Ann Rehabil Med.
2015 Feb;39(1):81-90. 10.5535/arm.2015.39.1.81.
The Effect of Dual-Task Training on Balance and Cognition in Patients With Subacute Post-Stroke
- Affiliations
-
- 1Department of Rehabilitation Medicine, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea. brkim08@gmail.com
- KMID: 2273023
- DOI: http://doi.org/10.5535/arm.2015.39.1.81
Abstract
OBJECTIVE
To investigate the effect of dual-task training on the recovery of balance ability and cognitive function in patients with subacute stroke.
METHODS
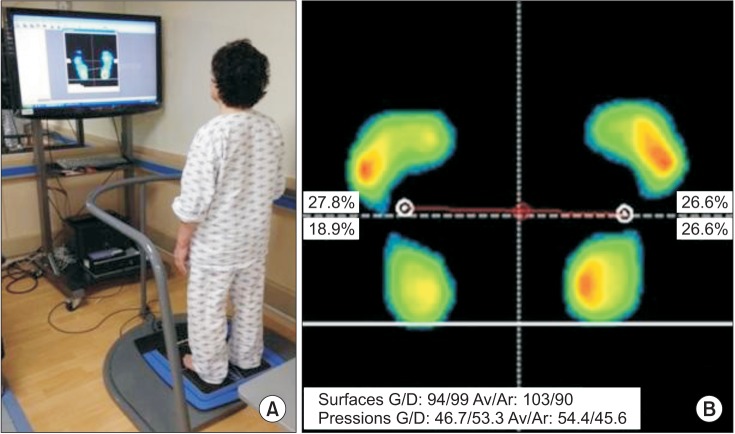
Twenty patients (12 males and eight females; average age, 59.70 years) with subacute stroke were enrolled in this study. All participants were randomly assigned to one of two groups, the dual-task group (n=10) or the control group (n=10). The dual task was simultaneous balance and cognitive training using the BioRescue. All patients were evaluated with posturographic parameters and the Berg Balance Scale for balance ability, a computerized neuropsychological test and the Korean version of the Mini-Mental State Examination for cognitive function, the Fugl-Meyer Assessment for motor function, and the Korean-Modified Barthel Index for activities of daily living (ADL) function before and after 4 weeks of rehabilitation.
RESULTS
The dual-task group showed significant improvements in the pressure of the weight distribution index (WDI), surface area, and length of the stability index during the eyes-open condition; surface area of the limit of stability (LOS) on the hemiparetic and intact sides, and the auditory continuous performance test and backward visual span test after rehabilitation. Although no significant difference was observed for the changes in balance ability or cognitive, motor, and ADL functions between the groups, changes in the WDI pressure during the eyes-open condition and in the area ratio of LOS (hemiparetic/intact) showed a tendency to improve in the dual-task group.
CONCLUSION
Our findings suggest that dual-task training could be as effective as conventional balance training for improving balance and cognition in subacute post-stroke patients.
Keyword
MeSH Terms
Figure
Reference
-
2. Balami JS, Chen RL, Buchan AM. Stroke syndromes and clinical management. QJM. 2013; 106:607–615. PMID: 23483140.
Article3. Winstein CJ, Gardner ER, McNeal DR, Barto PS, Nicholson DE. Standing balance training: effect on balance and locomotion in hemiparetic adults. Arch Phys Med Rehabil. 1989; 70:755–762. PMID: 2802955.4. Kelly VE, Eusterbrock AJ, Shumway-Cook A. A review of dual-task walking deficits in people with Parkinson's disease: motor and cognitive contributions, mechanisms, and clinical implications. Parkinsons Dis. 2012; 2012:918719. PMID: 22135764.
Article5. de Haart M, Geurts AC, Huidekoper SC, Fasotti L, van Limbeek J. Recovery of standing balance in postacute stroke patients: a rehabilitation cohort study. Arch Phys Med Rehabil. 2004; 85:886–895. PMID: 15179641.6. Abernethy B. Dual-task methodology and motor skills research: some applications and methodological constraints. J Hum Mov Stud. 1988; 14:101–132.7. McCulloch K. Attention and dual-task conditions: physical therapy implications for individuals with acquired brain injury. J Neurol Phys Ther. 2007; 31:104–118. PMID: 18025956.
Article8. Plummer-D'Amato P, Altmann LJ, Saracino D, Fox E, Behrman AL, Marsiske M. Interactions between cognitive tasks and gait after stroke: a dual task study. Gait Posture. 2008; 27:683–688. PMID: 17945497.9. Bowen A, Wenman R, Mickelborough J, Foster J, Hill E, Tallis R. Dual-task effects of talking while walking on velocity and balance following a stroke. Age Ageing. 2001; 30:319–323. PMID: 11509310.
