Infect Chemother.
2008 Oct;40(5):301-304. 10.3947/ic.2008.40.5.301.
A Case of Nocardia farcinica Brain Abscess in the Patient Receiving Steroid Treatment
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. molder@uniter.co.kr
- 2Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2285058
- DOI: http://doi.org/10.3947/ic.2008.40.5.301
Abstract
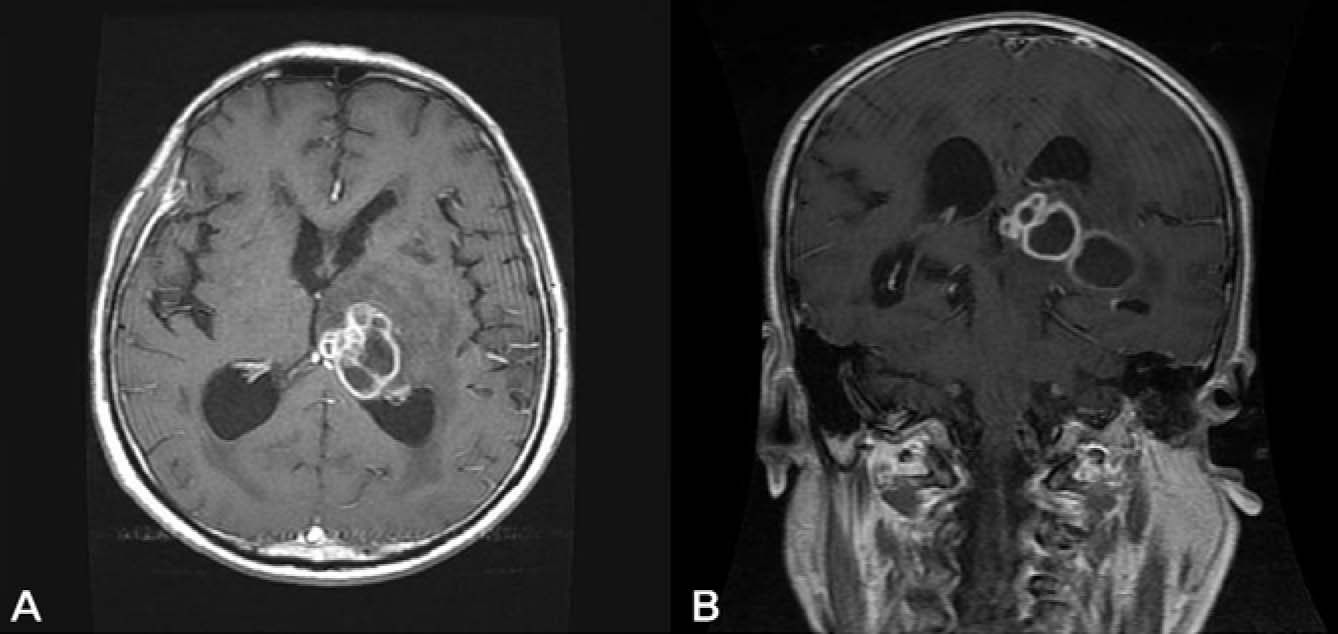
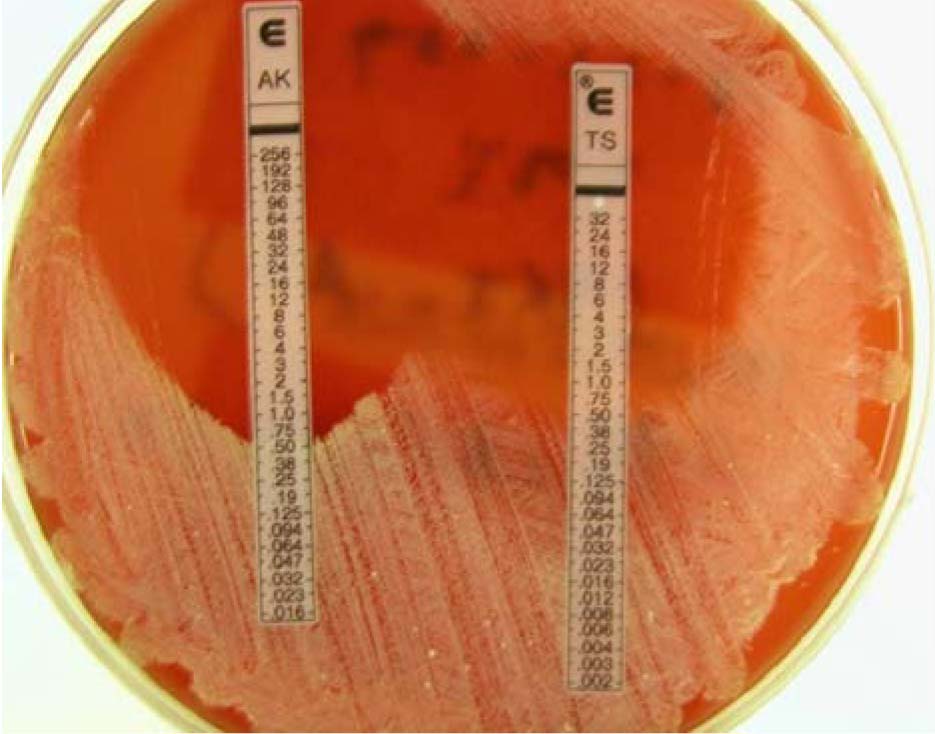
- Nocardiosis occurs mostly in the immunocompromised patients. N. farcinica is known to have resistance to some antibiotics and significant increase in morbidity and mortality in patients requiring long-term treatment. Nocardia farcinica infection, especially brain abscess, has not been reported in Korea. Here, we report a case of N. farcinica brain abscess in a patient receiving steroid treatment. The patient was a 64 year-old male with gouty arthritis. He received steroid for more than two months, because of allopurinol-hypersensitivity syndrome with skin rash. After three months of steroid therapy, he visited other hospital with mild fever and left thigh pain and was diagnosed of intramuscular abscess due to gram positive bacilli. One month later, he visited our hospital with right side weakness and was diagnosed as brain abscess. The causative organism turned out to be N. farcinica, which was confirmed by means of 16S rRNA sequencing. Antibiotics were selected by E-test results and treatment was successful
MeSH Terms
Figure
Cited by 3 articles
-
The First Case of Catheter-related Bloodstream Infection Caused by Nocardia farcinica
Sang Taek Heo, Kwan Soo Ko, Ki Tae Kwon, Seong Yeol Ryu, In Gyu Bae, Won Sup Oh, Jae-Hoon Song, Kyong Ran Peck
J Korean Med Sci. 2010;25(11):1665-1668. doi: 10.3346/jkms.2010.25.11.1665.Reliability of Sequence-Based Identification of Microorganism
Heungsup Sung, Mi-Na Kim
Infect Chemother. 2008;40(6):355-356. doi: 10.3947/ic.2008.40.6.355.A Case of Disseminated Nocardiosis by Nocardia brasiliensis after Steroid Injection
Na Ra Yun, Hee Jeong Lee, Su Jin Hong, Jun Lee, Dong-Min Kim, Sook Jin Jang, Ran Hong
Infect Chemother. 2011;43(4):367-371. doi: 10.3947/ic.2011.43.4.367.
