Clin Nutr Res.
2013 Jul;2(2):115-124. 10.7762/cnr.2013.2.2.115.
Effect of the Telephone-Delivered Nutrition Education on Dietary Intake and Biochemical Parameters in Subjects with Metabolic Syndrome
- Affiliations
-
- 1Health Promotion Center, Seoul National University of Bundang Hospital, Seongnam 463-707, Korea.
- 2Department of Food and Nutrition, Wonkwang University, Iksan 570-749, Korea. ccha@wku.ac.kr
- KMID: 2279666
- DOI: http://doi.org/10.7762/cnr.2013.2.2.115
Abstract
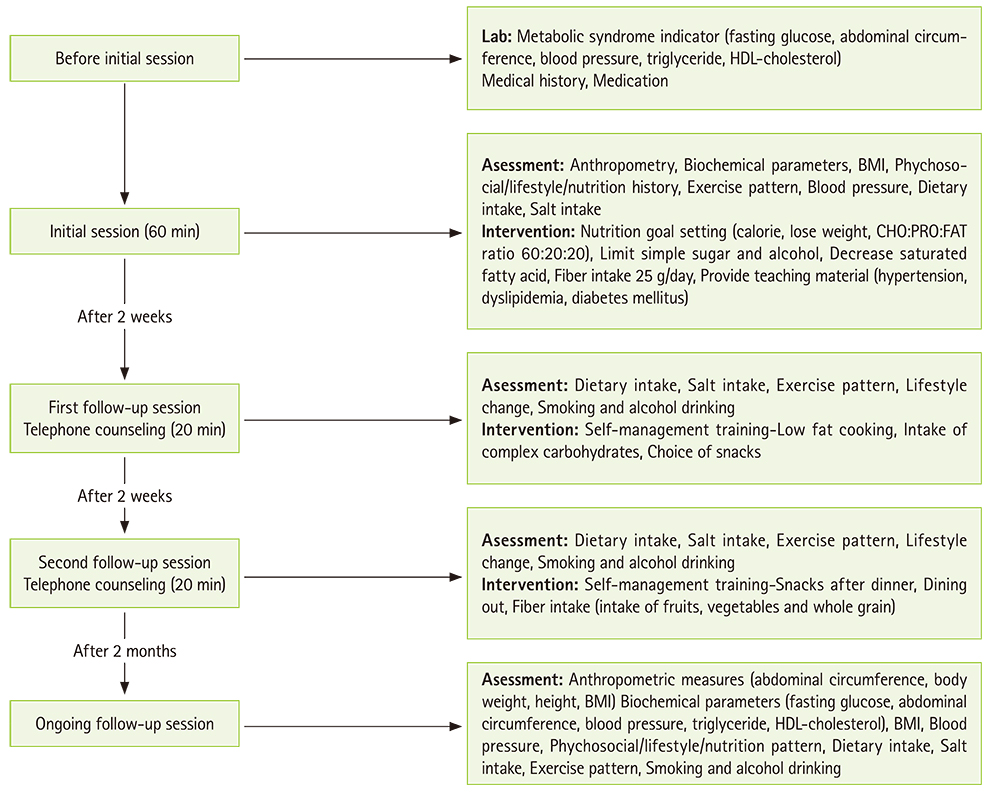
- As prevalence of metabolic syndrome has rapidly increased over the past decade, lifestyle changes including dietary habits are considered as a therapeutic cornerstone for metabolic syndrome, cardiovascular complications and type 2 diabetes. We evaluated the effectiveness of a telephone-delivered nutrition education to improve metabolic parameters compared with a single-visit with a dietitian in subjects with metabolic syndrome. A total of seventy-one adults who met diagnostic criteria for the metabolic syndrome were randomly assigned to either the single-visit group or the in-depth nutrition education group during a 3-month intervention study period. The in-depth telephone-delivered nutrition education group had an initial visit with a dietitian and additional two telephone counseling during the first 4 weeks of the study periods. Sixty-six subjects completed a 3-month intervention study. The trial examined participant's anthropometric changes and dietary intakes as well as changes in the metabolic syndrome factors. At the end of the trial, the in-depth nutrition education group showed significantly higher reduction in weight, body fat and abdominal circumference compared with the other group (p < 0.05). In the in-depth nutrition groups, the prevalence of metabolic syndrome was decreased to 45.5%, while 69.7% of the subjects were metabolic syndrome patients in the single-visit group (p < 0.05). These results demonstrate that the telephone-intervention counseling is a feasible mean to deliver dietary intervention in patients with metabolic syndrome.
