Ann Rehabil Med.
2014 Oct;38(5):620-627. 10.5535/arm.2014.38.5.620.
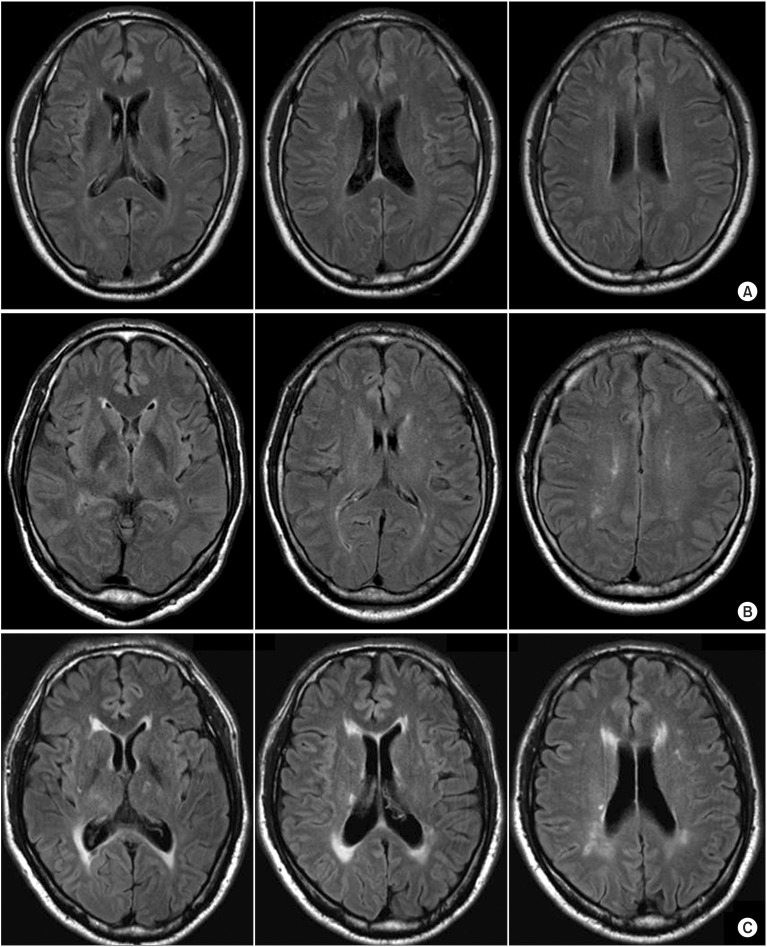
White Matter Hyperintensities and Cognitive Dysfunction in Patients With Infratentorial Stroke
- Affiliations
-
- 1Department of Physical and Rehabilitation Medicine, Center for Prevention and Rehabilitation, Heart Vascular and Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wh.chang@samsung. com
- 2Samsung Advanced Institute for Health Science and Technology, Sungkyunkwan University, Seoul, Korea.
- KMID: 2266496
- DOI: http://doi.org/10.5535/arm.2014.38.5.620
Abstract
OBJECTIVE
To determine whether cognitive function is associated with white matter hyperintensities (WMH) in patients with infratentorial stroke.
METHODS
This was a retrospective, cross-sectional study. Twenty-four first-ever infratentorial stroke patients between 18 and 60 years of age were enrolled. WMH was evaluated by the Fazekas scale and the Scheltens scale. Cognitive functions were assessed using the Korean Mini-Mental Status Examination (K-MMSE), Rey-Osterrieth Complex Figure Test, and the Seoul Computerized Neuropsychological Test Battery (SCNT) at one month after stroke. All participants were divided into two groups based on the presence of WMH (no-WMH group and WMH group). General characteristics and cognitive functions were compared between the groups.
RESULTS
There were no significant differences in general characteristics, such as age, stroke type, hypertension history, and education level between the two groups. However, K-MMSE in the WMH group was significantly lower compared to the no-WMH group (p<0.05). The verbal learning test score in SCNT was significantly higher in the no-WMH group compared to the WMH group (p<0.05). Executive function in the no-WMH group tended to be higher compared to the WMH group.
CONCLUSION
Impairment of cognitive function in patients with infratentorial stroke appeared to be associated with WMH. WMH should be carefully evaluated during rehabilitation of infratentorial stroke patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Kearney-Schwartz A, Rossignol P, Bracard S, Felblinger J, Fay R, Boivin JM, et al. Vascular structure and function is correlated to cognitive performance and white matter hyperintensities in older hypertensive patients with subjective memory complaints. Stroke. 2009; 40:1229–1236. PMID: 19246701.
Article2. Verdelho A, Madureira S, Moleiro C, Ferro JM, Santos CO, Erkinjuntti T, et al. White matter changes and diabetes predict cognitive decline in the elderly: the LADIS study. Neurology. 2010; 75:160–167. PMID: 20625169.3. Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2010; 341:c3666. PMID: 20660506.
