Ann Rehabil Med.
2011 Jun;35(3):418-426. 10.5535/arm.2011.35.3.418.
Retrodiscal Approach of Lumbar Epidural Block
- Affiliations
-
- 1Department of Rehabilitation Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul 139-707, Korea. swc328@naver.com
- KMID: 2266863
- DOI: http://doi.org/10.5535/arm.2011.35.3.418
Abstract
OBJECTIVE
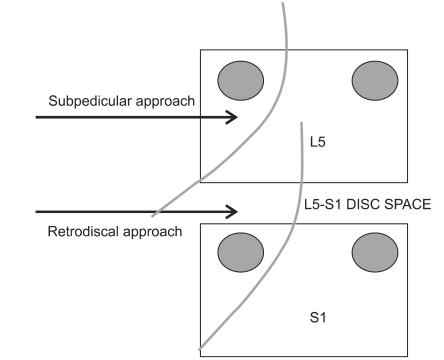
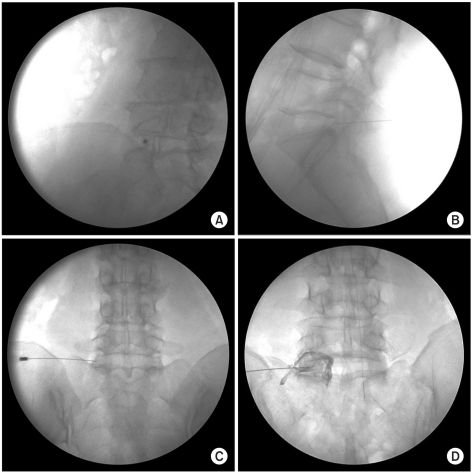
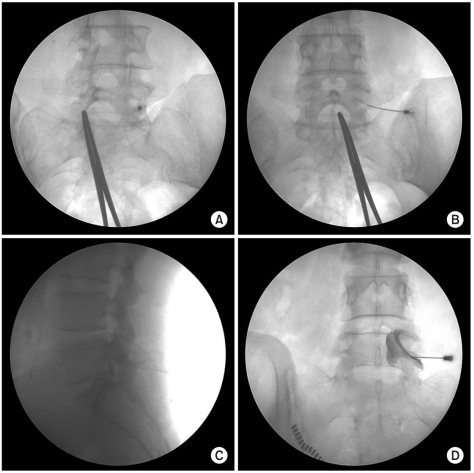
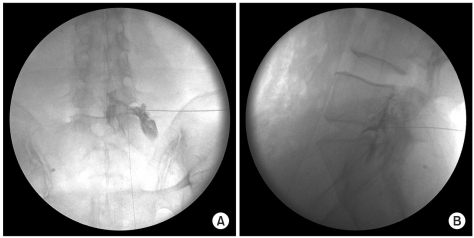
To compare the technical strengths and weaknesses between retrodiscal (RD) and conventional subpedicular (SP) approaches of transforaminal epidural block (TF-EPB). METHOD: Sixty-one patients with L5 radiculopathy who planned to undergo TF-EPB were consecutively enrolled as study subjects. Subjects were randomly assigned to one of two groups. For the RD approach, the positioning of the patient and the C-arm were similar to that for lumbar discography. We compared the pattern of dye spreads, the frequency of complications during the procedures, and the effect of the pain block 2 weeks after the procedure between the two groups.
RESULTS
For the RD group (n=24), the contrast dye diffused around the L5 and S1 nerve roots in 16 cases (67%), but it diffused around only the L5 root in 27 cases (73%) in the SP group (n=37) (p<0.05). Two weeks after the procedure, the visual analogue scale (VAS) decreased by the same amount in both groups (RD group: 3.1+/-1.6, SP group: 3.2+/-2.6). Symptoms of nerve root irritation occurred in 1 case of the RD group and in 10 cases of the SD group (p<0.05).
CONCLUSION
The RD approach was as efficient as the SP approach for temporary diagnostic relief and offered considerable advantages, such as lower nerve root irritation possible lower risk of vascular injection. Thus, it could be a useful technique when a herniated disc segment is stuck or when the foraminal stenosis is severe.
Keyword
Figure
Cited by 1 articles
-
Contrast Spreading Patterns in Retrodiscal Transforaminal Epidural Steroid Injection
Chul Kim, Hee Eun Choi, Seonghoon Kang
Ann Rehabil Med. 2012;36(4):474-479. doi: 10.5535/arm.2012.36.4.474.