MeSH Terms
Figure
Cited by 2 articles
-
Diet, Sleep and Metabolic Syndrome Among a Legal Amazon Population, Brazil
Poliana Rodrigues dos Santos, Graziele Souza Lira Ferrari, Carlos K B Ferrari
Clin Nutr Res. 2015;4(1):41-45. doi: 10.7762/cnr.2015.4.1.41.Importance of Adherence to Personalized Diet Intervention in Obesity Related Metabolic Improvement in Overweight and Obese Korean Adults
Juhyun An, So Ra Yoon, Jae Hyang Lee, Hyunyoung Kim, Oh Yoen Kim
Clin Nutr Res. 2019;8(3):171-183. doi: 10.7762/cnr.2019.8.3.171.
Reference
-
1. Statistics Korea [Internet]. The statistics of mortality and the causes. Daejeon: Statistics Korea;2011. cited 2013 May 10. Available from: http://kostat.go.kr/.2. Lim S, Park KS, Lee HK, Cho SI. Korean National Health and Nutrition Examination Surveys. Changes in the characteristics of metabolic syndrome in Korea over the period 1998-2001 as determined by Korean National Health and Nutrition Examination Surveys. Diabetes Care. 2005; 28:1810–1812.
Article3. Malik S, Wong ND, Franklin SS, Kamath TV, L'Italien GJ, Pio JR, Williams GR. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004; 110:1245–1250.
Article4. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002; 288:2709–2716.
Article5. Wilson C, Brown T, Acton K, Gilliland S. Effects of clinical nutrition education and educator discipline on glycemic control outcomes in the Indian health service. Diabetes Care. 2003; 26:2500–2504.
Article6. Franz MJ, Monk A, Barry B, McClain K, Weaver T, Cooper N, Upham P, Bergenstal R, Mazze RS. Effectiveness of medical nutrition therapy provided by dietitians in the management of non-insulin-dependent diabetes mellitus: a randomized, controlled clinical trial. J Am Diet Assoc. 1995; 95:1009–1017.
Article7. Ash S, Reeves MM, Yeo S, Morrison G, Carey D, Capra S. Effect of intensive dietetic interventions on weight and glycaemic control in overweight men with Type II diabetes: a randomised trial. Int J Obes Relat Metab Disord. 2003; 27:797–802.
Article8. Pritchard DA, Hyndman J, Taba F. Nutritional counselling in general practice: a cost effective analysis. J Epidemiol Community Health. 1999; 53:311–316.
Article9. Welty FK, Nasca MM, Lew NS, Gregoire S, Ruan Y. Effect of onsite dietitian counseling on weight loss and lipid levels in an outpatient physician office. Am J Cardiol. 2007; 100:73–75.
Article10. Koopman H, Spreeuwenberg C, Westerman RF, Donker AJ. Dietary treatment of patients with mild to moderate hypertension in a general practice: a pilot intervention study (2). Beyond three months. J Hum Hypertens. 1990; 4:372–374.11. Shon CM, Nho MR, Lee YH, Lim JH. The clinical and cost effectiveness of medical nutrition therapy in persons with hypercholesterolemia. J Korean Diet Assoc. 2003; 9:32–39.12. Delahanty LM, Sonnenberg LM, Hayden D, Nathan DM. Clinical and cost outcomes of medical nutrition therapy for hypercholesterolemia: a controlled trial. J Am Diet Assoc. 2001; 101:1012–1023.
Article13. Henkin Y, Shai I, Zuk R, Brickner D, Zuilli I, Neumann L, Shany S. Dietary treatment of hypercholesterolemia: do dietitians do it better? A randomized, controlled trial. Am J Med. 2000; 109:549–555.