Article4. Roman GC, Erkinjuntti T, Wallin A, Pantoni L, Chui HC. Subcortical ischaemic vascular dementia. Lancet Neurol. 2002; 1:426–436. PMID: 12849365.5. Cereda C, Carrera E. Posterior cerebral artery territory infarctions. Front Neurol Neurosci. 2012; 30:128–131. PMID: 22377879.
Article6. Alexander MP, Gillingham S, Schweizer T, Stuss DT. Cognitive impairments due to focal cerebellar injuries in adults. Cortex. 2012; 48:980–990. PMID: 21549360.
Article7. Nys GM, van Zandvoort MJ, de Kort PL, Jansen BP, de Haan EH, Kappelle LJ. Cognitive disorders in acute stroke: prevalence and clinical determinants. Cerebrovasc Dis. 2007; 23:408–416. PMID: 17406110.
Article8. Frank B, Schoch B, Hein-Kropp C, Dimitrova A, Hovel M, Ziegler W, et al. Verb generation in children and adolescents with acute cerebellar lesions. Neuropsychologia. 2007; 45:977–988. PMID: 17030046.
Article9. Mori E, Yamadori A. Acute confusional state and acute agitated delirium: occurrence after infarction in the right middle cerebral artery territory. Arch Neurol. 1987; 44:1139–1143. PMID: 3675246.10. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state": a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12:189–198. PMID: 1202204.11. Somerville J, Tremont G, Stern RA. The Boston Qualitative Scoring System as a measure of executive functioning in Rey-Osterrieth Complex Figure performance. J Clin Exp Neuropsychol. 2000; 22:613–621. PMID: 11094396.
Article12. Kim YH, Shin SH, Park SH, Ko MH. Cognitive assessment for patient with brain injury by computerized neuropsychological test. J Korean Acad Rehabil Med. 2001; 25:209–216.13. Pantoni L, Basile AM, Pracucci G, Asplund K, Bogousslavsky J, Chabriat H, et al. Impact of age-related cerebral white matter changes on the transition to disability: the LADIS study: rationale, design and methodology. Neuroepidemiology. 2005; 24:51–62. PMID: 15459510.14. Scheltens P, Barkhof F, Leys D, Pruvo JP, Nauta JJ, Vermersch P, et al. A semiquantative rating scale for the assessment of signal hyperintensities on magnetic resonance imaging. J Neurol Sci. 1993; 114:7–12. PMID: 8433101.
Article15. Kramer JH, Mungas D, Reed BR, Schuff N, Weiner MW, Miller BL, et al. Forgetting in dementia with and without subcortical lacunes. Clin Neuropsychol. 2004; 18:32–40. PMID: 15595356.
Article16. Kramer JH, Reed BR, Mungas D, Weiner MW, Chui HC. Executive dysfunction in subcortical ischaemic vascular disease. J Neurol Neurosurg Psychiatry. 2002; 72:217–220. PMID: 11796772.
Article17. Galluzzi S, Sheu CF, Zanetti O, Frisoni GB. Distinctive clinical features of mild cognitive impairment with subcortical cerebrovascular disease. Dement Geriatr Cogn Disord. 2005; 19:196–203. PMID: 15677867.
Article18. de Mendonca A, Ribeiro F, Guerreiro M, Palma T, Garcia C. Clinical significance of subcortical vascular disease in patients with mild cognitive impairment. Eur J Neurol. 2005; 12:125–130. PMID: 15679700.
Article19. Schmidtke K, Hull M. Neuropsychological differentiation of small vessel disease, Alzheimer's disease and mixed dementia. J Neurol Sci. 2002; 203-204:17–22. PMID: 12417351.
Article20. Tierney MC, Black SE, Szalai JP, Snow WG, Fisher RH, Nadon G, et al. Recognition memory and verbal fluency differentiate probable Alzheimer disease from subcortical ischemic vascular dementia. Arch Neurol. 2001; 58:1654–1659. PMID: 11594925.
Article21. Pantoni L. Pathophysiology of age-related cerebral white matter changes. Cerebrovasc Dis. 2002; 13(Suppl 2):7–10. PMID: 11901236.
Article22. Pantoni L, Garcia JH. The significance of cerebral white matter abnormalities 100 years after Binswanger's report: a review. Stroke. 1995; 26:1293–1301. PMID: 7604429.23. De Girolami U, Seilhean D, Hauw JJ. Neuropathology of central nervous system arterial syndromes. Part I: the supratentorial circulation. J Neuropathol Exp Neurol. 2009; 68:113–124. PMID: 19151625.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of Low Blood Pressure with White Matter Hyperintensities in Elderly Individuals with Controlled Hypertension
- The Association of Cognitive Dysfunction with White Matter Hyperintensity in Alzheimer's Disease and Mild Cognitive Impairment
- A Correlation Analysis between the Location of White Matter Hyperintensities and Cognitive Functions in Korean Vascular Depression Patients
- Comparison of White Matter Lesions on the Magnetic Resonance Imaging in Major Depression and Vascular Depression
- Association between Cognitive Function, Behavioral and Psychological Symptoms of Dementia and White Matter Hyperintensities in Patients with Alzheimer's Disease and Mild Cognitive Impairment