Toho University School of Medicine, Tokyo, Japan.
- KMID: 2288527
- DOI: http://doi.org/10.3802/jgo.2013.24.3.215
Abstract
OBJECTIVE
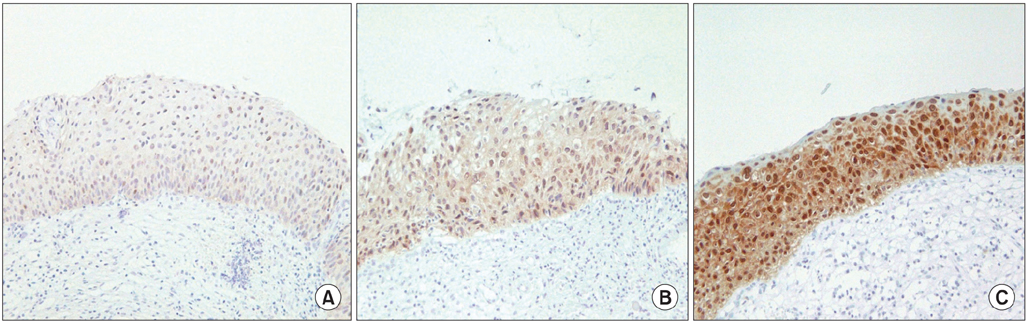
In cervical intraepithelial neoplasia (CIN), p16INK4a immunohistochemistry has been reported to be a useful diagnostic biomarker. However, limited information is available about the association between the p16INK4a immunohistochemistry and the outcomes of CIN. Here, we report p16INK4a immunohistochemistry as an effective biomarker to predict the outcomes of CIN.
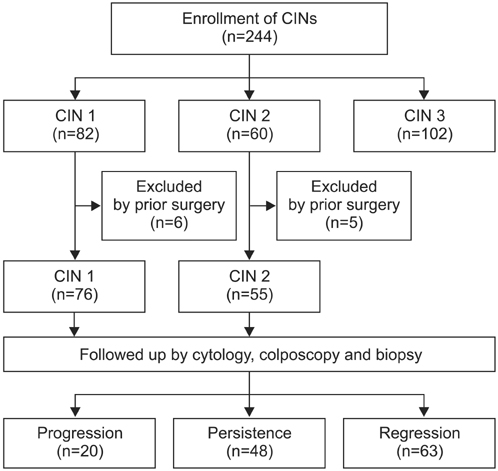
METHODS
p16INK4a immunohistochemistry was performed in patients with CIN from January 2000 to August 2009. Among these patients, we have performed a retrospective analysis of the medical records to evaluate the outcome of CIN 1-2 and performed statistical analysis to determine the correlation between p16INK4a expression and the outcomes. We also performed HPV genotyping and analyzed the relation between the infecting human papillomavirus (HPV) genotype and the outcomes.
RESULTS
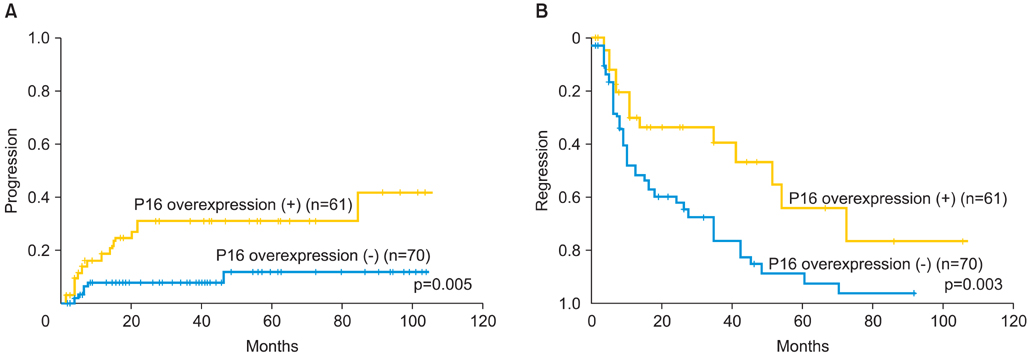
A total of 244 patients, including 82 with CIN 1, 60 with CIN 2, and 102 with CIN 3, were examined. The rate of p16INK4a overexpression increased with increasing CIN grade, 20.7% for CIN 1, 80.0% for CIN 2, and 89.2% for CIN 3, with significant differences between CIN 1 and CIN 2-3 group. In the 131 CIN 1-2 patients, the progression rate was significantly higher for the patients showing p16INK4a overexpression than for those not showing p16INK4a overexpression (p=0.005); the regression rate was also found to be significantly lower for the patients showing p16INK4a overexpression (p=0.003). High-risk HPV genotypes were detected in 73 patients (73.7%). Both progression and regression rates were not significantly different between the high-risk HPV-positive and HPV-negative groups (p=0.401 and p=0.381, respectively).
CONCLUSION
p16INK4a overexpression was correlated with the outcome of CIN 1-2, and p16INK4a is considered to be a superior biomarker for predicting the outcome of CIN 1-2 compared with HPV genotyping.