Article14. Goode AD, Reeves MM, Eakin EG. Telephone-delivered interventions for physical activity and dietary behavior change: an updated systematic review. Am J Prev Med. 2012; 42:81–88.
Article15. Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change: a systematic review. Am J Prev Med. 2007; 32:419–434.
Article16. Kim CG, Chung CH. Effects of telephone consulting program on self-efficacy and self-care in NIDDM patients. J Korean Acad Adult Nurs. 2002; 14:306–314.17. Davis RM, Hitch AD, Salaam MM, Herman WH, Zimmer-Galler IE, Mayer-Davis EJ. TeleHealth improves diabetes self-management in an underserved community: diabetes TeleCare. Diabetes Care. 2010; 33:1712–1717.
Article18. Kris-Etherton PM, Taylor DS, Smiciklas-Wright H, Mitchell DC, Bekhuis TC, Olson BH, Slonim AB. High-soluble-fiber foods in conjunction with a telephone-based, personalized behavior change support service result in favorable changes in lipids and lifestyles after 7 weeks. J Am Diet Assoc. 2002; 102:503–510.
Article19. Izquierdo RE, Knudson PE, Meyer S, Kearns J, Ploutz-Snyder R, Weinstock RS. A comparison of diabetes education administered through telemedicine versus in person. Diabetes Care. 2003; 26:1002–1007.
Article20. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr. International Diabetes Federation Task Force on Epidemiology and Prevention. Hational Heart, Lung, and Blood Institute. American Heart Association. World Heart Federation. International Atherosclerosis Society. International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009; 120:1640–1645.21. American Dietetic Association. Medical nutrition therapy evidence-based guides for practice. Nutrition practice guidelines for type 1 and 2 diabetes mellitus [CD-ROM]. Chicago (IL): American Dietetic Association;2001.22. Franz MJ. The role of nutrition therapy and dietitians in the management of the metabolic syndrome. Curr Diab Rep. 7:60–65. 2007.
Article23. The Lipid Research Clinics Coronary Primary Prevention Trial results. I. Reduction in incidence of coronary heart disease. JAMA. 1984; 251:351–364.24. The Lipid Research Clinics Coronary Primary Prevention Trial results. II. The relationship of reduction in incidence of coronary heart disease to cholesterol lowering. JAMA. 1984; 251:365–374.25. Rossouw JE, Lewis B, Rifkind BM. The value of lowering cholesterol after myocardial infarction. N Engl J Med. 1990; 323:1112–1119.
Article26. Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ. 1994; 308:367–372.
Article27. Kim M, Kim J, Bae W, Kim S, Lee Y, Na W, Sohn C. Relationship between nutrients intakes, dietary quality, and serum concentrations of inflammatory markers in metabolic syndrome patients. Korean J Community Nutr. 2011; 16:51–61.
Article28. Park SY, Yang YJ, Kim Y. Effects of nutrition education using a ubiquitous healthcare (u-Health) service on metabolic syndrome in male workers. Korean J Nutr. 2011; 44:231–242.
Article29. Kang JY, Cho SW, Lee JY, Sung SH, Park YK, Paek YM, Choi TI. The effects of a worksite on-line health education program on metabolic syndrome risk factors and nutrient intakes of male workers. Korean J Nutr. 2010; 43:57–68.
Article30. Song MS, Kim HS. Effect of the diabetes outpatient intensive management programme on glycaemic control for type 2 diabetic patients. J Clin Nurs. 2007; 16:1367–1373.
Article31. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346:393–403.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Nutrient Intake and Dietary Quality of Korean Adults in Metabolic Syndrome Patients According to Taking Medical Care: Based on the 2017 Korea National Health and Nutrition Examination Survey
- Nutritional status and metabolic syndrome risk according to the dietary pattern of adult single-person household, based on the Korea National Health and Nutrition Examination Survey
- Relationship between Dietary Intake and Depression in Metabolic Syndroem among Korean Adults: Korea National Health and Nutrition Examination Survey 2014
- Effects of Nutrition Education Using a Ubiquitous Healthcare (u-Health) Service on Metabolic Syndrome in Male Workers
- Effect of Home-visit Nutrition Education for the Elderly with High Fasting Blood Glucose Levels