J Breast Cancer.
2015 Mar;18(1):29-35. 10.4048/jbc.2015.18.1.29.
Local Control of Brain Metastasis: Treatment Outcome of Focal Brain Treatments in Relation to Subtypes
- Affiliations
-
- 1Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. gsjjoon@yuhs.ac
- 2Department of Surgery, Eulji General Hospital, Eulji University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2286334
- DOI: http://doi.org/10.4048/jbc.2015.18.1.29
Abstract
- PURPOSE
To investigate treatment options for local control of metastasis in the brain, we compared focal brain treatment (FBT) with or without whole brain radiotherapy (WBRT) vs. WBRT alone, for breast cancer patients with tumor relapse in the brain. We also evaluated treatment outcomes according to the subtypes.
METHODS
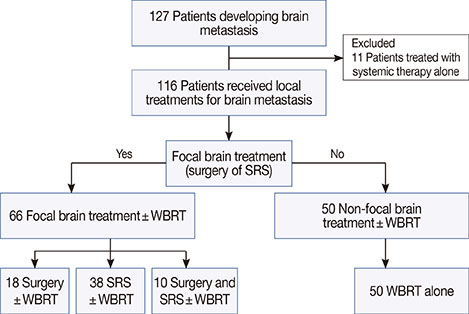
We conducted a retrospective review of breast cancer patients with brain metastasis after primary surgery. All patients received at least one local treatment for brain metastasis. Surgery or stereotactic radiosurgery was categorized as FBT. Patients were divided into two groups: the FBT group received FBT+/-WBRT, whereas the non-FBT group received WBRT alone. Subtypes were defined as follows: hormone receptor (HR)-positive/human epidermal growth factor receptor 2 (HER2)-negative, HR-positive/HER2-positive, HR-negative/HER2-positive, and triple-negative (TN). We examined the overall survival after brain metastasis (OSBM), brain metastasis-specific survival (BMSS), and brain metastasis-specific progression-free survival (BMPFS).
RESULTS
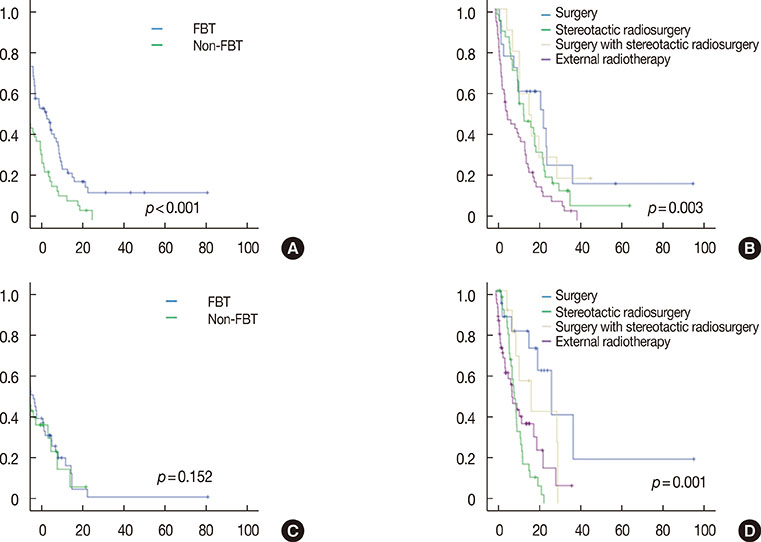
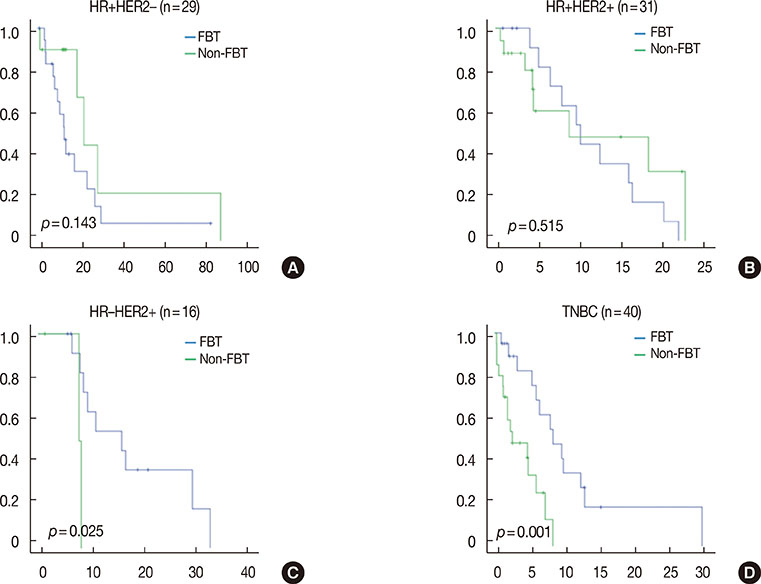
A total of 116 patients were identified. After a median follow-up of 50.9 months, the median OSBM was 11.5 months (95% confidence interval, 9.0-14.1 months). The FBT group showed significantly superior OSBM and BMSS. However, FBT was not an independent prognostic factor for OSBM and BMSS on multivariate analyses. In contrast, multivariate analyses showed that patients who underwent surgery had improved BMPFS, indicating local control of metastasis in the brain. FBT resulted in better BMPFS in patients with HR-negative/HER2-positive cancer or the TN subtype.