Reference
-
1. Saubolle MA, Sussland D. Nocardiosis: review of clinical and laboratory experience. J Clin Microbiol. 2003. 41:4497–4501.2. Beaman BL, Beaman L. Nocardia species: host-parasite relationships. Clin Microbiol Rev. 1994. 7:213–264.
Article3. Torres OH, Domingo P, Pericas R, Boiron P, Montiel JA, Vazquez G. Infection caused by Nocardia farcinica: case report and review. Eur J Clin Microbiol Infect Dis. 2000. 19:205–212.4. Lederman ER, Crum NF. A case series and focused review of nocardiosis: clinical and microbiologic aspects. Medicine. 2004. 83:300–313.5. Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol R. v. 2006. 19:259–282.
Article6. Lee KW, Jeong MS, Kim SH, Song SH, Koo SH, Kim SY, Shin YT. Nocardial Brain Abscess Complicated in A Patient with Systemic Lupus Erythematosus. Korean J Med. 1995. 48:545–551.7. Butler WR, Kilburn JO, Kubica GP. High-performance liquid chromatography analysis of mycolic acids as an aid in laboratory identification of Rhodococcus and Nocardia species. J Clin Microbiol. 1987. 25:2126–2131.
Article8. Choe WH, Kang JO, Pai HJ, Choi TY. A Case of Nocardia asteroides type I Induced Pneumonia. Korean J Lab Med. 2005. 25:324–328.9. Steingrube VA, Brown BA, Gibson JL, Wilson RW, Brown J, Blacklock Z, Jost K, Locke S, Ulrich RF, Wallace RJ Jr. DNA amplification and restriction endonuclease analysis for differentiation of 12 species and taxa of Nocardia, including recognition of four new taxa within the Nocardia asteroides complex. J Clin Microbiol. 1995. 33:3096–3101.
Article10. Roth A, Andrees S, Kroppenstedt RM, Harmsen D, Mauch H. Phylogeny of the genus Nocardia based on reassessed 16S rRNA gene sequences reveals underspeciation and division of strains classified as Nocardia asteroides into three established species and two unnamed taxons. J Clin Microbiol. 2003. 41:851–856.
Article11. Laurent FJ, Provost F, Boiron P. Rapid identification of clinically relevant Nocardia species to genus level by 16S rRNA gene PCR. J Clin Microbiol. 1999. 37:99–102.
Article12. Mandell GL, Bennett JE, Dolin R. Principles and Practice of Infectious disease. 2005. 5th. New York: Churchill Livingstone;2916–2922. chapter 252.13. Wallace RJ Jr, Tsukamura M, Brown BA, Brown J, Steingrube VA, Zhang YS, Nash DR. Cefotaxime-resistant Nocardia asteroides strains are isolates of the controversial species Nocardia farcinica. J Clin Microbiol. 1990. 28:2726–2732.
Article14. Woods GL, Brown-Elliott BA, Desmond EP, Hall GS, Heifets L, Pfyffer GE, Ridderhof JC, Wallace RJ Jr, Warren NG, Witebsky FG. Susceptibility testing of mycobacteria, nocardia, and other aerobic actinomyetes; approved standard. 2003. Wayne, Pennsylvania: NCCLS;M24-A.15. Biehle JR, Cavalieri SJ, Saubolle MA, Getsinger LJ. Comparative evaluation of the E test for susceptibility testing of Nocardia species. Diagn Microbiol Infect Dis. 1994. 19:101–110.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Nocardia farcinica Brain Abscess in a Focal Segmental Glomerulosclerosis Patient after Steroid Treatment
- Nocardia Brain Abscess in an Immunocompetent Patient
- A Case of Disseminated Nocardiosis by Nocardia brasiliensis after Steroid Injection
- Nocardia Brain Abscess in a Liver Transplant Recipient
- A Case of Intramuscular Abscess Caused by Nocardia farcinica in a Patient with Lupus Nephritis Concurrent with Pulmonary Tuberculosis