Reference
-
1. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Sanelli JT, Freeman ED, Slaten WK, Rao S. Fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil. 2002; 81:898–905. PMID: 12447088.2. Slipman CW, Chow DW. Therapeutic spinal corticosteroid injections for the management of radicu lopathies. Phys Med Rehabil Clin N Am. 2002; 13:697–711. PMID: 12380554.3. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine. 2002; 27:11–16. PMID: 11805628.4. Bogduk N. Clinical anatomy of the lumbar spine and sacrum. 2005. 4th ed. New York: Churchill Living stone;p. 123–124.5. Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J. 2002; 2:70–75. PMID: 14588291.6. Somayaji HS, Saifuddin A, Casey AT, Briggs TW. Spinal cord infarction following therapeutic computed tomography-guided left L2 nerve root injection. Spine (Phila Pa 1976). 2005; 30:E106–E108. PMID: 15706327.
Article7. Stretanski MF, Chopko B. Unintentional vascular uptake in fluoroscopically guided, contrast confirmed spinal injections: a 1-yr clinical experience and discussion of findings. Am J Phys Med Rehabil. 2005; 84:30–35. PMID: 15632486.8. Jasper JF. Lumbar retrodiscal transforaminal injection. Pain Physician. 2007; 10:501–510. PMID: 17525785.
Article9. Lee IS, Kim SH, Lee JW, Hong SH, Choi JY, Kang HS, Song JW, Kwon AK. Comparison of the temporary diagnostic relief of transforaminal epidural ste roid injection approaches: conventional versus posterolateral technique. AJNR Am J Neuroradiol. 2007; 28:204–208. PMID: 17296980.10. Lew HL, Coelho P, Chou LH. Preganglionic approach to transforaminal epidural steroid injections. Am J Phys Med Rehabil. 2004; 83:378. PMID: 15100628.
Article11. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Freeman TL, Slaten WK. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000; 81:1045–1050. PMID: 10943753.
Article12. Sullivan WJ, Willick SE, Chira-Adisai W, Zuhosky J, Tyburski M, Dreyfuss P, Prather H, Press JM. Incidence of intravascular uptake in lumbar spinal injec tion procedures. Spine. 2000; 25:481–486. PMID: 10707395.13. Furman MB, O'Brien EM, Zgleszewski TM. Incidence of intravascular penetrati on in transforaminal lumbosacral epidural steroid injections. Spine. 2000; 25:2628–2632. PMID: 11034648.14. Furman MB, Giovanniello MT, O'Brien EM. Incidence of intravascular penet ration in transforaminal cervical epidural steroid injections. Spine. 2003; 28:21–25. PMID: 12544950.15. Smuck M, Fuller BJ, Yoder B, Huerta J. Incidence of simultaneous epidural and vascular injection during lumbosacral transforaminal epidural injections. Spine J. 2007; 7:79–82. PMID: 17197337.
Article16. Derby R, Lee SH, Kim BJ, Chen Y, Seo KS. Complications following cervical epidural steroid injections by expert interventionalists in 2003. Pain Physician. 2004; 7:445–449. PMID: 16858486.17. Alleyne CH Jr, Cawley CM, Shengelaia GG, Barrow DL. Microsurgical anatomy of the artery of Adamkiewicz and its segmental artery. J Neurosurg. 1998; 89:791–795. PMID: 9817417.
Article18. Burn JM, Langdon L. Lumbar epidural injection for the treatment of chronic sciatica. Rheumatol Phys Med. 1970; 10:368–374. PMID: 5458848.
Article19. Snoek W, Weber H, Jorgensen B. Double blind evaluation of extradural methyl prednisolone for herniated lumbar discs. Acta Orthop Scand. 1977; 48:635–641. PMID: 343479.
Article20. Cohen SP, Maine DN, Shockey SM, Kudchadkar S, Griffith S. Inadvertent disk injection during transforaminal epidural steroid injection: steps for prevention and management. Pain Med. 2008; 9:688–694. PMID: 18657222.
Article21. In : Kim C, Choi HE, Kang SH, Lim MH, editors. The contrast spreading pattern in the retrodiscal approach for transforaminal epidural block. 2010. The 38th Annual Conference of the Korean Academy of Rehabilitation Medicine; 2010 Oct 21-23; Seoul, Korea. Seoul: Medrang.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contrast Spreading Patterns in Retrodiscal Transforaminal Epidural Steroid Injection
- Left Leg Paralysis after Lumbar Epidural Block: A case report
- Pneumocephalus after Interlaminar Lumbar Epidural Block
- Preganglionic Epidural Steroid Injection through Translateral Recess Approach
- Pulsatile subdural contrast image during attempted lumbar transforaminal epidural block: A case report