Korean J Obstet Gynecol.
2012 Sep;55(9):649-654. 10.5468/KJOG.2012.55.9.649.
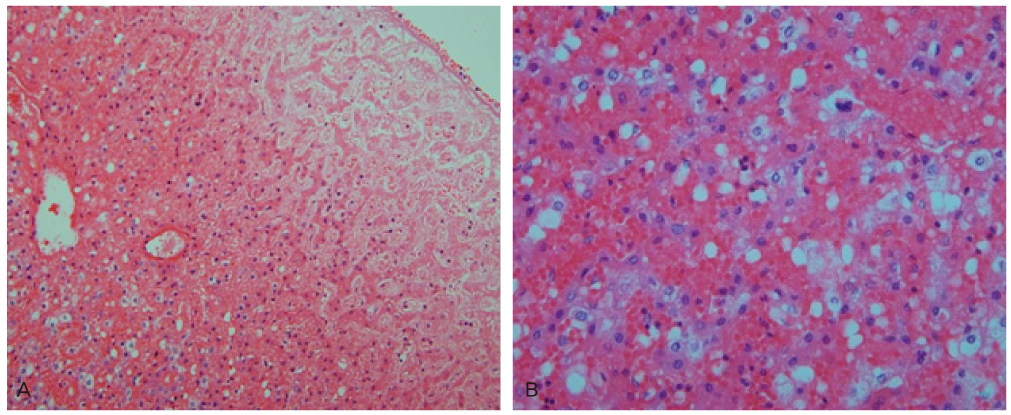
Acute fatty liver of pregnancy with fetal microvesicular hepatic steatosis
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Eulji Hospital, Eulji University School of Medicine, Seoul, Korea. obdrseo@naver.com
- KMID: 2274137
- DOI: http://doi.org/10.5468/KJOG.2012.55.9.649
Abstract
- Acute fatty liver of pregnancy (AFLP) is a serious maternal disease occurring in the third trimester of pregnancy with significant perinatal and maternal mortality. Until recently the pathogenesis of AFLP was unknown and still has not been fully elucidated. However, recent molecular advances suggest that AFLP may result from mitochondrial dysfunction. Several reports have documented a strong association between AFLP and a deficiency of the enzyme long-chain 3-hydroxyacyl-CoA dehydrogenase in the fetus, a disorder of mitochondrial fatty acid beta-oxidation. Therefore in this case, through findings of liver biopsy from dead fetus, we report possible causal relationship between fetal liver disease and maternal AFLP with literature reviews.
MeSH Terms
Figure
Cited by 1 articles
-
Maternal Death due to Acute Fatty Liver of Pregnancy
Jeong-Hwa Kwon, Misun Choi, Hongil Ha, Sohyung Park
Korean J Leg Med. 2017;41(4):141-144. doi: 10.7580/kjlm.2017.41.4.141.
Reference
-
1. Knox TA, Olans LB. Liver disease in pregnancy. N Engl J Med. 1996. 335:569–576.2. Treem WR. Mitochondrial fatty acid oxidation and acute fatty liver of pregnancy. Semin Gastrointest Dis. 2002. 13:55–66.3. Buytaert IM, Elewaut GP, Van Kets HE. Early occurrence of acute fatty liver in pregnancy. Am J Gastroenterol. 1996. 91:603–604.4. Reyes H, Sandoval L, Wainstein A, Ribalta J, Donoso S, Smok G, et al. Acute fatty liver of pregnancy: a clinical study of 12 episodes in 11 patients. Gut. 1994. 35:101–106.5. Holzbach RT. Acute fatty liver of pregnancy with disseminated intravascular coagulation. Obstet Gynecol. 1974. 43:740–744.6. Burroughs AK, Seong NH, Dojcinov DM, Scheuer PJ, Sherlock SV. Idiopathic acute fatty liver of pregnancy in 12 patients. Q J Med. 1982. 51:481–497.7. Castro MA, Ouzounian JG, Colletti PM, Shaw KJ, Stein SM, Goodwin TM. Radiologic studies in acute fatty liver of pregnancy. A review of the literature and 19 new cases. J Reprod Med. 1996. 41:839–843.8. Kamijo T, Wanders RJ, Saudubray JM, Aoyama T, Komiyama A, Hashimoto T. Mitochondrial trifunctional protein deficiency. Catalytic heterogeneity of the mutant enzyme in two patients. J Clin Invest. 1994. 93:1740–1747.9. Ushikubo S, Aoyama T, Kamijo T, Wanders RJ, Rinaldo P, Vockley J, et al. Molecular characterization of mitochondrial trifunctional protein deficiency: formation of the enzyme complex is important for stabilization of both alpha- and beta-subunits. Am J Hum Genet. 1996. 58:979–988.10. Ibdah JA, Bennett MJ, Rinaldo P, Zhao Y, Gibson B, Sims HF, et al. A fetal fatty-acid oxidation disorder as a cause of liver disease in pregnant women. N Engl J Med. 1999. 340:1723–1731.11. Rinaldo P, Raymond K, al-Odaib A, Bennett MJ. Clinical and biochemical features of fatty acid oxidation disorders. Curr Opin Pediatr. 1998. 10:615–621.12. Pons R, Roig M, Riudor E, Ribes A, Briones P, Ortigosa L, et al. The clinical spectrum of long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency. Pediatr Neurol. 1996. 14:236–243.13. Yang Z, Zhao Y, Bennett MJ, Strauss AW, Ibdah JA. Fetal genotypes and pregnancy outcomes in 35 families with mitochondrial trifunctional protein mutations. Am J Obstet Gynecol. 2002. 187:715–720.14. Yang Z, Yamada J, Zhao Y, Strauss AW, Ibdah JA. Prospective screening for pediatric mitochondrial trifunctional protein defects in pregnancies complicated by liver disease. JAMA. 2002. 288:2163–2166.15. Ibdah JA. Acute fatty liver of pregnancy: an update on pathogenesis and clinical implications. World J Gastroenterol. 2006. 12:7397–7404.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hepatic failure caused by acute fatty liver of pregnancy treated by orthotopic liver transplantation: A case report
- A Case of Acute Fatty Liver of Pregnancy
- Acute Fatty Liver of Pregnancy Associated with Diabetes Insipidus
- Diagnostic Performance of Hepatic Steatosis Algorithms in Korean Population with Metabolic-Associated Fatty Liver Disease
- Acute fatty liver of pregnancy: A case report