Article10. Hyndman D, Ashburn A, Yardley L, Stack E. Interference between balance, gait and cognitive task performance among people with stroke living in the community. Disabil Rehabil. 2006; 28:849–856. PMID: 16777772.
Article11. Hyndman D, Pickering RM, Ashburn A. Reduced sway during dual task balance performance among people with stroke at 6 and 12 months after discharge from hospital. Neurorehabil Neural Repair. 2009; 23:847–854. PMID: 19556368.
Article12. Kizony R, Levin MF, Hughey L, Perez C, Fung J. Cognitive load and dual-task performance during locomotion poststroke: a feasibility study using a functional virtual environment. Phys Ther. 2010; 90:252–260. PMID: 20023003.
Article13. McCulloch KL, Buxton E, Hackney J, Lowers S. Balance, attention, and dual-task performance during walking after brain injury: associations with falls history. J Head Trauma Rehabil. 2010; 25:155–163. PMID: 20473089.14. Melzer I, Tzedek I, Or M, Shvarth G, Nizri O, Ben-Shitrit K, et al. Speed of voluntary stepping in chronic stroke survivors under single- and dual-task conditions: a case-control study. Arch Phys Med Rehabil. 2009; 90:927–933. PMID: 19480867.
Article15. Yang YR, Wang RY, Chen YC, Kao MJ. Dual-task exercise improves walking ability in chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2007; 88:1236–1240. PMID: 17908563.
Article16. Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008; 88:559–566. PMID: 18292215.
Article17. Jung HY, Park JH, Shim JJ, Kim MJ, Hwang MR, Kim SH. Reliability test of Korean version of Berg Balance Scale. J Korean Acad Rehabil Med. 2006; 30:611–618.18. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.19. Kim YH, Shin SH, Park SH, Ko MH. Cognitive assessment for patient with brain injury by computerized neuropsychological test. J Korean Acad Rehabil Med. 2001; 25:209–216.20. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, et al. Development of the Korean version of Modified Barthel Index (K-MBI): multi-center study for subjects with stroke. J Korean Acad Rehabil Med. 2007; 31:283–297.21. Hong SH, Im S, Park GY. The effects of visual and haptic vertical stimulation on standing balance in stroke patients. Ann Rehabil Med. 2013; 37:862–870. PMID: 24466521.
Article22. Gopalai AA, Senanayake SM, Kiong LC, Gouwanda D. Real-time stability measurement system for postural control. J Bodyw Mov Ther. 2011; 15:453–464. PMID: 21943619.
Article23. Lee SW, Shin DC, Song CH. The effects of visual feedback training on sitting balance ability and visual perception of patients with chronic stroke. J Phys Ther Sci. 2013; 25:635–639. PMID: 24259819.
Article24. French B, Thomas L, Leathley M, Sutton C, McAdam J, Forster A, et al. Does repetitive task training improve functional activity after stroke? A Cochrane systematic review and meta-analysis. J Rehabil Med. 2010; 42:9–14. PMID: 20111838.
Article25. Wevers L, van de Port I, Vermue M, Mead G, Kwakkel G. Effects of task-oriented circuit class training on walking competency after stroke: a systematic review. Stroke. 2009; 40:2450–2459. PMID: 19461035.26. Bensoussan L, Viton JM, Schieppati M, Collado H, Milhe de, Mesure S, et al. Changes in postural control in hemiplegic patients after stroke performing a dual task. Arch Phys Med Rehabil. 2007; 88:1009–1015. PMID: 17678663.
Article27. Marshall SC, Grinnell D, Heisel B, Newall A, Hunt L. Attentional deficits in stroke patients: a visual dual task experiment. Arch Phys Med Rehabil. 1997; 78:7–12. PMID: 9014950.
Article28. Ben-Yishay Y, Piasetsky EB, Rattok J. A systematic method for ameliorating disorders in basic attention. In : Meier M, Benton A, Diller L, editors. Neuropsychological rehabilitation. New York: Guilford Press;1987. p. 165–181.29. Lee SJ, Chun MH, Han EY, Lee JA. The correlation between postural control and attention during performance of dual task in stroke patients. J Korean Acad Rehabil Med. 2010; 34:20–26.30. Hyndman D, Ashburn A. People with stroke living in the community: attention deficits, balance, ADL ability and falls. Disabil Rehabil. 2003; 25:817–822. PMID: 12851091.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effectiveness of Goal-Oriented Dual Task Proprioceptive Training in Subacute Stroke: A Retrospective Observational Study
- Dual-Task Training Effect on Cognitive and Body Function, β-amyloid Levels in Alzheimer’s Dementia Patients: A Randomized Controlled Trial
- Dual Task Training Effects on Upper Extremity Functions and Performance of Daily Activities of Chronic Stroke Patients
- The Effects of Additional Balance Training in Subacute Hemiplegic Stroke Patients
- Effects of activities of daily living-based dual-task training on upper extremity function, cognitive function, and quality of life in stroke patients