Keyword
MeSH Terms
Figure
Reference
-
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55:74–108.2. Ostor AG. Natural history of cervical intraepithelial neoplasia: a critical review. Int J Gynecol Pathol. 1993; 12:186–192.3. Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007; 370:890–907.4. Nakagawa H, Sugano K, Fujii T, Kubushiro K, Tsukazaki K, Nozawa S. Frequent detection of human papilloma viruses in cervical dysplasia by PCR single-strand DNA-conformational polymorphism analysis. Anticancer Res. 2002; 22:1655–1660.5. Fujii T, Tsukazaki K, Kiguchi K, Kubushiro K, Yajima M, Nozawa S. The major E6/E7 transcript of HPV-16 in exfoliated cells from cervical neoplasia patients. Gynecol Oncol. 1995; 58:210–215.6. Wright TC Jr, Massad LS, Dunton CJ, Spitzer M, Wilkinson EJ, Solomon D. 2006 consensus guidelines for the management of women with cervical intraepithelial neoplasia or adenocarcinoma in situ. Am J Obstet Gynecol. 2007; 197:340–345.7. Cuzick J, Clavel C, Petry KU, Meijer CJ, Hoyer H, Ratnam S, et al. Overview of the European and North American studies on HPV testing in primary cervical cancer screening. Int J Cancer. 2006; 119:1095–1101.8. Cuschieri K, Wentzensen N. Human papillomavirus mRNA and p16 detection as biomarkers for the improved diagnosis of cervical neoplasia. Cancer Epidemiol Biomarkers Prev. 2008; 17:2536–2545.9. Khleif SN, DeGregori J, Yee CL, Otterson GA, Kaye FJ, Nevins JR, et al. Inhibition of cyclin D-CDK4/CDK6 activity is associated with an E2F-mediated induction of cyclin kinase inhibitor activity. Proc Natl Acad Sci U S A. 1996; 93:4350–4354.10. Hu L, Guo M, He Z, Thornton J, McDaniel LS, Hughson MD. Human papillomavirus genotyping and p16INK4a expression in cervical intraepithelial neoplasia of adolescents. Mod Pathol. 2005; 18:267–273.11. Serrano M, Hannon GJ, Beach D. A new regulatory motif in cell-cycle control causing specific inhibition of cyclin D/CDK4. Nature. 1993; 366:704–707.12. Sano T, Oyama T, Kashiwabara K, Fukuda T, Nakajima T. Expression status of p16 protein is associated with human papillomavirus oncogenic potential in cervical and genital lesions. Am J Pathol. 1998; 153:1741–1748.13. Omori M, Hashi A, Nakazawa K, Yuminamochi T, Yamane T, Hirata S, et al. Estimation of prognoses for cervical intraepithelial neoplasia 2 by p16INK4a immunoexpression and high-risk HPV in situ hybridization signal types. Am J Clin Pathol. 2007; 128:208–217.14. Hariri J, Oster A. The negative predictive value of p16INK4a to assess the outcome of cervical intraepithelial neoplasia 1 in the uterine cervix. Int J Gynecol Pathol. 2007; 26:223–228.15. del Pino M, Garcia S, Fuste V, Alonso I, Fuste P, Torne A, et al. Value of p16(INK4a) as a marker of progression/regression in cervical intraepithelial neoplasia grade 1. Am J Obstet Gynecol. 2009; 201:488.e1–488.e7.16. Ozaki S, Zen Y, Inoue M. Biomarker expression in cervical intraepithelial neoplasia: potential progression predictive factors for low-grade lesions. Hum Pathol. 2011; 42:1007–1012.17. Matsumoto K, Oki A, Furuta R, Maeda H, Yasugi T, Takatsuka N, et al. Predicting the progression of cervical precursor lesions by human papillomavirus genotyping: a prospective cohort study. Int J Cancer. 2011; 128:2898–2910.18. Masumoto N, Fujii T, Ishikawa M, Mukai M, Saito M, Iwata T, et al. Papanicolaou tests and molecular analyses using new fluid-based specimen collection technology in 3000 Japanese women. Br J Cancer. 2003; 88:1883–1888.19. Fujii T, Saito M, Iwata T, Hirao N, Nishio H, Ohno A, et al. Ancillary testing of liquid-based cytology specimens for identification of patients at high risk of cervical cancer. Virchows Arch. 2008; 453:545–555.20. Sasagawa T, Basha W, Yamazaki H, Inoue M. High-risk and multiple human papillomavirus infections associated with cervical abnormalities in Japanese women. Cancer Epidemiol Biomarkers Prev. 2001; 10:45–52.21. Onuki M, Matsumoto K, Satoh T, Oki A, Okada S, Minaguchi T, et al. Human papillomavirus infections among Japanese women: age-related prevalence and type-specific risk for cervical cancer. Cancer Sci. 2009; 100:1312–1316.22. Ishikawa M, Fujii T, Saito M, Nindl I, Ono A, Kubushiro K, et al. Overexpression of p16 INK4a as an indicator for human papillomavirus oncogenic activity in cervical squamous neoplasia. Int J Gynecol Cancer. 2006; 16:347–353.23. Negri G, Vittadello F, Romano F, Kasal A, Rivasi F, Girlando S, et al. p16INK4a expression and progression risk of low-grade intraepithelial neoplasia of the cervix uteri. Virchows Arch. 2004; 445:616–620.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of p16INK4a Immunocytochemical Staining in ASC-H Patients
- Cervical intraepithelial neoplasia 3, coinfected with HPV-16 and -18: case report
- Is the expression of p16INK4A and galectin-3 correlated with disease progression of cervical neoplasia?
- Effect of Surgical Therapy on the Courses of Human Papillomavirus Infection in Cervical Intraepithelial Neoplasia
- Detection of Human Papillomavius DNA by Hybrid Capture Test in Cervical Intraepithelial Neoplasia and Carcinoma