CONCLUSION
We found that patients who underwent surgery experienced improved local control of brain metastasis, regardless of its extent. Furthermore, FBT showed positive results and could be considered for better local control of brain metastasis in patients with aggressive subtypes such as HER2-positive and TN.
MeSH Terms
Figure
Reference
-
1. Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012; 62:220–241.
Article2. Xue J, Peng G, Yang JS, Ding Q, Cheng J. Predictive factors of brain metastasis in patients with breast cancer. Med Oncol. 2013; 30:337.
Article3. Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013; 45:1–14.
Article4. Hofer S, Pestalozzi BC. Treatment of breast cancer brain metastases. Eur J Pharmacol. 2013; 717:84–87.
Article5. Karam I, Hamilton S, Nichol A, Woods R, Speers C, Kennecke H, et al. Population-based outcomes after brain radiotherapy in patients with brain metastases from breast cancer in the Pre-Trastuzumab and Trastuzumab eras. Radiat Oncol. 2013; 8:12.
Article6. Ahn HK, Park YH, Lee SJ, Park S, Maeng CH, Park W, et al. Clinical implication of Time To Brain Metastasis (TTBM) according to breast cancer subtypes. Springerplus. 2013; 2:136.
Article7. Padovani L, Muracciole X, Régis J. , knife radiosurgery of brain metastasis from breast cancer. Prog Neurol Surg. 2012; 25:156–162.8. Cheng X, Hung MC. Breast cancer brain metastases. Cancer Metastasis Rev. 2007; 26:635–643.
Article9. Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990; 322:494–500.
Article10. Vecht CJ, Haaxma-Reiche H, Noordijk EM, Padberg GW, Voormolen JH, Hoekstra FH, et al. Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol. 1993; 33:583–590.
Article11. Central nervous system cancers, version 1. National Comprehensive Cancer Network;2013. Accessed August 21st, 2014. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.12. Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, Luo X, et al. Effect of tumor subtype on survival and the graded prognostic assessment for patients with breast cancer and brain metastases. Int J Radiat Oncol Biol Phys. 2012; 82:2111–2117.
Article13. Sperduto PW, Kased N, Roberge D, Chao ST, Shanley R, Luo X, et al. The effect of tumor subtype on the time from primary diagnosis to development of brain metastases and survival in patients with breast cancer. J Neurooncol. 2013; 112:467–472.
Article14. Jang G, Lee SS, Ahn JH, Jung KH, Lee H, Gong G, et al. Clinical features and course of brain metastases in triple-negative breast cancer: comparison with human epidermal growth factor receptor 2-positive and other type at single institution in Korea. Breast Cancer Res Treat. 2011; 128:171–177.
Article15. Kim HJ, Im SA, Keam B, Kim YJ, Han SW, Kim TM, et al. Clinical outcome of central nervous system metastases from breast cancer: differences in survival depending on systemic treatment. J Neurooncol. 2012; 106:303–313.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long Term Survival in Patient with Hepatocellular Carcinoma after Surgical Resection of Brain Metastasis: A Case Report
- Advances in Brain Metastasis Models
- Treatment Outcome of Brain Metastasis after the Cranial Radiotherapy Followed by Fractionated Stereotactic Radiotherapy and Its Prognostic Factors
- Revisiting the Role of Surgical Resection for Brain Metastasis
- The Initial Computerized Tomography Findings of the Brain and the Functional Outcome in Traumatic Brain Injured Patients